Introduction
Detection of root fracture is challenging both clinically and radiographically. Root fractures occur in different planes with unpredictable presentations.
Aim
The aim of the study was to evaluate the diagnostic accuracy of selected digital image enhancement tools in the detection of horizontal Root Fracture (RF).
Materials and Methods
Fifty three roots, of single and multi-rooted teeth, in eight dentate human cadaver mandibles were selected for this study. Following minimally traumatic extraction of the teeth, horizontal fractures were induced in 23 roots and remounted in the empty sockets of their respective human dry mandibles. The remaining teeth with no fractures were used as the control group. Twenty two periapical radiographs were obtained by using the paralleling technique and using Complementary Metal Oxide Semiconductor (CMOS). Image J software was used to enhance the original images with the Inversion (IN), Histogram-Equalization (EQ) and Polynomial (Poly) tools. A total of 88 periapical images (original and three enhanced images) were reviewed independently by three Oral and Maxillofacial Radiologists and two Endodontists. Receiver Operating Characteristic (ROC) curve analysis was used to evaluate the accuracy of fracture detection and the kappa statistic was used to assess agreement among reviewers.
Results
The diagnostic accuracy for one of the observers was significantly different in detection of RF with only EQ enhancement tool. Sensitivity and specificity were not significantly different. Interobserver agreement showed no significant difference between imaging methods. Intra-observer agreement was high to moderate.
Conclusion
There was no significant difference between the different imaging modalities. No statistical difference for the agreement was found among or between the endodontists and radiologists in this study.
Digital imaging, Image processing, Periapical radiograph, Polynomial model
Introduction
RF are defined as fractures involving the dentin, cementum and pulp [1]. The prevalence of root fractures in permanent teeth has been reported to be between 0.5% and 7% and commonly occur between the age group of 11-20 years-old [2-4]. RF commonly occur in different planes and are broadly classified as horizontal and vertical. Horizontal RF occur mainly in the anterior teeth of young patients from direct trauma; whereas, vertical RF generally occur in the posterior jaw and are associated with endodontically treated teeth [1,2,5]. Detection of RF is difficult and in most cases it can be only visualized clinically through surgical exploration.
Early detection of the RF is vital to retain affected teeth and prevent extensive damage to the supporting structures [6,7]. The clinical signs and symptoms of RF include pain, tooth mobility, localized swelling, sensitivity to percussion and palpation, sinus tract formation and/or localized periodontal pocket formation [6-10]. Many times the information that is collected clinically is not enough; radiographic findings have to be considered in order to establish the correct diagnosis. Depending on the mechanical vector of trauma, RF can have various presentations. If the root segments are well separated a direct diagnosis can be easily made. If not, then indirect interpretation of radiographic finding is necessary [11]. Radiographic findings such as widening of periodontal ligament space, cervical root resorption, or adjacent bone resorption (such as a “J-shaped” radiographic lesion) have to be considered for final diagnosis [6,7].
Periapical radiography is the first and most common imaging modality used to evaluate RF [12,13]. However, periapical radiography provides a two-dimensional representation of three-dimensional structures, causing superimposition of many structures between the X-ray source and the sensor [14]. In addition, fractures may not be visible if the beam does not pass directly through the fracture line. Therefore, multiple radiographs at different angulations may be necessary [15-17]. However, increasing the number of radiographic images will expose the patient to unnecessary and possibly harmful ionizing radiation. Research has shown that the diagnostic accuracy of digital radiographs is similar to film [15,16]. Digital radiographs have become widely accepted in several fields of dentistry due to the many advantages compared to standard film; such as low-radiation dose, decrease in artifacts due to processing and image enhancement by software [18]. Post-acquisition software image enhancement has been shown to improve diagnostic accuracy of dental lesions [19,20].
The principal objective of image enhancement is to modify an image to make it fit for a given task and specific observer [21,22]. Several enhancement filters have been studied and used clinically in the diagnosis of caries [23-26], endodontic file length [27], peri-implant bone level [28] and periapical lesions [29,30]. Commonly used enhancement filters include IN “reverse-contrast”, EQ, sharpening and coloration. Proper diagnosis of an image is strongly dependent on the contrast of the image. For endodontic purposes, high contrast and high spatial resolution is recommended [31]. Research has shown that our eyes are more sensitive to slight brightness changes located within dark regions of an image, suggesting inverted contrast may be suitable for RF evaluation [32]. A new filter, the poly enhancement tool, converts grey values of an image to equivalent aluminum thickness from a reference stepwedge [33]. Using software enhancement tools in digital imaging can increase the diagnostic accuracy and improve the visibility [18,19].
Few articles have studied the effect of enhancement tools in detection of root fracture [34-36]. This study tests the validity of a poly enhancement filter and compares the diagnostic accuracy between Oral Maxillofacial Radiology Residents and Endodontists in the detection of horizontal RF. The purpose of this study was to compare the diagnostic accuracy of three different digital enhancement tools: IN, EQ and Poly with the original images in the detection of root fractures.
Materials and Methods
This in vitro study was conducted on dry mandibles in the physics laboratory facility of the oral and maxillofacial radiology graduate program in the School of Dentistry of the University of Texas Health Science Center San Antonio (UTHSCSA). Maxillary arches were not used because they could not be separated from their skulls and transported to the physics laboratory and also due to the difficulty to apply the parallel technique on maxillary teeth.
The mandibles were borrowed from the forensic laboratory in UTHSCSA, they were anonymized with unknown age and sex and therefore an expedited approval was granted by the Institutional Review Board (IRB) of the Health Science Center.
Prior to starting the research, a power analysis was conducted; in order to get 80% power with five readers and an expected difference of 0.05 between ROCs of different modalities, a minimum of 45 teeth, equally, or almost equally, divided between fractured and intact, were needed.
Fifty three roots in eight dentate human cadaver mandibles were selected for this study. Teeth included in the study were intact or had small carious lesions. Endodontically treated teeth and fractured teeth were excluded from the research.
Teeth were loosened in their sockets, removed, wrapped with gauze and firmly placed in a bench vise (Craftsman® 51854 4" Bench Vise W/ 180° Swivel, Global Industrial 11 Harbor Park Drive, Port Washington, NY 11050). A small hammer was used to induce the fracture by slowly tapping on the crown [Table/Fig-1]. The fragments were then put back together. Using cyanoacrylate-based fast-acting adhesive (3M™ Scotch-Weld™ Super-Fast Instant Adhesive SF100, 3M. 2115 South Broadway Alexandria, MN 56308), the teeth were placed back in their sockets.
Device used to create the artificial root fractures.
Following a traumatic extraction of the teeth, horizontal fractures were stimulated in 23 roots by applying an external force to the facial aspect of the teeth until a fracture was visible. After fractures were induced, teeth with RF were remounted in the empty sockets of their respective human dry mandibles, with each mandible then containing a combination of fractured (N=23) and non-fractured (N=30) tooth roots. An optical bench was used to provide reproducible radiographic projection geometry including source to object distance and object to receptor distance. An aluminum stepwedge with maximum thickness of 20 mm was placed on the superior part of the CMOS sensor XDR (XDR Radiology Los Angeles, CA). Twenty-two periapical radiographs were obtained by using the paralleling technique. The radiographs were exposed with a Planmeca (Planmeca Oy, Helsinki, Finland) intraoral X-ray machine operating at 60 KVp and 8 mA, with an exposure time of 0.08 second. After obtaining the raw data, Image J (National Institute of Health Bethesda, MD) software and Microsoft Excel were used for image analysis. Image J provided the numerical values of the histograms from the stepwedge and Microsoft Excel provided the regression formulas. All digital images were saved as Tagged Image File Format (TIFF) images.
Image J software was used to enhance the 22 original images with the IN, EQ and Poly tools. Each group was randomly arranged. Images were displayed on a calibrated Dell (Round Rock, TX) 17 inch (.28 dot pitch) high resolution color monitor set at a 16 bit color depth and screen resolution of 1024 x 768 pixels.
Five observers, three OMFR and two board certified Endodontists, each with at least three years of dental experience, evaluated a total of 88 images (22 each of original image, IN, EQ, Poly). Roots were scored on a five-point scale as follows: 1= definitely no fracture present, 2= possibly no fracture present, 3= uncertain, unable to tell, 4= fracture probably present, 5= fracture is definitely present. Observers rated all 53 roots by all three enhancement tools in addition to non-enhanced images on one day (212 decisions per observer) and then rated a randomly selected set of 27 images (6 Original, 7 EQ, 6 IN, 8 Poly; 12 with RF and 15 without RF) on another day two weeks later to provide an opportunity to assess intra-rater agreement. The images were reviewed in a dimly lit room with no windows and conditions remained consistent between sessions.
Statistical Analysis
ROC curve analysis was used to evaluate the accuracy of fracture detection. A score of 3 or higher was considered positive for presence of RF in calculating sensitivity and specificity. Area under the ROC curves, sensitivity and specificity were analyzed using mixed model analysis of variance. The statistical model included the type of image (4 levels: non-enhanced, IN, EQ, Poly) and dentist group (2 levels: OMFR or Endodontist). The level of significance was set at α = 0.05 and the kappa statistic was used to assess agreement among reviewers. All statistical analyses were done with SPSS (version 20.0) software program (IBM Corporation, Armonk, New York, USA).
Results
The kappa analysis for the intra-observer and inter-observer agreement are summarized in [Table/Fig-2,3] The Intra-observer agreement between day 1 and day 2 was high for observers A, B and E and moderate for observers C and D [Table/Fig-2]. The inter-observer agreement varied between combinations of observers [Table/Fig-3]. Agreement between observers B and E was significantly better than C with all other observers and also better than A with B, C, or E. All other observer combinations were statistically the same and agreed within a 0.05 level of statistical significance.
Intra-observer agreement.
| Observer | Observed agreement | Kappa (std error) | Kappa 95% confidence interval |
|---|
| A | 0.852 | 0.695 (0.141) | 0.419 – 0.971 |
| B | 0.852 | 0.700 (0.138) | 0.429 – 0.971 |
| C | 0.815 | 0.634 (0.148) | 0.345 – 0.924 |
| D | 0.778 | 0.550 (0.162) | 0.232 – 0.868 |
| E | 0.889 | 0.776 (0.122) | 0.536 – 1.000 |
Inter-observer agreement.
| Observers | Observed agreement | Kappa (std error) | Kappa 95% confidence interval |
|---|
| A and B | 0.774 | 0.532 (0.059) | 0.415 – 0.648 |
| A and C | 0.731 | 0.460 (0.061) | 0.341 – 0.580 |
| A and D | 0.792 | 0.576 (0.057) | 0.464 – 0.687 |
| A and E | 0.741 | 0.463 (0.062) | 0.341 – 0.585 |
| B and C | 0.731 | 0.451 (0.062) | 0.329 – 0.573 |
| B and D | 0.840 | 0.634 (0.057) | 0.522 – 0.747 |
| B and E | 0.901 | 0.755 (0.051) | 0.655 – 0.854 |
| C and D | 0.759 | 0.512 (0.060) | 0.396 – 0.629 |
| C and E | 0.708 | 0.403 (0.064) | 0.278 – 0.528 |
| D and E | 0.797 | 0.536 (0.063) | 0.412 – 0.660 |
The ratings of all observers of a particular imaging method were combined and compared to the ratings of a different imaging method. The observed agreement and Kappa statistics are shown in [Table/Fig-4]. The values indicate a remarkable amount of agreement among each method, indicating that none of the imaging methods is superior to any other in aiding a dentist to make a decision about root fractures. Inter-observer agreement showed no significant difference between imaging methods.
| Methods | Observed agreement | Kappa (std error) | Kappa 95% confidence interval |
|---|
| BC/EQ | 0.864 | 0.711 (0.045) | 0.623 – 0.799 |
| BC/IN | 0.834 | 0.628 (0.051) | 0.527 – 0.728 |
| BC/Poly | 0.819 | 0.616 (0.050) | 0.518 – 0.715 |
| EQ/IN | 0.842 | 0.661 (0.048) | 0.566 – 0.755 |
| EQ/Poly | 0.849 | 0.687 (0.046) | 0.598 – 0.777 |
| IN/Poly | 0.834 | 0.646 (0.049) | 0.551 – 0.742 |
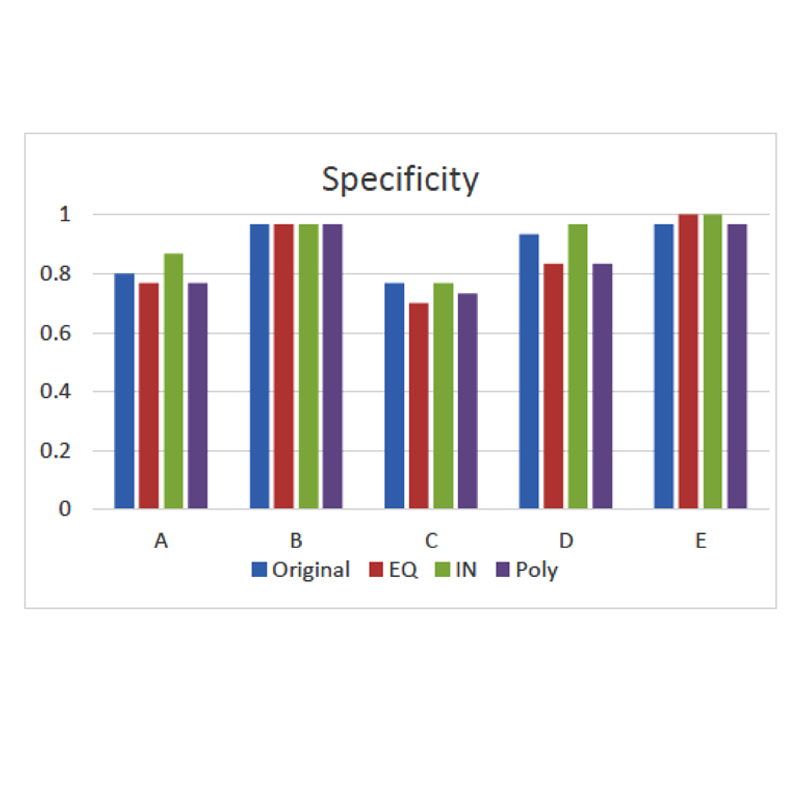
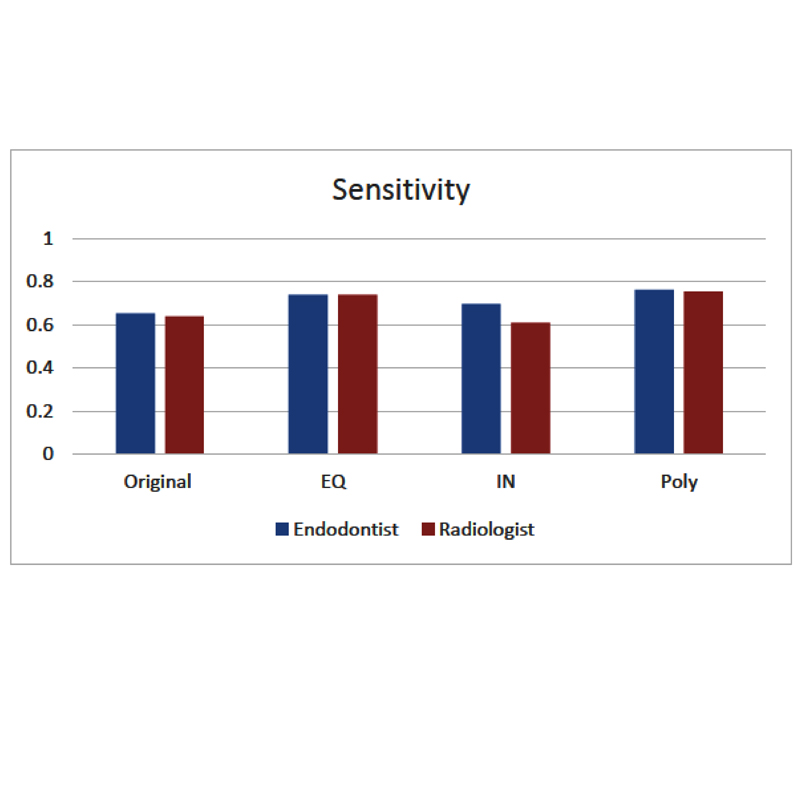
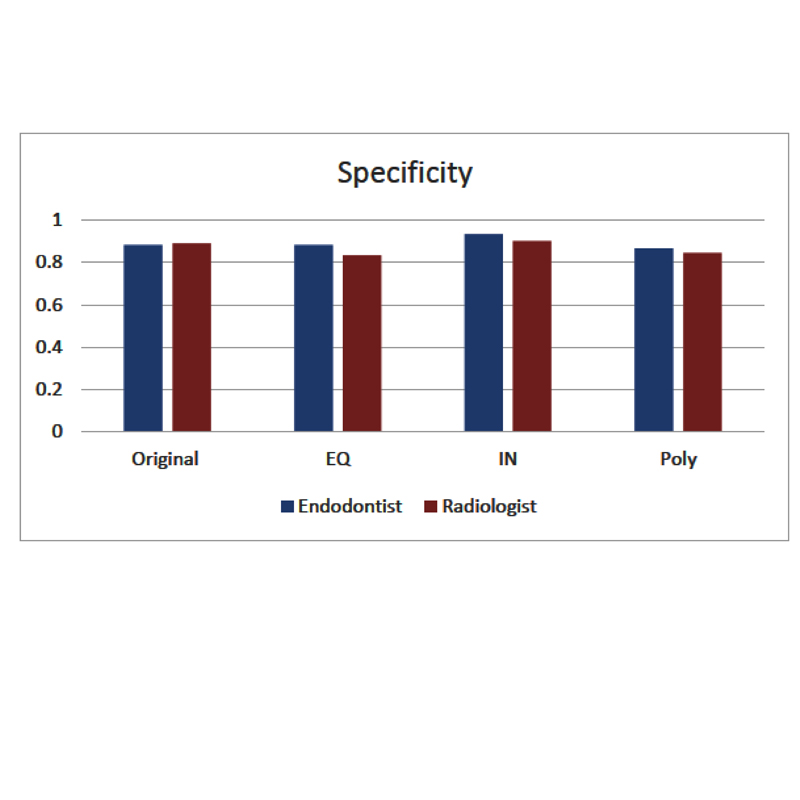
The sensitivity (ability to identify the presence of the disease), specificity (ability to identify the absence of the disease) and accuracy values are presented in [Table/Fig-5,6]. Although, the EQ and Poly enhanced images show slight increases in the sensitivity scores of the observers, there was no significant statistical difference among images. Specificity of the original and IN images showed a slight increase compared with the other modalities; however, there was no significant difference among images.
Accuracy of different imaging modalities.
Specificity of the different methods.
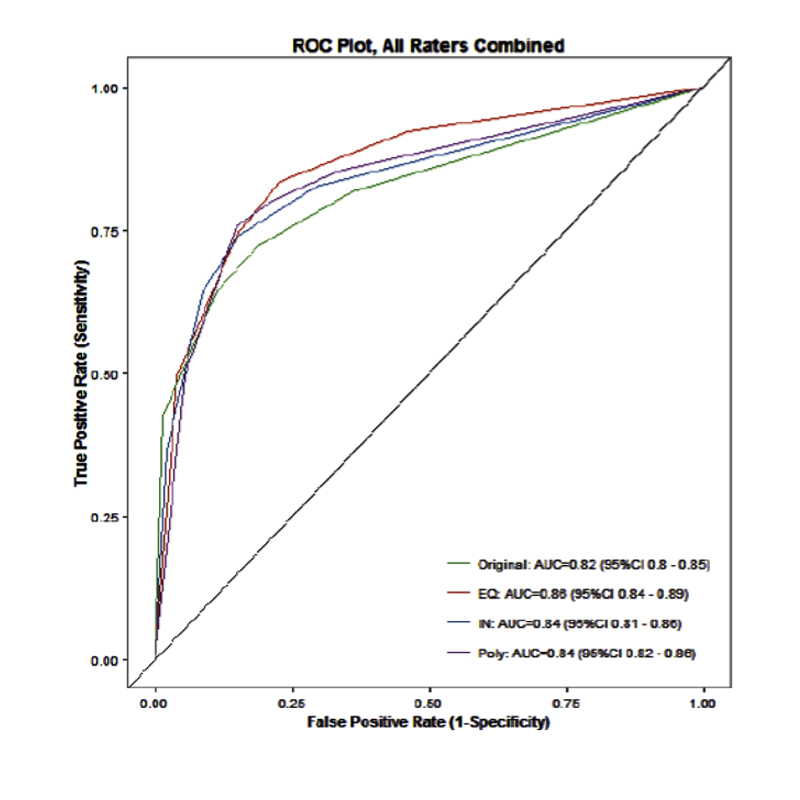
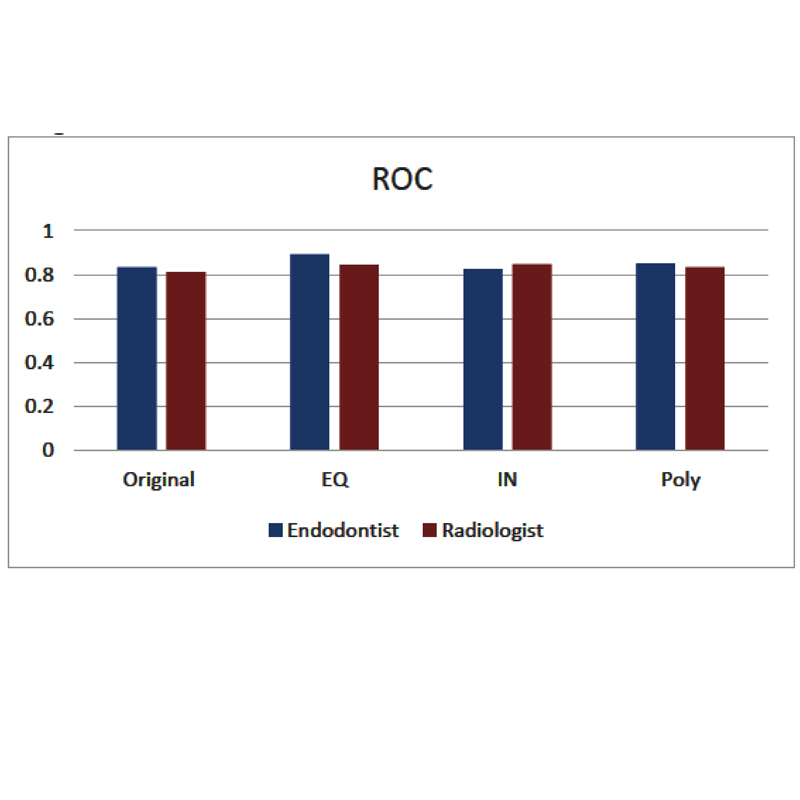
[Table/Fig-7] show area under the ROC curve (Az) for each observer, arranged by the imaging technique. An imaging technique that allows an observer to correctly identify the presence of RF with high confidence on all surfaces would have an Az value of 1.0. However, an imaging technique which resulted in dentists guessing every time (such as a coin flip) would have an Az value of 0.5. The diagnostic accuracy for one of the observers (Observer E) was significantly different in detection of RF with only EQ enhancement tool. However, there was no significant difference between the different imaging modalities.
Area under the ROC curve (Az) for each observer, arranged by imaging technique.
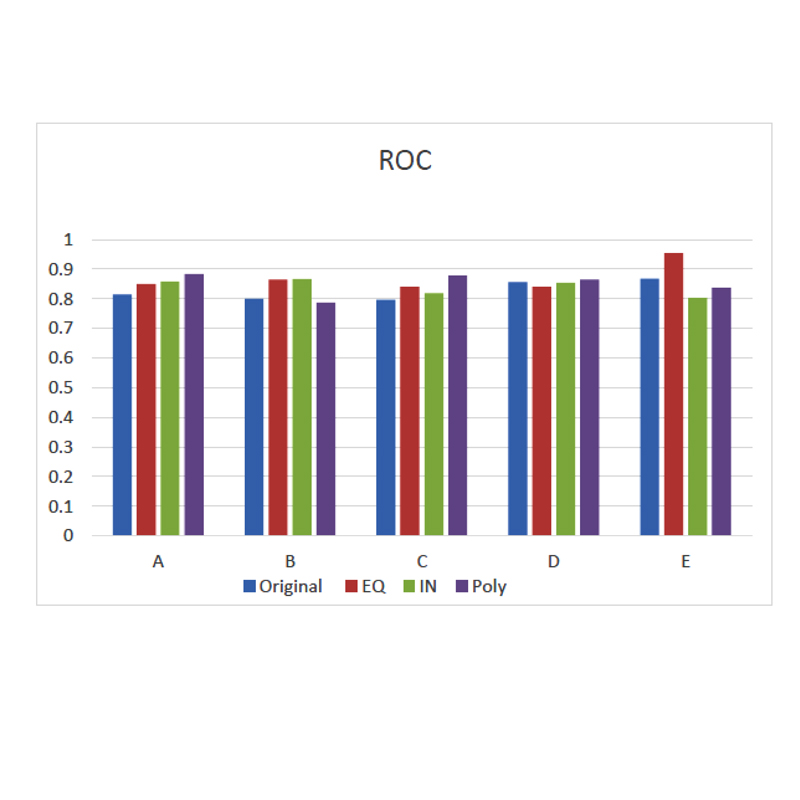
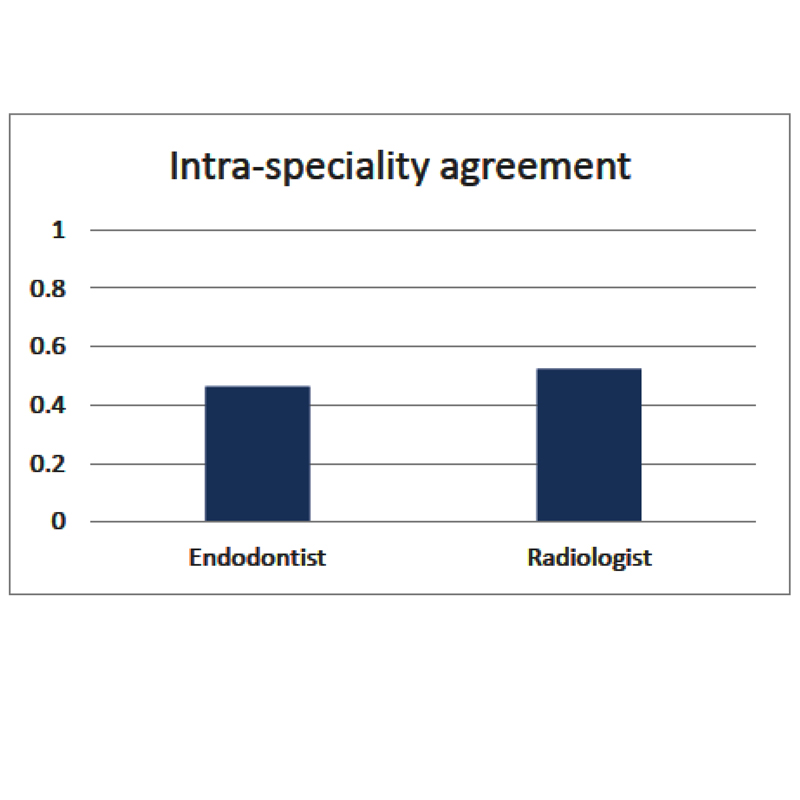
Statistical analysis by specialty group: [Table/Fig-8,9,10,11 and 12] show sensitivity, specificity, ROC, intra-specialty agreement and average agreement between endodontists and radiologists. There was no statistical difference at the 0.05 level of significance for the agreement among or between the endodontists and radiologists in this study.
Sensitivity agreement between endodontists and radiologists.
Specificity agreement between endodontists and radiologists.
ROC agreement between endodontists and radiologists.
Intra-specialty agreement between endodontists and radiologists.
Agreement between endodontists and radiologists.
| Observers | Observed Agreement | Kappa (std error) | Kappa 95% confidence interval |
|---|
| Endo/Radio | 0.784 | 0.537 (0.025) | 0.489 – 0.585 |
Discussion
The main goal of radiology is the production of images with sufficient detail to reveal significant diagnostic information [25]. Post-acquisition enhancements of image display are reported to be advantageous in compensating for visual limitations of the human observer and also for specific diagnostic questions [19,20]. This study compared the use of three methods of digital enhancement tools {reverse-contrast (IN), EQ and Poly} with the original non- enhanced images in the detection of in vitro root fractures by five observers (two endodontists and three OMFR).
Several studies have evaluated the diagnostic accuracy of different imaging enhancement tools in the detection of caries. Studies have shown that there are no statistically significant differences when using enhancement filters in detection of caries [23-26]. Another study found that the noise reduction digital enhancement does not improve the measurement accuracy of the length of the endodontic files [27]. Studies have shown that using imaging enhancement tools does not increase the diagnostic accuracy in detection of peri-implant bone levels [28] or periapical lesions [29, 30].
The results from our study are consistent with earlier studies showing that no significant improvement in diagnostic ability was gained when enhancement tools were used.
Few studies have evaluated the effect of enhancement tools in the diagnosis of root fractures. Kamburoğlu K et al., [34] used a Charged-Coupled Device (CCD) digital system to evaluate vertical root fractures. They did not find significant differences between the sharpness, zoom-in, reverse-contrast and pseudo-3D enhancement functions. Tofangchiha M et al., [35] also used CCD and found that the original image is more accurate than reverse contrast and colorized images in the diagnosis of vertical root fractures. However, a recent study by Nascimento AR et al., [36] used Photo-Stimulable Phosphor (PSP) Digora Optime images instead CCD and showed that the sharpen filter improved the diagnostic accuracy for vertical root fractures in comparison with the original and the other filtered images (3D Emboss, Negative and Shadow). None of the previous studies evaluated the horizontal root fracture or used a CMOS sensor. In the present study, we used a CMOS sensor and we found no significant difference in detection of horizontal root fractures between enhanced images and original images.
Limitation
Further studies need to be done in this subject, using multiple periapical radiographs with different horizontal angulations rather than fixed angulation as used in this study. In a clinical practice situation, multiple radiographs might be needed to evaluate the presence of a root fracture. In addition, observers in this study were not allowed to manipulate the images as they would in clinical practice and none of the observers in this study was a general dentist. The result might be different if the observers had the chance to adjust the images and if general dentists were included. Further in vitro and in vivo studies mimicking clinical conditions are needed to fully evaluate the efficacy of enhancement tools in root fracture detection.
Conclusion
In the present study, there was no significant difference between different enhancement tools in the detection of horizontal root fracture. No statistical difference was found among or between the endodontists and radiologists for the agreement.
[1]. Andreasen JO, Andreasen FM, Andreasen L, Textbook and Color Atlas of Traumatic Injuries to Teeth 2007 4th edOxfordBlackwell Publishing Ltd:337 [Google Scholar]
[2]. Majorana A, Pasini S, Bardellini E, Keller E, Clinical and epidemiological study of traumatic root fracturesDent Traumatol 2002 18:77-80. [Google Scholar]
[3]. Clark SJ, Eleazer P, Management of a horizontal root fracture after previous root canal therapyOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 89:220-23. [Google Scholar]
[4]. Yates JA, Root fractures in permanent teeth: a clinical reviewInt Endod J 1992 25:150-57. [Google Scholar]
[5]. Hovland EJ, Horizontal root fractures: treatment and repairDent Clin North Am 1992 36:509-25. [Google Scholar]
[6]. Tamse A, Kaffe I, Lustig J, Ganor Y, Fuss Z, Radiographic features of vertically fractured endodontically treated mesial roots of mandibular molarsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101(6):797-802. [Google Scholar]
[7]. Tamse A, Fuss Z, Lustig J, Ganor Y, Kaffe I, Radiographic features of vertically fractured, endodontically treated maxillary premolarsOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 88(3):348-52. [Google Scholar]
[8]. Meister F Jr, Lommel TJ, Gerstein H, Diagnosis and possible causes of vertical root fracturesOral Surg Oral Med Oral Pathol 1980 49:243-53. [Google Scholar]
[9]. Testori T, Badino M, Castagnola M, Vertical root fractures in endodontically treated teeth: a clinical survey of 36 casesJ Endod 1993 19:87-90. [Google Scholar]
[10]. Fuss Z, Lustig J, Tamse A, Prevalence of vertical root fractures in extracted endodontically treated teethInt Endod J 1999 32:283-86. [Google Scholar]
[11]. Moule AJ, Kahler B, Diagnosis and management of teeth with vertical root fracturesAust Dent J 1999 44(2):75-87. [Google Scholar]
[12]. Nair MK, Nair UP, Grondahl HG, Wallace JA, Accuracy of tuned aperture computed tomography in the diagnosis of radicular fractures in non-restored maxillary anterior teeth: an in vitro studyDentomaxillofac Radiol 2002 31:299-304. [Google Scholar]
[13]. Mora M, Mol A, Tyndall D, Rivera E, Effect of the number of basis images on the detection of longitudinal tooth fractures using local computed tomographyDentomaxillofac Radiol 2007 36:382-86. [Google Scholar]
[14]. Patel S, Dawood A, Whaites E, Pitt Ford T, New dimensions in endodontic imaging: Part 1. Conventional and alternative radiographic systemsInt Endod J 2009 42:447-62. [Google Scholar]
[15]. Kositbowornchai S, Nuansakul R, Sikram S, Sinahawttana S, Saengmontri S, Root fracture detection: a comparison of direct digital radiography with conventional radiographyDentomaxillofac Radiol 2001 30:106-09. [Google Scholar]
[16]. Tsesis I, Kamburoğlu K, Katz A, Tamse A, Kaffe I, Kfir A, Comparison of digital with conventional radiography in detection of vertical root fractures in endodontically treated maxillary premolars: an ex vivo studyOral Surg Oral Med Oral Pathol Oral Radiol Endod 2008 106:124-28. [Google Scholar]
[17]. Varshosaz M, Tavakoli MA, Mostafavi M, Baghban AA, Comparison of conventional radiography with cone beam computed tomography for detection of vertical root fractures: an in vitro studyInt J Oral Sci 2010 52:593-97. [Google Scholar]
[18]. White SC, Pharoah MJ, The evolution and application of dental maxillofacial imaging modalitiesDent Clin North Am 2008 52:689-705. [Google Scholar]
[19]. Verdonschot EH, Kuijipers TMC, Polder BJ, De Leng-Worm MH, Bronkhorst EM, Effects of digital grey-scale modification on the diagnosis of small approximal carious lesionsJ Dent 1992 20:44-49. [Google Scholar]
[20]. Versteeg CH, Sanderink GC, van der Stelt PF, Efficacy of digital intraoral radiography in clinical dentistryJ Dent 1997 25:215-24. [Google Scholar]
[21]. Analoui M, Radiographic image enhancement. Part I. Spatial domain techniquesDentomaxillofac Radiol 2001 30:01-09. [Google Scholar]
[22]. Mol A, Image processing tools for dental applicationsDent Clin North Am 2000 44:299-318. [Google Scholar]
[23]. Kositbowornchai S, Basiw M, Promwang Y, Moragorn H, Sooksuntisakoonchai N, Accuracy of diagnosing occlusal caries using enhanced digital imagesDentomaxillofac Radiol 2004 33:236-40. [Google Scholar]
[24]. Haiter-Neto F, Pontual AA, Frydenberg M, Wenzel A, Detection of non-cavitated approximal caries lesions in digital images from seven solid-state receptors with particular focus on task-specific enhancement filtersClin Oral Investig 2008 12:217-23. [Google Scholar]
[25]. Zangooei Booshehry M, Davari A, Ardakani F, Nejad MR, Efficacy of application of pseudocolor filters in the detection of interproximal cariesJ Dent Res Dent Clin Dent Prospects 2010 4(3):79-82. [Google Scholar]
[26]. Belém MDF, Ambrosano GMB, Tabchoury CPM, Ferreira-Santos RI, Haiter-Neto F, Performance of digital radiography with enhancement filters for the diagnosis of proximal cariesBrazilian Oral Research 2013 27:245-51. [Google Scholar]
[27]. Mehdizadeh M, Khademi AA, Shokraneh A, Farhadi N, Effect of digital noise reduction on the accuracy of endodontic file length determinationImaging Sci Dent 2013 43(3):185-90. [Google Scholar]
[28]. de Azevedo Vaz SL, Neves FS, Figueiredo EP, Haiter-Neto F, Campos PS, Accuracy of enhancement filters in measuring in vitro peri-implant bone levelClin Oral Implants Res 2013 24:1074-77. [Google Scholar]
[29]. Kullendorff B, Nilsson M, Diagnostic accuracy of direct digital dental radiography for the detection of periapical bone lesions. II. Effects on diagnostic accuracy after application of image processingOral Surg Oral Med Oral Pathol Oral Radiol Endod 1996 82:585-89. [Google Scholar]
[30]. Raitz R, Assuncão Junior JN, Fenyo-Pereira M, Correa L, de Lima LP, Assessment of using digital manipulation tools for diagnosing mandibular radiolucent lesionsDentomaxillofac Radiol 2012 41:203-10. [Google Scholar]
[31]. Schmitd LB, Lima Tde C, Chinellato LE, Bramante CM, Garcia RB, de Moraes IG, Comparison of radiographic measurements obtained with conventional and indirect digital imaging during endodontic treatmentJ Appl Oral Sci 2008 16(2):167-70. [Google Scholar]
[32]. Baxes G, Digital Image Processing: Principles and Applications 1994 John Wiley and Sons, Inc [Google Scholar]
[33]. Geha H, Bechara B, Faddoul T, Noujeim M, A mathematical model relating changes of grey values to changes of thicknesses of a stepwedgeDentomaxillofac Radiol 2013 42(1)50719185 (epub 2012) [Google Scholar]
[34]. Kamburoğlu K, Murat S, Pehlivan SY, The effects of digital image enhancement on the detection of vertical root fractureDent Traumatol 2010 26:47-51. [Google Scholar]
[35]. Tofangchiha M, Bakhshi M, Shariati M, Valizadeh S, Adel M, Sobouti S, Detection of vertical root fractures using digitally enhaced images: reverse-contrast and colorizationDent Traumatol 2012 28:478-82. [Google Scholar]
[36]. Nascimento AR, Ramos ACA, Neves FS, de-Azevedo-Vaz SL, Freitas DQ, The ‘Sharpen’ filter improves the radiographic detection of vertical root fracturesInt Endo J 2015 48:428-34. [Google Scholar]