Propofol, a non opioid intravenous anaesthetic agent, is frequently used as an inducing agent today. The uniqueness of propofol lies in its rapid induction and clear, prompt and refreshing recovery. But such a widely used drug does have some demerits of its own which still remains a considerable concern for anaesthesiologists. Propofol causes pain and discomfort during intravenous injection (i.v.) for induction, in 28%-90% of the patients [1,2].
Propofol, an alkyl phenol compound, is virtually insoluable in aqueous solution. Therefore, it is formulated as emulsion containing 1% (weight/vol) propofol, 10% soya bean oil, 2.25% glycerol and 1.2% purified egg phosphatid [3]. The drug evokes pain on i.v. injection though its pH and osmolality are close to those of blood.
The American anaesthesiogist had ranked pain induced by propofol injection as the seventh most common problem of current clinical anaesthesiology [4]. Various methods both non pharmacological and pharmacological, have been tried for attenuating pain during i.v. injection of propofol. Neither a single agent nor any method is found till date that has 100% efficacy to relieve the pain of the patient.
Non pharmacological methods like injection in a fast running i.v. fluid, injection in a larger vein [5], diluting with 10% intra lipid, cooling propofol to 4°C [6] have been tried with little success.
Amongst pharmacological methods pre-treatment with several agents have been tried like lignocaine, alfentanyl, thiopental, ketamine, dexamethasone etc. Recently ondansetron, a 5HT3 receptor antagonist has been tried and found to be successful in relieving pain during propofol injection, without any adverse effect in significant number of patients [7].
Granisetron, another specific 5HT3 receptor antagonist is now frequently used to prevent post operative nausea and vomiting after general anaesthesia. It was proposed in earlier publications that intravenous administration of granisetron like ondansetron might decrease pain on injection of propofol [8]. This study was planned to compare pretreated analgesic effects of granisetron, lignocaine and placebo after injection of propofol.
Materials and Methods
After obtaining necessary approval from Institutional Ethical Committee a randomized double blinded controlled interventional study was conducted to test the analgesic effect of prophylactic administration of granisetron (1 mg/ml) and lignocaine (1%) as active comparator with placebo or “no treatment” as control on pain induced by injection with propofol in a tertiary care hospital in the Eastern part of India between March 2013 and February 2014. Considering the study population normally distributed with a margin error of 5% and a confidence level of 95% the sample size calculated to be (n=132) using Raosoft® sample size calculator. A total of (n=90) patients could be included within the study period which was evenly distributed into three study groups (n= 30) each.
All patients with ASA physical status I and II aged between 18 and 50 years of either sex admitted for elective surgery under general anaesthesia, were taken into consideration. Patients who refused to participate in the study, having difficulty in communication, history of drug allergy or receiving analgesic within 24 hours prior to surgery were excluded from the study.
Written informed consent was obtained from all patients participating in the study and they were randomly chosen using online random number generator (www.random.org) and were divided into three groups containing (n= 30) patients in each group.
Group I patients (n=30) received injection of intravenous propofol (2.5 mg/kg) one minute after pretreatment with placebo (2 ml of normal saline). Group II patients (n=30) received injection of intravenous propofol (2.5 mg/kg) one minute after pretreatment with 2 ml of 1% lignocaine and Group III patients received injection of intravenous propofol (2.5 mg/kg) one minute after pretreatment with 2 ml of granisetron (1 mg/ml). Pain sensation during injection of intravenous propofol administration was assessed by verbal rating score in all patients.
Meticulous pre-anaesthetic check up was done by thorough physical examination and routine investigations like complete blood count, fasting blood glucose, blood urea, creatinine, ECG and chest skiagram. Procedure of conducting Verbal Rating Score (VRS) during injection was explained and demonstrated to all patients during scheduled pre anaesthetic check up.
In the operation theatre individual body weight of every patient was recorded and then monitors were attached to patients for recording of ECG, SpO2 and Non Invasive Blood Pressure (NIBP). An 18G intravenous cannula was inserted preferably into the dorsum of left hand and lactated Ringers’ solution infusion was started. Procedure of conducting VRS during injection was again explained to the patients.
After pre-oxygenation for three minutes, 2 ml of the drug for pretreatment was given and light pressure was applied on the left mid arm of the patient by an assistant just sufficient to stop the infusion. Thus, the venous drainage at mid arm was occluded manually.
After one minute, the occlusion was released and induction of anaesthesia was done with propofol 2.5 mg/kg. Initial 2 ml propofol was given in bolus and the rest of it was given slowly over 20-30 seconds. A trained and qualified anaesthesiologist, blinded to the allocation of patients in different study group injected the propofol emulsion in a similar fashion for each patient. The injections were delivered through a 3-way cannula attached to the already existing intravenous line that was maintained with a ringer lactate infusion. Time required for the closure of eyes was assessed by the blinded observer. Patients reported pain during injection as none, mild, moderate, or severe (almost intolerable) when asked continuously by the same blinded observer. The patients were blinded too regarding their group allocation.
Pain was graded according to a Verbal Rating Score (VRS-4) [9] bearing 4 points:
0 - No pain
1 - Mild pain (pain reported only in response to questioning without any behavioural sign)
2 - Moderate pain (pain reported in response to questioning and accompanied by a behavioural sign or pain reported spontaneously without any questioning)
3 - Severe pain (strong vocal response accompanied by facial grimacing, arm withdrawal or tears)
Statistical Analysis
The data recording including heart rate, blood pressure and pain during propofol injection were collected by a blinded observer and was later statistically analysed. Continuous variables are expressed as mean±standard deviation and compared across the three groups using One-Way ANOVA and between two groups using unpaired t-test. The statistical software SPSS version 20.0 has been used for the analysis. An alpha level of 5% has been taken, i.e., if any p-value was less than 0.05 it was considered as significant.
Results
A total of (n=90) patients were recruited in the study with no significant difference in respect to age, sex, weight and ASA status (p>0.05) [Table/Fig-1].
Demographic profile of the study participants.
| No of Patients | Age (Years) Mean ± SD | Weight (Kg) Mean ± SD | M : F | ASA Grade I : II |
|---|
| Group I (n=30) | 32.12 ±10.05 | 53.87 ± 10.73 | 08:22 | 18 : 12 |
| Group II (n=30) | 32.08 ± 10.10 | 53.10 ± 10.91 | 06:24 | 21 : 09 |
| Group III (n=30) | 35.38 ±11.82 | 53.03 ± 11.46 | 09:21 | 17 : 13 |
Change in pulse rate was compared between the groups at three time points i.e., pretreatment with the drug, after full dose of propofol and after 10 minutes. It was found that there was a significant difference in pulse rate change between Group I and Group III plus Group II and Group III when compared at pre treatment level and Group I and Group II as well as Group II and Group III when compared after full dose of propofol. Although a statistically non-significant changes in pulse rate was noticed across all the groups when compared after 10 minutes of administration of propofol to the patients [Table/Fig-2].
Comparison of pulse rate differences between groups at different time points.
| Variables | Group I (n=30) Mean ± SD | Group II (n=30) Mean ± SD | Group III (n=30) Mean ± SD | Significance (p-value) |
|---|
| Pretreatment | 0.57 ± 5.79 | 1 ± 7.39 | -3.07 ± 6.54 | 0.393*0.013◊0.013# |
| After full dose propofol | -4.3 ± 10.6 | -9.70 ± 7.69 | -6.3 ± 12.4 | 0.013*0.252◊0.012# |
| After 10 minutes | -3.3 ±13.3 | - 6.6 ± 14.8 | -3.1 ± 16.5 | 0.367*0.959◊0.390# |
Note: Differences in pulse rate value just after pretreatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
p-value between Group I and Group II,
p-value between Group I and Group III
p-value between Group II and Group III
The changes in systolic blood pressure were also compared between the groups after pretreatment with the drug, after full dose of propofol and after 10 minutes and was found that, there was no significant difference between groups at any point of time regarding systolic arterial blood pressure [Table/Fig-3]. Differences in pulse rate as well as systolic/diastolic blood pressure value just after pre treatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
Comparison of systolic arterial blood pressure differences between groups at different time points.
| Variables | Group I (n=30) Mean ± SD | Group II (n=30) Mean ± SD | Group III (n=30) Mean ± SD | Significance (p-value) |
|---|
| Pretreatment | -0.40 ± 3.17 | 0.60 ± 4.27 | 2.30 ± 9.66 | 0.307*0.381#0.151◊ |
| After full dose propofol | -25.3 ± 10.4 | -26.03 ± 6.99 | -28.4 ± 13.6 | 0.750*0.399#0.325◊ |
| After 10 minutes | 5.9 ± 15.5 | 7.4 ± 14.8 | 4.9 ± 19.4 | 0.702*0.826#0.576◊ |
Note: Differences in systolic blood pressure just after pretreatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
p-value between Group I and Group II,
p-value between Group I and Group III
p-value between Group II and Group III
Similarly, change in the diastolic blood pressure was compared between the groups after pretreatment with the drug, after full dose of propofol and after 10 minutes and no significant difference between groups were observed, but diastolic blood pressure significantly decreased than baseline after pretreatment in Group II [Table/Fig-4].
Comparison of diastolic arterial blood pressure differences between groups at different time points.
| Variables | Group I (n=30) Mean ± SD | Group II (n=30) Mean ± SD | Group III (n=30) Mean ± SD | Signifi- cance (p-value) |
|---|
| Pretreatment | 0.50 ± 3.72 | -1.10 ± 3.32 | -1.60 ± 8.09 | 0.04*0.622#0.101◊ |
| After full dose propofol | -13.63 ± 6.56 | -13.60 ± 6.16 | -13.97 ± 9.81 | 0.492*0.561#0.431◊ |
| After 10 minutes | 1.3 ± 10.0 | 0.9 ± 12.1 | 4.8 ±10.6 | 0.889*0.193#0.189◊ |
Note: Differences in diastolic blood pressure just after pretreatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
p-value between Group I and Group II,
p-value between Group I and Group III
p-value between Group II and Group III
According to verbal assessment score for pain, it was found that there was a significant lesser pain perception in the Group II and III patients when compared to Group I, i.e., placebo group [Table/Fig-5,6].
Comparison of pain perception according to Verbal Rating Score (VRS-4) among the patients of different groups.
| Pain score | Group I (n=30) | Group II (n=30) | Group III(n=30) | Significance p-value |
|---|
| No pain | 3 | 27 | 25 | <0.05*>0.05# |
| Mild pain | 11 | 3 | 4 | >0.05# |
| Moderate pain | 13 | 0 | 0 | <0.05* |
| Severe pain | 3 | 0 | 1 | <0.05* |
p-value between Group I and Group II & III,
p-value between Group II and Group III
Comparison of pain perception among the patients of different groups. Gr=Group
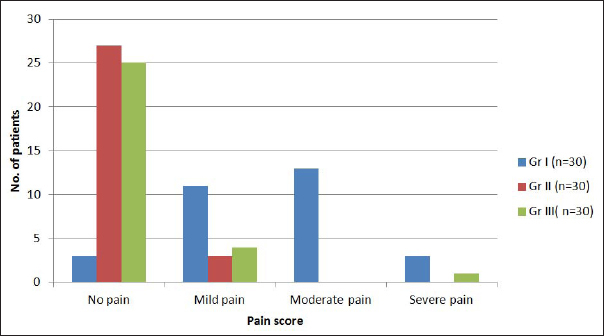
On the other side when Group II i.e., lignocaine compared with Group III i.e., granisetron [Table/Fig-5] there was no statistically significant difference observed regarding pain reduction following administration of propofol while calculating using one-way ANOVA with Tukey’s post-hoc test.
Discussion
Propofol has earned enormous popularity as an intravenous induction agent especially in day care surgery due to its prompt recovery. Yet the pain during injection is an annoying problem with the patients. When injected in a vein on the dorsum of the hand the incidence of pain has been reported to be 28%-90% [1,2] in adults. When a larger (wider) proximal vein is chosen for the injection the possibility of pain varies from 0%-30% [5].
In the present study, 90 patients were randomly divided into three groups which showed that there was no pain on injection of propofol in three patients in the placebo group while 27 out of 30 patients in the lignocaine pretreatment group. This is in conformity with the earlier finding of Nathanson MH et al., who found that lignocaine pretreatment was very effective to attenuate propofol injection pain [10].
So far as the granisetron pretreatment group (III) patients were concerned there was no pain on injection of propofol in 25 out of 30 patients. This finding was similar to the finding of Ambesh SP et al., [7].
Ambesh SP et al., following a double blind controlled study observed that incidence of pain following propofol were only 25% following ondansetron pretreatment while it was 55% after the placebo [7]. The result was statistically significant (p<0.05). Since ondansetron and granisetron both are 5HT3 receptor antagonist there is possibility of existence of class effect which was reflected in the result of our study similar to that of Ambesh SP et al., [7].
In the present study, there was no statistically significant difference in preventing pain of propofol injection between lignocaine (group-II) and granisetron (group-III) pretreatment groups, which again re establishes the findings of Ambesh SP et al., where ondansetron was used [7].
Singh DK et al., in another study considering pretreatment with various drugs (magnesium sulfate, granisetron, nitroglycerine and a placebo) consisting 25 patients in each group observed that granisetron was the most effective drug (incidence of pain was only 40%) amongst all the three drugs which was statistically significant [11].
Dubey PK and Prasad SS in a comparative study amongst three groups (each group had 50 patients) using normal saline, lignocaine and granisetron as pretreatment to prevent propofol pain observed that both lignocaine and granisetron significantly reduced the incidence of pain more than the placebo (p<0.01) [8]. However, they preferred granisetron over the other comparator as it had an additional benefit of preventing postoperative nausea and vomiting similar to our present study.
Ahmed A et al., compared the effect of granisetron pretreatment with that normal saline in preventing pain of propofol injection and observed that only 15% patients of granisetron group complained of pain which was also statistically significant (p<0.05) [12]. They further observed that the severity of pain was much less (2.5% compared to 37.5%). They also concluded that granisetron has additional benefit of preventing emetogenic sequelae of anaesthesia similar to findings of Dubey PK and Prasad SS and the present study [8].
Regarding haemodynamic parameters in this study there was no significant difference in pulse rate between groups at 10 minutes after propofol administration. After full dose of propofol there was significant fall in pulse rate in granisetron group (Group III) when compared with the lignocaine group (Group II). This indicates that lignocaine as pretreatment medication was more effective than granisetron to maintain at 5% level of significance. The difference in pulse rate between lignocaine and granisetron was significant after pretreatment and after full dose of propofol and not after 10 minutes of injection.
There was no significant change in systolic blood pressure between the three groups at any point of study. The change in diastolic blood pressure was not significant either when compared between placebo (Group I) and granisetron (Group III) or lignocaine (Group II) with granisetron.
Following a critical analysis of the various earlier studies made by Ambesh SP et al., Dubey PK and Prasad SS, Singh DK et al., Ahmed A et al., it can be commented that they corroborates the present study proving granisetron, a very effective drug in preventing pain of propofol injection [7,8,11,12].
Limitation
The study was conducted in a small sample of patients due to time constrain since it was done as a research work of dissertation, who were pre admitted, pre planned for operative indications in a single tertiary care hospital. Emergency cases were not included in our study. Neither the paediatric or geriatric age group patients nor the pregnancy related cases were assessed in this study.
Conclusion
It can be concluded that intravenous granisetron can effectively reduce the injection pain of intravenous propofol, and comparable with that of lignocaine. There is no significant difference in pain reduction or haemodynamic changes between the two drugs according to the present study.
The additional established benefit of granisetron being a longer acting antiemetic might be more preferable as it has an extra advantage over lignocaine as a pre anaesthetic medication to prevent nausea and vomiting along with attenuation of injection pain of intravenous propofol as found in the present study. Hence further more multicentric controlled studies are required in future to generate reliable data to establish our hypothesis.
Note: Differences in pulse rate value just after pretreatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
*p-value between Group I and Group II,
◊p-value between Group I and Group III
#p-value between Group II and Group III
Note: Differences in systolic blood pressure just after pretreatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
*p-value between Group I and Group II,
#p-value between Group I and Group III
◊p-value between Group II and Group III
Note: Differences in diastolic blood pressure just after pretreatment in Group I, Group II and Group III was ascertained by comparing baseline parameters of patient to stated time.
*p-value between Group I and Group II,
#p-value between Group I and Group III
◊p-value between Group II and Group III
*p-value between Group I and Group II & III,
#p-value between Group II and Group III