Introduction
The association between psychological factors and non-ulcer dyspepsia remains controversial.
Aim
To determine the prevalence of Helicobacter pylori (HP) and Stress/Anxiety/Depression (SAD) in patients with Functional Dyspepsia (FD) and assess the outcome at three months after appropriate intervention.
Materials and Methods
This prospective non-randomized interventional study was conducted on 120 patients with FD. Initial workup included upper gastrointestinal endoscopy to confirm HP infection with either of two tests, the urease test or histopathology. Patient Health Questionnaire-9 scale (PHQ-9) was used to assess depression, General Anxiety Disorder-7 scale (GAD-7) for anxiety and Perceived Stress Scale (PSS) for stress. Patients were considered positive when they had significant scores on one or more of the questionnaires (SAD+).
The subjects were then classified into four groups: Group A (positive for HP and SAD, n=35), Group B (positive for HP and negative for SAD, n=31), Group C (negative for HP and positive for SAD, n=33) and Group D (negative for HP and SAD, n=21). The groups were then treated as follows: Group A: HP eradication plus psychiatric intervention, Group B: HP eradication alone, Group C: psychiatric intervention alone and Group D: proton pump inhibitors.
Modified Glasgow Dyspepsia Symptom Score (Mod. GDSS) was used to assess the severity of dyspepsia at baseline and to monitor the change in score over three months.
Statistical analysis was done using the Statistical Package for the Social Sciences version 16.0. Non-parametric data like proportions of response in different groups to treatment was analysed using the Chi square test and quantitative data using ANOVA. Gender wise distribution and response to treatment was calculated using the z-test and unpaired t-test.
Results
Overall 120 patients were recruited across four groups. A 55% of the subjects were positive for HP and 56.7% for SAD and 29.2% for both. In all three groups with psychiatric comorbidity, females exceeded males in a proportion of 3:1.
Mod. GDSS was not significantly different at baseline between HP+ and HP- patients (p=0.1278) except when HP positivity was also associated with SAD (p<0.001), whereas SAD positivity alone significantly increased the baseline Mod. GDSS (p=0.006).
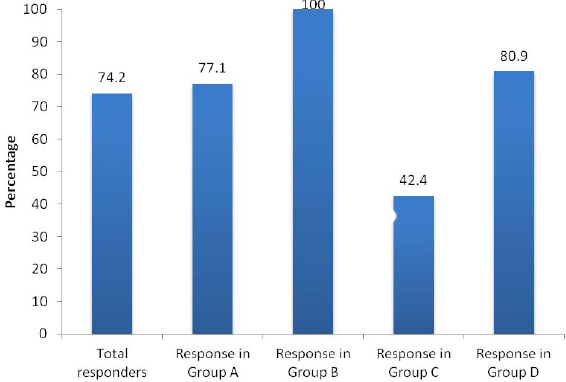
Mod. GDSS declined in all four groups at three months. When a fall of four or more was considered as an indicator of significant response to intervention, it was seen that overall 74.2% responded to intervention with the best response in Group B and the poorest was in Group C.
Conclusion
There is a significant prevalence of HP and SAD in FD. Appropriate intervention is beneficial except in those who are HP negative and SAD positive. This latter group requires further investigation and or drug intervention for SAD.
Cognitive behavioral therapy, Giemsa staining, Proton pump inhibitors
Introduction
The definitive treatment approach and the underlying patho-physiology of FD has been the subject of study for several decades. Though several publications have shown a positive correlation between FD and HP infection and FD and SAD, efficacy of HP eradication and treatment of psychiatric comorbidity in these individuals remains controversial [1–4]. Previous studies have shown that subjects with long standing functional gastrointestinal disorders have a high prevalence of psychological illness [5] and these subjects may benefit from psychotherapy [6]. Likewise, several studies have also shown improvement in dyspeptic symptoms following HP eradication [7–10]. However, a systematic review by Moayyedi P et al., showed that in ten of thirteen trials, patients with dyspepsia had no significant benefit from HP eradication when compared to the placebos [2].
In our study, we aimed to look at the association of FD with HP and with the presence or absence of coexisting psychiatric comorbidity such as SAD and to document objectively the benefit obtained with appropriate intervention, either HP eradication or non-drug psychiatric intervention or both as regards dyspepsia scores.
Materials and Methods
This prospective non-randomized interventional study was conducted in the Department of General Surgery at Mahatma Gandhi Medical College and Research Institute, Puducherry, India, from October 2012 to April 2014 after ethical approval from the Institute Human Ethics Committee.
Inclusion criteria: Patients with symptoms described in ROME III B1 criteria for FD [11] were screened and enrolled in the study after obtaining an informed consent. One or more of the following symptoms, viz., post-prandial fullness, early satiation, epigastric pain or epigastric burning if present for three months with onset at least six months prior to diagnosis were considered as positive for non-ulcer dyspepsia. The study entry parameters measured included:
a) Ultrasonography of the abdomen and upper gastrointestinal endoscopy to rule out biliary tract diseases, pancreatic diseases and abnormalities of the upper GI tract. Patients with positive findings were excluded from the study.
b) Four antral biopsies were taken during endoscopy within 2 cm of the pylorus with a standard 2.8 mm cup. Two samples were tested for HP using the rapid urease test and two samples were sent for histopathological examination by Giemsa stain for HP. The subjects were considered positive for HP if either or both tests were positive and considered negative if both tests were negative.
c) PHQ-9 was used to screen for depression [12]. GAD-7 was used to screen for anxiety [13] and PSS was used to measure the perception of stress [14]. Patients with significant scores on one or more of the questionnaires were considered to be positive for SAD. Patients with any one of the psychiatric morbidity were classified as SAD+, others as SAD-.
d) The severity of dyspepsia was assessed using the Mod. GDSS [15]. It scores the frequency of dyspeptic symptoms on a score of 0-4, intensity of dyspeptic symptoms on a score of 0-2, frequency of use of over-the-counter medication on a scale of 0-2, and frequency of use of prescribed medication on a score of 0-2 [15]. The scores can range from a minimum of zero to a maximum of ten.
Intervention: The patients were recruited into four groups as follows:
Group A (HP+, SAD+) n = 35: received HP eradication which included Cap Amoxicillin 500 mg Q8H, Tab Clarithromycin 500 mg Q12H, Cap Omeprazole 20 mg Q12H and Cap Lactobacillus Sporogenes 1cap OD, all for 14 days along with counselling therapy for SAD.
Group B (HP+, SAD-) n = 31: received only HP eradication therapy as mentioned above.
Group C (HP-, SAD+) n = 33: received only counselling therapy.
Group D (HP-, SAD-) n = 21: received proton pump inhibitors (Tab Omeprazole 40 mg Q12H) for 14 days.
It was decided by the psychiatrist that the SAD symptoms in the study groups were not serious enough to warrant medical therapy as the first intervention and required counseling for a start. Also it was felt that some of these drugs may interfere with HP eradication and treatment with proton pump inhibitors.
Follow up: Patients were followed at three months after completion of therapy. Follow up was done either through telephonic communication or hospital visits. During follow up, patients were assessed for improvement of the existing illness after receiving appropriate treatment using the Mod GDSS. Improvement of their symptoms was calculated depending on the decrease in the scores from baseline. A reduction of four or more in the Mod GDSS score compared to baseline was considered as satisfactory response to treatment.
Statistical Analysis
The data was analysed using Statistical Package for the Social Sciences version 16.0 (SPSS) and excel database. Gender wise distribution in each group and the statistical significance of difference between the number of males and females in each group was calculated using the z-test. Response to treatment in each group comparing the baseline and three months (Mod. GDSS) was assessed using the ANOVA test. The statistical difference in the overall response to treatment and gender wise response to treatment in each group was estimated using the Chi Square test. Significant response to treatment measured using the Mod. GDSS between males and females in each group was calculated using the independent unpaired t-test. The gender wise distribution and response to treatment among individuals who showed evidence of SAD was assessed using the Chi-square test.
Results
Overall 120 patients were recruited in four groups. About 55% (n=66) of the overall group were positive for HP and 56.7% (n=68) were positive for SAD. Of this 56.7%, 63 were positive for stress, 64 for anxiety and 63 for depression. A 29.2% were positive for both. It was seen that in all three types of associated psychiatric comorbidity, females exceeded males in a proportion of over 3:1. All patients were intended to be followed up for a period of three months. However, seven patients (5.8%) dropped out and were not available for follow up either by telephonic communication or hospital visit at three months (Group A – one patient, Group C – two patients, Group D – four patients).
Males and females were almost equal in number when all four groups were considered as a whole. When distributed group wise, females predominated in groups positive for SAD (Groups A and C) and males predominated in groups without SAD (Groups B and D). It was seen that nearly 90% of patients fell between 21-60 years of age [Table/Fig-1].
Age and gender distribution.
| Age group | Male | Female | Total |
|---|
| <20 | 1 | 5 | 6 |
| 21-30 | 17 | 11 | 28 |
| 31-40 | 15 | 15 | 30 |
| 41-50 | 14 | 14 | 28 |
| 51-60 | 9 | 12 | 21 |
| >60 | 3 | 4 | 7 |
| Total | 59 | 61 | 120 |
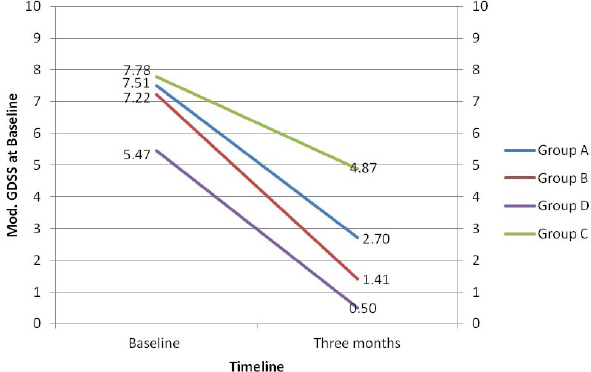
The mean baseline and post intervention Mod. GDSS in the four groups is shown in [Table/Fig-2]. When each group was compared individually with the other three, it was seen that there was significant difference between Group D and each of the other three groups in baseline scores [Table/Fig-3]. Mod. GDSS was not significantly different between HP+ and HP- patients (p=0.1278) except when HP positivity was also associated with SAD (p<0.001), whereas SAD positivity alone significantly increased (p=0.0006) the baseline Mod. GDSS [Table/Fig-4].
Baseline modified glasgow dyspepsia severity score.
| Group | Baseline | Three month | p-value |
|---|
| A (HP+/SAD+) | 7.51±1.5 | 2.70±2.51 | <0.001 |
| B (HP+/SAD-) | 7.22±1.7 | 1.41±1.0 | <0.001 |
| C (HP-/SAD+) | 7.78±1.6 | 4.87±3.3 | <0.001 |
| D (HP-/SAD-) | 5.47±1.5 | 0.50±0.6 | <0.001 |
Multivariate comparison of baseline modified glasgow dyspepsia severity score.
| Groups | Baseline scores | Mean difference | Std. error | p | Cl at 95% |
|---|
| Group A7.51±1.5 | Group B | 7.22±1.7 | 0.288 | 0.404 | >0.05 | -0.8 - 1.37 |
| Group C | 7.78±1.6 | -0.274 | 0.397 | >0.05 | -1.34 - 0.79 |
| Group D | 5.47±1.5 | 2.038 | 0.452 | <0.001 | 0.83 - 3.25 |
| Group B7.22±1.7 | Group A | 7.51±1.5 | -0.288 | 0.404 | >0.05 | -1.37 - 0.8 |
| Group C | 7.78±1.6 | -0.562 | 0.409 | >0.05 | -1.66 - 0.54 |
| Group D | 5.47±1.5 | 1.75 | 0.463 | <0.001 | 0.51 - 2.99 |
| Group C7.78±1.6 | Group A | 7.51±1.5 | 0.397 | 0.397 | >0.05 | -0.79 - 1.34 |
| Group B | 7.22±1.7 | 0.409 | 0.409 | >0.05 | -0.54 - 1.66 |
| Group D | 5.47±1.5 | 0.457 | 0.457 | <0.001 | 1.08 - 3.54 |
| Group D5.47±1.5 | Group A | 7.51±1.5 | 0.452 | 0.452 | <0.001 | -3.25 - -0.83 |
| Group B | 7.22±1.7 | 0.463 | 0.463 | <0.001 | -2.99 - -0.51 |
| Group C | 7.78±1.6 | 0.457 | 0.457 | <0.001 | -3.54 - -1.08 |
Comparison of baseline Modified Glasgow Dyspepsia Severity Score among groups.
| Comparison of baseline Mod. GDSS among groups with SAD+ and SAD- |
| Number | Baseline scores | p-value | CI at 95% |
| Group A+C (S/A/D+) | 68 | 7.65±1.6 | 0.0006 | 0.49-1.76 |
| Group B+D (S/A/D-) | 52 | 6.52±1.9 |
| Comparison of baseline Mod. GDSS among groups with HP+ and HP- |
| Number | Baseline scores | p-value | CI at 95% |
| Group A+B (HP+) | 66 | 7.38±1.6 | 0.1278 | -0.14-1.12 |
| Group C+D (HP-) | 54 | 6.89±1.9 |
| Comparison of baseline Mod. GDSS among groups with positive findings and negative findings |
| Groups | Number | Baseline scores | p-value | CI at 95% |
| Group A+B+C(HP+/ S/A/D+) | 99 | 7.51±1.6 | <0.001 | 1.27-2.80 |
| Group D (HP-/S/A/D-) | 21 | 5.47±1.6 |
The response to treatment was measured with Mod. GDSS, which ranges from 0-10. The mean values for the four groups at baseline and at three months excluding those lost to follow up are shown in [Table/Fig-5]. It was seen that in all groups, there was a declining trend of scores from baseline to three months. None of the groups showed an increase of Mod. GDSS at three months indicating that the intervention was beneficial. A reduction of four or more in the Mod. GDSS was considered as significant response to treatment. It was seen that overall 74.2% responded to intervention. The best response of 100% was seen in Group B (HP+/SAD-) followed by Group D with 80.9% (HP-/SAD-) [Table/Fig-6]. The poorest response was seen in Group C of 42%. This latter group received only psychological intervention. The overall response was significant with an alpha value of 0.001. While analysing separately gender wise response in patients with stress, anxiety and depression, no significant difference was noted between the two genders or between patients with stress, anxiety or depression when compared to one another. Gender wise difference with respect to Mod. GDSS in the four groups showed significant improvement in males in Group A, B and D (p<0.001). However, the change was not significant in Group C (p=0.1089). Female patients, they had significant improvement in Groups A, B and C (p<0.001). The significance could not be calculated in Group D since only one female came back for follow up [Table/Fig-7].
Response to treatment measured with modified glasgow dyspepsia severity score.
Overall response to treatment.
Gender wise response to treatment.
| Gender | Male | Female | Total |
|---|
| Group A | Baseline | 7.45±1.3 | 7.54±1.6 | 7.51±1.5 |
| three months | 1.72±1.5 | 3.17±2.7 | 2.70±2.51 |
| CI at 95% | 4.48-6.98 | 3.07-5.67 | 3.82-5.80 |
| p-value | <0.001 | <0.001 | <0.001 |
| Group B | Baseline | 7.25±1.8 | 7.14±1.3 | 7.22±1.7 |
| three months | 1.58±1.1 | 0.85±0.8 | 1..41±1.0 |
| CI at 95% | 4.80-6.54 | 5.03-7.55 | 5.10-6.52 |
| p-value | <0.001 | <0.001 | <0.001 |
| Group C | Baseline | 8.00±0.70 | 7.75±1.6 | 7.78±1.6 |
| three months | 5.20±3.4 | 4.80±3.3 | 4.87±3.3 |
| CI at 95% | 0.78-6.38 | 1.53-4.37 | 1.63-4.19 |
| p-value | <0.1089 | <0.001 | <0.001 |
| Group D | Baseline | 5.52±1.6 | 5.00±0.0 | 5.47±1.5 |
| three months | 0.43±0.5 | 2*1 | 0.50±0.6 |
| CI at 95% | 4.24-5.94 | - | 4.18-5.76 |
| p-value | <0.001 | - | <0.001 |
As there was only one female at three months follow up in Group D, an average, standard deviation and p-value could not be calculated.
Discussion
The principal aim of this study was to assess the correlation between HP and SAD among patients with FD. We found that of 120 patients with FD, only 17.5% were negative for HP and SAD. The remaining 82.5% patients were positive for either HP or SAD or both. This suggests that the coexistence of HP and of SAD among patients suffering from FD is high in India. Prevalence of HP and SAD in FD-on a global scale, the positive correlation between HP and FD was found to be between 23%-61% [16]. In India, the prevalence rate of HP in previous published literature is consistent with our results [17-19]. The higher prevalence of HP in FD in developing countries (80%-90% vs. 30%) [20] is thought to be multifarious due to the failure of treatment and emergence of drug resistance besides lack of environmental hygiene which facilitates HP transmission [21]. Previous data has shown a strong correlation between SAD and FD [22] more so among the female gender [23-25].
Assessment with Mod. GDSS: In our study, we have considered a fall of four or more on the Mod. GDSS score from baseline to three months as positive response to treatment. Group A and Group C had relatively higher scores on the Mod. GDSS as compared to Group B and D both at baseline and at follow up, suggesting that individuals who are positive for SAD are likely to have a poorer quality of life as compared to those without SAD.
Published literature using the GDSS scale has shown that in healthy individuals, an average of 1.2 was observed in comparison to individuals with FD who had an average of 10.5 (GDSS score range from 0-20) [26]. McColl K et al., used an abbreviated version of the GDSS, which was adapted in our study. He observed that the mean score among healthy volunteers was 1 (0-6) and in individuals with FD was 6.7 (4-10) which is comparable with our results [15].
Outcome at three months with appropriate intervention: A study done by Haag S et al., showed similar results while comparing standard medical therapy and intense medical therapy along with Cognitive Behavioural Therapy (CBT). He found significant improvement in symptoms (p<0.025) in the group that received medical therapy along with CBT [27]. There is very little published literature on the outcome of combined HP eradication and counseling therapy in patients with FD positive for HP and SAD.
The regimen used by us was chosen as it is proven to have an 85-95% eradication rate, when given for a period of 10-14 days [28,29]. Previously published literature using similar though slightly modified assessment tools have shown 78%-95% complete or almost complete resolution of dyspeptic symptoms following HP eradication, which is comparable with our results [8,9,30]. However, several other studies have shown different outcomes of HP eradication in patients with FD [1,31].
The poor response in the groups with SAD seen by us may be due to either: (i) inadequate counseling; (ii) insufficient duration of counseling; (iii) lack of compliance; and (iv) lack of drug treatment for SAD. Previous research on FD and SAD, including antidepressants and antianxiety drugs along with counseling therapy have showed more promising results when compared to isolated counseling therapy [6,31-35]. Yet another reason may be that SAD is the effect and not the cause of FD.
Group D receiving only PPI’s showed a significant improvement at three months follow up. This group had the lowest scores in the Mod. GDSS at baseline and three months with a statistically significant reduction. Treatment with proton pump inhibitors for a period of two weeks is standard protocol for those presenting with unexplained dyspeptic symptoms or those with chronic gastritis.
These findings are consistent with various other studies done previously [36,37]. There is Level A evidence supporting the role of PPI’s in symptomatic improvement of FD [38,39].
Limitation
The possible limitation of this study are short term follow up period of three months and the groups with stress, anxiety and depression positive will need further detailed investigation and possibility of improved outcomes with longer duration of counseling and follow up.
Conclusion
A significant proportion of patients with FD (Rome III, B1) had associated HP and SAD. All patients with FD showed a significant improvement in dyspepsia scores after three months with appropriate treatment with the least response in Group C consisting of patients positive for SAD alone. This latter group probably requires longer treatment or drug intervention for psychiatric comorbidity. Further studies including a larger sample size with a longer duration of follow up along with better strategy at follow up to ensure complete HP eradication will need to be conducted. Also, the symptomatic benefit from adding antidepressive/antianxiety drugs to the treatment of SAD will need to be studied in more detail.
1As there was only one female at three months follow up in Group D, an average, standard deviation and p-value could not be calculated.
[1]. Moayyedi P, Soo S, Deeks J, Delaney B, Harris A, Innes M, Eradication of Helicobacter pylori for non-ulcer dyspepsiaCochrane Database Syst Rev 2003 (1):CD002096 [Google Scholar]
[2]. Moayyedi P, Soo S, Deeks J, Forman D, Systematic review and economic evaluation of Helicobacter pylori eradication treatment for non-ulcer dyspepsiaBr Med J 2000 321:659-64. [Google Scholar]
[3]. Wood J, Neuropathophysiology of functional gastrointestinal disordersWorld J Gastroenterol 2007 13(9):1313-32. [Google Scholar]
[4]. Hojo M, Miwa H, Yokoyama T, Ohkusa T, Nagahara A, Kawabe M, Treatment of functional dyspepsia with antianxiety or antidepressive agents: systematic reviewJ Gastroenterol 2005 40(11):1036-42. [Google Scholar]
[5]. Alander T, Svärdsudd K, Johansson S-E, Agréus L, Psychological illness is commonly associated with functional gastrointestinal disorders and is important to consider during patient consultation: a population-based studyBMC Med 2005 3:8 [Google Scholar]
[6]. Paré P, Facg F, Math JLM, Hawes IA, Acpr BSP, Paré P, Counselling by primary care physicians may help patients with hearburn-predominant uninvestigated dyspepsiaCan J Gastroenterol 2010 24(3):189-95. [Google Scholar]
[7]. Kate V, Maroju NK, Ananthakrishnan N, Helicobacter pylori Infection and upper gastrointestinal disordersGastroenterol Res Pract 2013 Jan [Google Scholar]
[8]. Malfertheiner P, Mössner J, Fischbach W, Layer P, Leodolter A, Stolte M, Helicobacter pylori eradication is beneficial in the treatment of functional dyspepsiaAliment Pharmacol Ther 2003 18:01-14. [Google Scholar]
[9]. Abdul Aziz AF, Hamzah Z, Tong SF, Nadeson S, Wan Puteh SE, Helicobacter pylori related dyspepsia: prevalence and treatment outcomes at University Kebangsaan Malaysia-Primary Care CentreAsia Pac Fam Med 2009 8:4 [Google Scholar]
[10]. Lane JA, Murray LJ, Noble S, Egger M, Harvey IM, Donovan JL, Impact of Helicobacter pylori eradication on dyspepsia, health resource use, and quality of life in the Bristol helicobacter project: randomised controlled trialBMJ 2006 332(7535):199-204. [Google Scholar]
[11]. Drossman D, Appendix B: Comparison Table of Rome II & Rome III Adult Diagnostic CriteriaAm J Gastroentrol 2010 105:798-801. [Google Scholar]
[12]. Kroenke K, Spitzer RL, Williams JBW, The PHQ-9J Gen Intern Med 2001 16:606-13. [Google Scholar]
[13]. Spitzer RL, Kroenke K, Williams JBW, Löwe B, A brief measure for assessing generalized anxiety disorder: the GAD-7Arch Intern Med 2006 166:1092-97. [Google Scholar]
[14]. Cohen S, Perceived stress scaleMeas Stress A Guid Heal Soc Sci 1994 1994 [Google Scholar]
[15]. McColl K, El-Nujumi A, Murray L, El-Omar EM, Dickson A, Kelman AW, Assessment of symptomatic response as predictor ofHelicobacter pylori status following eradication therapy in patients with ulcerGut 1998 42:618-22. [Google Scholar]
[16]. Gisbert JP, Calvet X, Helicobacter Pylori “Test-and-Treat” strategy for management of dyspepsia: A Comprehensive ReviewClin Transl Gastroenterol 2013 4:e32 [Google Scholar]
[17]. Sodhi JS, Javid G, Zargar SA, Tufail S, Shah A, Khan BA, Prevalence of Helicobacter pylori infection and the effect of its eradication on symptoms of functional dyspepsia in Kashmir, IndiaJ Gastroenterol Hepatol 2013 28:808-13. [Google Scholar]
[18]. Kate V, Ananthakrishnan N, Badrinath S, Ratnakar C, Prevalence of Helicobacter pylori infection in disorders of the upper gastrointestinal tract in south IndiaNatl Med J India 1998 11(1):05-08. [Google Scholar]
[19]. Katelaris PH, Tippett GH, Norbu P, Lowe DG, Brennan R, Farthing MJ, Dyspepsia, Helicobacter pylori, and peptic ulcer in a randomly selected population in IndiaGut 1992 33:1462-66. [Google Scholar]
[20]. Loyd R, McClellan D, Update on the evaluation and management of functional dyspepsiaAm Fam Physician 2011 83(5):547-52. [Google Scholar]
[21]. Ahmed N, 23 years of the discovery of Helicobacter pylori: is the debate over?Ann Clin Microbiol Antimicrob 2005 4:17 [Google Scholar]
[22]. Vishnar A, Ghulam R, Mittal R, Non ulcer dyspepsia and its correlation with life stress, anxiety and depressionIndian J Psychiatry 1999 41(4):88-93. [Google Scholar]
[23]. Mahadeva S, Goh K-L, Epidemiology of functional dyspepsia: a global perspectiveWorld J Gastroenterol 2006 12:2661-66. [Google Scholar]
[24]. Cardin F, Ambrosio F, Amodio P, Minazzato L, Bombonato G, Schiff S, Quality of life and depression in a cohort of female patients with chronic diseaseBMC Surg. BioMed Central Ltd 2012 12(Suppl 1):S10 [Google Scholar]
[25]. Chang F, Chen P, Wu T, Pan W, Chang H, Ms SW, Prevalence of functional gastrointestinal disorders in Taiwan :questionnaire-based survey for adults based on the Rome III criteriaAsia Pac J Clin Nutr 2012 21:594-600. [Google Scholar]
[26]. Zanten S van, Assessment of outcome in dyspepsia: has progress been made?Gut 2002 50:23-25. [Google Scholar]
[27]. Haag S, Senf W, Tagay S, Langkafel M, Braun-Lang U, Pietsch A, Is there a benefit from intensified medical and psychological interventions in patients with functional dyspepsia not responding to conventional therapy?Aliment Pharmacol Ther 2007 25(8):973-86. [Google Scholar]
[28]. Ables A, Simon I, Melton E, Update on Helicobacter pylori treatmentAm Fam Physician 2007 75(3):351-58. [Google Scholar]
[29]. Kate V, Ananthakrishnan N, Treatment of Helicobacter pylori infection: a reviewIndian J Pharmacol 2001 33:410-16. [Google Scholar]
[30]. Mazzoleni L, Sander G, Helicobacter pylori eradication in functional dyspepsiaArch Intern Med 2011 171(21):1929-36. [Google Scholar]
[31]. Matsuda N, Kinoshita E, Functional dyspepsia: review of pathophysiology and treatmentOpen Gastroenterol J 2009 3:11-12. [Google Scholar]
[32]. Harmon RC, Peura DA, Evaluation and management of dyspepsiaTherap Adv Gastroenterol 2010 3:87-98. [Google Scholar]
[33]. Brun R, Kuo B, Functional dyspepsiaTherap Adv Gastroenterol 2010 3(3):145-64. [Google Scholar]
[34]. Chua ASB, Functional dyspepsia :Are psychosocial factors of relevance ?World J Gastroenterol 2006 12(17):2694-700. [Google Scholar]
[35]. Craig OF, Quigley EMM, Current and emerging therapies for the management of functional gastrointestinal disordersTher Adv Chronic Dis 2011 2:87-99. [Google Scholar]
[36]. Voiosu TA, Giurcan R, Voiosu AM, Voiosu MR, Functional dyspepsia todayMædica 2013 8:68-74. [Google Scholar]
[37]. Suzuki H, Okada S, Hibi T, Proton-pump inhibitors for the treatment of functional dyspepsiaTherap Adv Gastroenterol 2011 4:219-26. [Google Scholar]
[38]. Duckworth M, Ra P, Isa È, Nen È, Talley NJ, Pare P, Efficacy of omeprazole in functional dyspepsia: double-blind, randomized, placebo-controlled trials (the Bond and Opera studies)Aliment Pharmacol Ther 1998 12:1055-65. [Google Scholar]
[39]. Lacy BE, Talley NJ, Locke GR, Bouras EP, DiBaise JK, El-Serag HB, Review article: current treatment options and management of functional dyspepsiaAliment Pharmacol Ther 2012 36(1):03-15. [Google Scholar]