Measles is a respiratory infection usually affecting children under-five years of age. It contributes to significant childhood morbidity and mortality globally. According to WHO 2012 global report; 2, 27, 245 cases of measles were reported with 18 deaths every hour [1].
In the year 2013, many outbreaks of measles were reported around the world, most notable being Swansea (UK) which affected 1400 children and Northern England with 1000 cases. Europe has been experiencing frequent outbreaks since 2011 mostly in France, Ukraine and Romania [2].
Many developing countries like Afghanistan, Pakistan and Syria have had challenges in their health sectors due to increase in outbreaks with cases ranging from thousands to lakhs resulting in significant mortality [2].
World Health Organisation (WHO) global estimate for the year 2013 suggested mortality due to measles as high as 0.14 million with India accounting for 50% of those cases [3]. The year 2005 saw about eight outbreaks in India in four states viz., Uttaranchal, West Bengal, Tamil Nadu and Himachal Pradesh accounting for a total of 432 cases [4].
During pre-vaccination era, the disease was endemic in India with epidemics reported once every 2–3 years and over 90% of the children being affected before they reached 15 years of age [5].
Measles is predominantly seen in infants and young children in the population with low vaccine coverage and herd immunity as low as 10%. An increase in the vaccine coverage results in the age shift in the occurrence of measles to older children, adolescents and adults [6].
The latest report available on vaccine coverage in Udupi district of India suggests coverage of 97.4% [7], which is the highest in Karnataka state and Manipal being an educational hub, caters to students from various regions of the country and abroad. This high coverage of vaccination in the indigenous population and admix of student from various parts makes the situation conducive for an impending outbreak. A study conducted among health sciences students in the same region as the present study found the prevalence of 9.5% among them in the year 2013 [8].
An outbreak of fever with maculo-papular rash occurred among adolescents residing in Manipal. An outbreak investigation was therefore taken up to define it in terms of person, place and time and estimate the attack rates, case fatality rate and vaccine efficacy.
Materials and Methods
This outbreak investigation was conducted in Manipal; a small university town situated in Udupi district, Karnataka, India. This place is home to a student population 28,000 coming from various parts of India and abroad, studying in 29 institutions and departments attached to the university spread over an area of 26 km2.
The outbreak was reported in four hostels blocks of Manipal Institute of Technology (MIT) and one hostel block of Kasturba Medical College (KMC). Apart from the hostels, one case was residing in a nearby apartment as well.
Confirmation of outbreak: Standard measles outbreak investigation formats by WHO was used for collecting data [9]. Outbreak was defined by WHO as five or more suspect cases of measles in a block in a week or any death due to measles in a block in a week or five or more suspect cases in an area bordering several blocks [10]. In the present scenario, first criterion was satisfied.
Constitution of Rapid Response Team (RRT): An emergency rapid response team consisting of eleven members, comprising of government health authorities and postgraduates of community medicine of Manipal University was constituted, oriented and trained for the investigation.
Case definition: To ensure uniformity during investigation, the following definitions were adopted from WHO’s recommended standards for surveillance of selected vaccine-preventable diseases [11]. Clinical Measles - Any person with fever and maculo-papular rash (i.e., non-vesicular or without fluid), with cough or coryza (running nose) or conjunctivitis (red eyes) during last three months. Laboratory confirmed measles – A case that meets the clinical case definition and presence of measles specific IgM antibodies in the serum. Epidemiologically confirmed measles – A case that meets the clinical case definition and is linked epidemiologically to a laboratory confirmed case.
Vaccination status and coverage: The vaccination status of cases was verified by direct interview, telephonic interview of parents and immunization card (if available). All possible efforts were made to obtain the information regarding vaccination against measles. In spite of exhaustive efforts, if the information was not obtained, those cases were classified as “unknown”.
Laboratory testing: The blood samples collected were subjected to IgM Enzyme Linked Immuno Sorbent Assay (ELISA) and Polymerase Chain Reaction (PCR) for confirmation at Manipal Centre for Virus Research (MCVR), Manipal. Lab confirmed (MCVR, Manipal) serum samples were sent to National Institute of Virology (NIV) Bengaluru unit for cross verification along with one serum and one urine sample.
Investigation and outbreak control: A line list of laboratory confirmed cases of measles was prepared and approached. The Emergency Rapid Response Team was divided into five groups to carry out an active search in the neighbourhood of the cases. Students residing in the same hostel as the confirmed cases, residents in the staff quarters adjacent to the hostels of both the institutions and the residents of the apartment where one of the cases was reported were approached to search for new and suspect cases. They were explained the purpose of the visit and interviewed regarding the symptoms suggestive of measles (as per the case definition) among members residing in the household. They were also provided with contact information of the members of the rapid response team to obtain information regarding new (incubating) cases in the future.
Blood specimens were collected from newly detected cases and were provided with two doses of Vitamin A supplementation. The suspected cases were isolated in a room and were provided with all the necessities. A team of doctors visited the isolated students for follow up and check for progression and development of complications. The housekeeping staff and caretakers were also interviewed during population survey and were requested to report new cases of fever with rash to the concerned nodal persons.
Meeting was convened with doctors of Kasturba Medical College, Manipal and wardens of the respective hostels to update them with the situation and seek their co-operation. In order to facilitate passive surveillance, student clinics were set up in the MIT and KMC hostel campus functional from 9.00 AM to 6.00 PM. From 6.00 PM to 9.00 AM students were asked to report to the casualty of Kasturba hospital or call the nodal persons. Information, Education and Communication (IEC) material was displayed at prominent places in the university campus to raise awareness about measles and provide contact details in case of emergency. New cases reported from outside the campus were admitted in the isolation ward of Kasturba Hospital. The emergency rapid response team met regularly at District Surveillance Unit, Udupi to discuss the progress and report newly detected confirmed and suspected cases.
Statistical Analysis
The obtained data was analysed using Microsoft office excel 2010. Results were expressed as proportions; attack rates and vaccine efficacy were calculated. Proportions were compared using Chi-square test with Fisher’s-Exact correction.
Results
The outbreak investigation conducted for a period of three months (November 2013 – January 2014) reported a total of 20 laboratory confirmed cases of measles. Following the report of the first case on 21st November 2013 and confirmation of an epidemic in the 2nd week of December 2013, 540 possible contacts were investigated to search for hidden and incubating cases. A total of 480 subjects were screened from the hostel, 33 from the surrounding staff quarters and 27 from the surrounding flats in the apartment of the confirmed cases. Blood samples were obtained from all the suspected/clinically confirmed cases with no refusal.
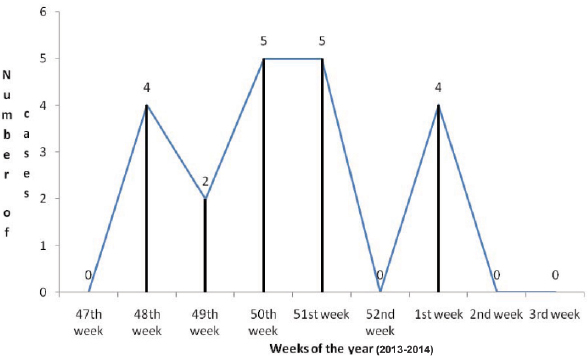
Descriptive epidemiology: The Integrated Disease Surveillance Project office (IDSP) received report of four cases of laboratory confirmed measles from the hostels of MIT in the 48th week of the year 2013 followed by two cases from the same institution in the 49th week. Five cases were reported from KMC hostels in the 50th week confirming the presence of an outbreak. Following that, an outbreak investigation was carried out among 540 people residing in the same hostel and apartment as the cases. During the investigation, five cases came to the notice of the health authorities in the 51st week. No cases were reported in the 52nd week. But four new confirmed cases were reported in the 1st week of 2014. Thereafter no cases were found for the next two weeks (duration longer than the longest incubation period of the disease) [9] bringing the investigation to an end. This outbreak saw a total of 20 laboratory confirmed cases of measles over a period of two months. This was depicted in the form of an epidemic curve [Table/Fig-1] which showed a peak after two weeks of the index case. There was another small increase in cases from 29th December 2013 to 4th January 2014, following which no further cases were seen for another two weeks.
Epidemic curve of the measles outbreak (n=20).
The age distribution of the cases ranged from 16 years to 30 years with most of them in the age group of 16-20 years (50%).
Males (70%) were more affected than females (30%).
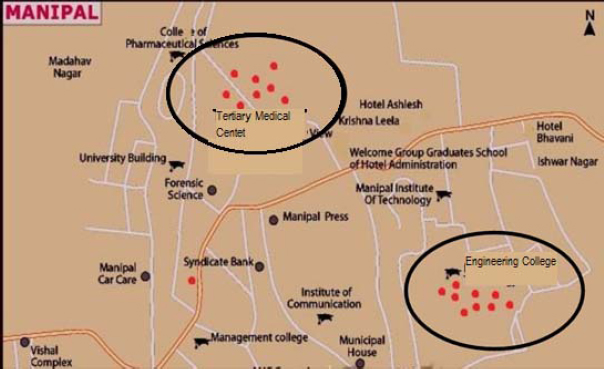
There was a clustering of cases seen in two areas namely staff Quarters and hostels around Kasturba Medical College and Manipal Institute of technology as seen in the spot map [Table/Fig-2].
Spot map showing clustering of cases in outbreak (n=20).
There were no deaths reported among the cases.
Vaccination status and coverage: Among the population surveyed including the confirmed cases [11], 398 were vaccinated with a single dose of measles, 45 of them were not vaccinated and 108 were unaware of their vaccination status.
Attack rate and vaccine efficacy: The overall attack rate was 3.5%. Attack rate was high in the age group of 16-20 years. No cases were seen among less than 15 years of age and more than 30 years of age.
It was found that the Attack Rate among Unvaccinated (ARU) was 7.8% and that of vaccinated was 2.01% giving a vaccine efficacy of 74.8% [Table/Fig-3,4].
Age and gender distribution cases during measles outbreak (n=20).
| Age groups (Years) | Males (%) | Females (%) |
|---|
| 16-20 | 9(64.3) | 1(16.7) |
| 21-25 | 5(35.7) | 4 (66.6) |
| 26-30 | 0(0) | 1(16.7) |
| Total | 14 (70) | 6 (30) |
Age specific attack rates in outbreak (n = 551).
| Age Group(Years) | Total no. of cases in the age group (a) | Total population surveyed in the age group (B) | Age specific attack rate (%) A/(A+B) x 100 |
|---|
| ≤15 | 0 | 16 | 0 |
| 16-20 | 10 | 172 | 5.49 |
| 21-25 | 9 | 261 | 3.33 |
| 26-30 | 1 | 33 | 2.94 |
| ≥31 | 0 | 69 | 0 |
| Total | 20 | 551 | 3.5 |
Laboratory findings: A total of 34 blood samples were obtained from suspected cases of measles and 20 were confirmed by laboratory diagnosis and 14 were negative.
Outbreak control: Following the isolation of cases during the investigation, there was a reduction in the number of cases and increased Information, Education and Communication (IEC) regarding the disease ensured that the students took precautions to prevent contracting it. The strict implementation of the control measures and constant vigil by the investigators, active and passive surveillance ensured no cases occurred after the first week of January 2014. The confirmed cases of measles were given two doses of Vitamin A supplementation and adequate nutrition was ensured at the place of isolation thereby helping them recover faster and prevent complications and death.
Discussion
Measles is a disease of childhood predominantly seen in the age group of six months to three years, but the present study found that among the total of 20 laboratory confirmed cases, the age group affected was 16-29 years similar to the findings of Ehresmann KR et al., [12] (20–29 years, Minnesota; 2004) and most other studies reported the outbreak in an age group of less than 15 years [4,13-17], showing a higher age group of incidence of the disease in the region. This may be attributed to either non-vaccination or reduction in the level of protective antibodies. Among the cases detected, only four (20%) received a single dose of vaccine against measles during childhood and 16 (80%) were either unaware of their vaccination status or unvaccinated which may be one of the reasons for the outbreak.
A gender-wise analysis revealed males were predominantly affected than females. These findings were similar to that of Gupta SN et al., (Himachal Pradesh; 2009) [16], but in Patro BK et al., (Chandigarh; 2012) study [15], females were more commonly affected than males revealing that the disease has no gender specificity. The higher number of males being affected can be due to the outbreak occurring in the hostels.
The current epidemic started in November and lasted for six weeks. Peak of the epidemic was seen after two weeks of index case reporting. Mishra A et al., (Madhya Pradesh; 2009) reported two outbreaks in their study with the first being detected in January [14], lasting for two weeks and second in March, lasting for six weeks, reinforcing the seasonal trend of measles.
This study determined an overall attack rate of 3.5%, with the highest rate (5.49%) seen in the age group of 16-20 years and least (2.94) in 26-30 years. This was lower than the rates found in the investigations conducted by Murhekar MV et al. (33% and 46%), Mishra A et al., (6.2%), Gupta SN et al., (11%), and Bhuniya S et al., (14%) [4,14,16,17]. The lower rates may be due to the good environmental conditions and prompt investigation and containment.
The Attack Rate Among Unvaccinated (ARU) was 7.8% and that of vaccinated was 2.01% but Bhuniya S et al., found a 30% attack rate among vaccinated and 89% among unvaccinated, higher than the results obtained in the present study [17].
A vaccine efficacy of 74.8% was obtained in this study lesser than that obtained by Gupta SN et al., (82%) [16]. whereas a lower efficacy was found by Mishra A et al., (47.3%) and Bhuniya S et al., [17] (66.3%) [14,17].
There were no deaths due to measles in the current study. Studies conducted by Mishra PP et al., reported one death [13], Murhekar MV et al., reported six deaths (CFR – 1.5%) [4], Pomerai KW et al., had five deaths (CFR – 4%) [18] and Mishra A et al., reported 14 deaths (CFR – 6.2%) [14]. This may be attributed to the immediate medical attention and Vitamin A prophylaxis provided to the cases.
Government of India introduced the second dose of measles vaccination at age of one and half years in the year 2010. Measles, Mumps and Rubella (MMR) has been provided as an optional vaccine according to Universal Immunization Programme and routine immunization according to Indian Academy of Paediatrics (IAP) schedule. The information regarding the receipt of MMR is lacking among the cases. The subjects in the current study could not have received the second dose of measles. The new born children are now being provided with the second dose which is helping to enhance the protective antibody levels whereas those in the higher age group have weaning antibody levels making them prone for an attack of measles.
This trend shows that a high vaccine coverage in the young pushes the age of incidence of measles to the older generation, as evidenced by the increase in the number of outbreaks in the adolescents.
Limitation
The serological assay to determine the antibody level in the participants could not be assessed.
Conclusion
This outbreak investigation revealed occurrence of measles in the higher age group due to either non-vaccination or the reduction in the immune-status over time. Thus, warranting a need for a booster dose in the adolescent age group to increase their immunity.