Denture hygiene is of utmost importance because dentures are used by the patients throughout the day and are in constant touch with oral environment including various microorganisms [1]. The microbial load of the prosthesis is responsible for increased incidence of oral problems such as denture stomatitis, inflammatory papillary hyperplasia etc., [2].
Three methods are advocated for cleaning of dentures that includes mechanical, chemical and combination of both. Mechanical method is routinely and widely used by the patients but many elderly patients are not able to follow it because of lack of compliance and poor motor coordination due to age and hence, the use of chemical denture cleansers becomes a viable option for such patients [3]. Denture cleansers are either available commercially as sodium hypochlorite solutions, denture cleansing tablets (fittydent tablets) or are present as a regular household item like vinegar. Ideally, cleanser chosen should be compatible with the denture base material to be disinfected but studies have shown that the cleansers may alter the physical properties of denture base resin on prolonged used [4-7]; Contrary to it, few studies claim that cleansers if used according to manufacturer’s instructions do not affect the physical properties [8-11].
Among various physical properties that can be affected by use of cleansers, flexural strength is of prime interest because denture base resins may fail clinically due to flexural fatigue [12,13]. Effect of cleansers on surface roughness of acrylic resins is also relevant as it can influence the adhesion and retention of microorganisms which can further aggravate oral problems [14].
If routine use of denture cleansers affects the physical properties like flexural strength or surface roughness of denture base resin then it may be more detrimental to the prosthesis rather than improving its longevity. Thus, choosing an appropriate cleanser is of paramount importance. Since, the studies in the literature are not in agreement regarding the adverse effects of chemical cleansers on denture base resin and also comparative studies of effect of household cleansers with that of commercially available cleansers is not very well documented, so, this study focused on evaluation of flexural strength and surface roughness of heat cured denture base resin when subjected daily to different cleansers (one household and two commercial cleansers) for a period of three months.
Materials and Methods
This in vitro study was conducted at MM College of Dental Sciences and Research, Mullana, Haryana, India. Total of 32 and 40 specimens of heat cure denture base resin for surface roughness and flexural strength testing respectively were fabricated.
Steps Followed for the Study
Specimen fabrication: Disc shaped wax patterns (10 mm in diameter and 2 mm thick) for surface roughness testing and rectangular wax patterns of dimension 65 mm x 10 mm x 2.5 mm (According to ADA Specification No.12) for flexural strength testing were fabricated using stainless steel mould of desired dimension and were invested in Type III gypsum product (Dental Stone- Gypstone, prevest denpro Ltd., Jammu, India) in a metallic flask. After setting of the stone, dewaxing was performed followed by application of separating media (Cold mold seal, Dental products of India, Mumbai, India). Molds were packed with heat polymerized acrylic resin (DPI Heat Cure, Dental Products of India, India) and were processed according to manufacturer’s instructions. Long cure cycle of polymerization (73°C for 90 minutes followed by 94°C for 30 minutes) was done. The specimens were removed from the molds and trimmed using tungsten steel bur mounted in a handpiece at low speed followed by finishing with 120, 220, 320-grit sandpaper and polishing with wet rag and slurry of pumice. Dimensions of all specimens were checked with digital Vernier caliper and those not accurate were replaced with new specimens. All specimens [Table/Fig-1a,b] thus obtained were immersed in distilled water at 37±1°C for 24 hours for residual monomer elimination.
Specimens of heat cure denture base resin. a) Specimens for surface roughness. b) Specimens for flexural strength.
Cleansing protocol: Specimens were subjected to daily cleansing for three months by immersion in different cleansers according to the group they belonged to. Specimens not subjected to any cleanser served as control. Three cleansers used in the study are tabulated in [Table/Fig-2].
| S. No | Name | Brand | Concentration | Immersion time |
|---|
| 1 | Sodium hypochlorite | Organo Biotech | 1% | 10 minutes |
| 2 | Fittydent | Dr.Reddy | 1 tablet | 30 minutes |
| 3 | Vinegar | American Garden White vinegar | 100% | 10 minutes |
Specimens (n=32) to be evaluated for surface roughness [Table/Fig-1a] were randomly divided into 4 groups (Group A, B, C and D). Group A served as control whereas Group B, C and D were subjected to daily immersion in cleanser 1,2 and 3 respectively for three months [Table/Fig-2]. All specimens were stored in distilled water for entire period of the study.
Specimens (n=40) to be evaluated for flexural strength [Table/Fig-1b] were randomly divided into five groups (Group A, B, C, D and E). Group A specimens were tested just 24 hours after fabrication and served as baseline and specimens in Group B were stored in distilled water for entire period of the study and served as control. Group C, D and E were subjected to daily immersion in cleanser 1, 2 and 3 respectively [Table/Fig-2] for three months.
Surface roughness testing: Surface analyser (Surftest SJ-210, Mitutoyo, USA) was used to measure the surface roughness of each disc shaped specimens before and after immersion procedures [Table/Fig-3]. The stylus of analyser moved across the specimen surface and recorded three lines with 1 mm distance. The mean roughness (Ra) of three lines was calculated. The mean difference in surface roughness of the specimens before and after immersions was also calculated.
Surface roughness testing in Surface Profilometer.

Flexural strength testing: For testing flexural strength, specimens were subjected to three point bending test by mounting specimens on Universal testing machine (Instron, India) and loading with 50 Kgf (Kilogram – force) at a crosshead speed of 5 mm/min [Table/Fig-4]. Peak load was noted at which the specimens fractured. The flexural strength (S) of each rectangular specimen was calculated from the formula:
Flexural strength testing in universal testing machine.
 S= 3PL/2bd2
S= 3PL/2bd2Where S = flexural strength (MPa), P = peak load, L = distance between the supports (50 mm), B = width of specimen (10 mm), D = specimen thickness (2.5 mm).
Statistical Analysis
The Ra and S Values were submitted to statistical analysis by one-way analysis of variance (ANOVA) followed by post-hoc Tukey’s test with the aid of the statistical software SPSS version 17.5. All tests were performed using a confidence level of 95% and p-value ≤ 0.05 was considered significant in all tests.
Results
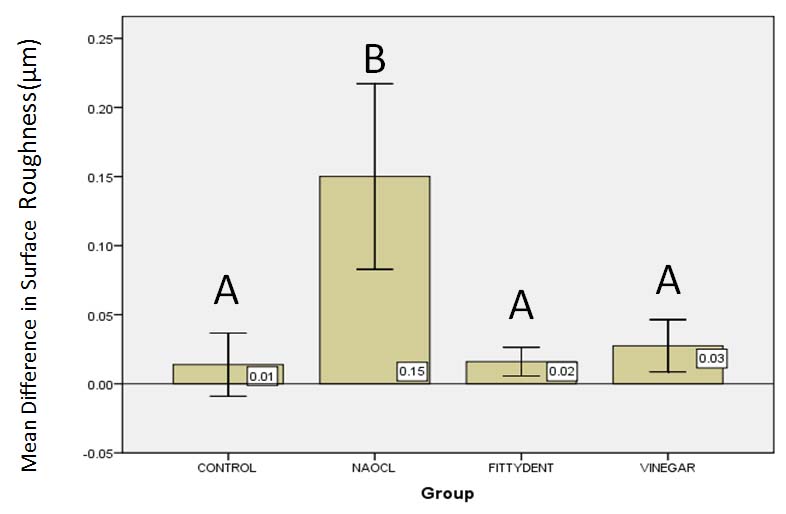
Surface roughness: [Table/Fig-5] shows the mean and standard deviation for each denture cleanser. The one-way ANOVA analysis data showed statistically significant difference (p<0.001) in surface roughness of groups Further analysis with the post-hoc Tukey’s test. [Table/Fig-5] indicated significantly higher surface roughness for specimens immersed in sodium hypochlorite compared to other groups.
Mean +Values with different letters are significantly different.
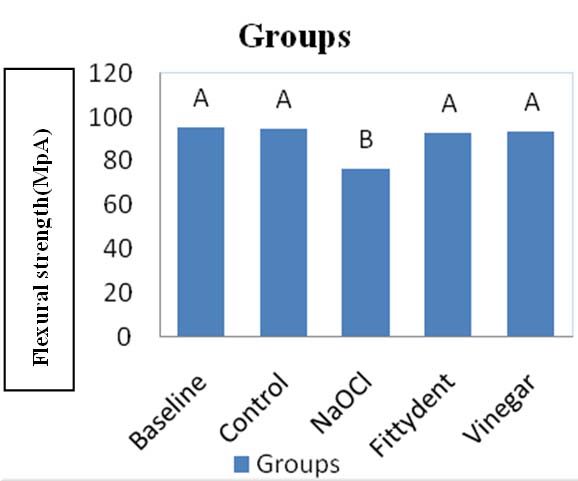
Flexural strength: [Table/Fig-6] shows the mean flexural strength (S) and standard deviation for each denture cleanser. The one-way ANOVA analysis data showed statistically significant decrease (p<0.001) in flexural strength for the treatments. Further analysis with the post-hoc Tukey’s test indicated significant decrease in the flexural strength of specimens immersed in sodium hypochlorite compared to other groups [Table/Fig-6].
Mean+SD of flexural strength (S) in Mpa(n=8). Values with different letters are significantly different.
Discussion
Denture cleaning being an important part in maintenance of prosthesis and reducing the oral problems, needs to be performed effectively as well as routinely. Chemical cleansing is found to be better and a recommended method especially in patients with poor dexterity and in old age people having dementia [15]. Various in vitro and in vivo studies have shown that chemical methods are effective enough to remove biofilm, food debris and also tobacco stains from the denture surface [16-18]. Chemical cleansers may thoroughly disinfect denture but it is important to analyse how these chemicals alter the properties of denture base material when used for longer time. Various commercial denture cleansers are available for use to denture wearer but they may also use household cleansers like vinegar because of their easy availability, low cost and less toxicity [19]. Literature is scanty in regard to the comparative effect of household cleansers like vinegar with that of commercially available products like sodium hypochlorite solutions and fittydent denture cleansing tablets, on physical properties of denture base resin.
It has been reported that immersion in 1% sodium hypochlorite for 10 minutes is effective in elimination of microorganisms from both superficial and inner surfaces of material [20]. Da Silva FC et al., also reported that 1% NaOCl for 10 minutes had best antimicrobial activity among various tested disinfectants [21]. Hence, in the present study, 1% NaOCl for 10 minutes was chosen as cleanser.
Fittydent denture cleansing tablet is a commercial denture cleansing product containing sodium perborate as the main ingredient. Fittydent tablets when dissolved in water, readily decomposes to form Hydrogen Peroxide (H2O2) which when goes in aqueous solution, releases nascent oxygen (O) which in turn cleanses the surface debris and stains via effervescent action. Manufacturer’s recommended immersion time for fittydent is 30 minutes [22].
Vinegar is regular household product which is easily available, inexpensive and has low toxicity as well. Vinegar is basically 6%-13% acetic acid which is a weak acid and only partially dissociates in aqueous solution. White vinegar is frequently used in concentration of 50% and 100% for disinfection of toothbrushes and denture base acrylic resins. Da Silva FC et al., Yildirim-Bicer AZ et al., advocated the use of 100% vinegar for 10 minutes as denture disinfectant especially against Candida Albicans [21,23].
Physical properties studied include flexural strength of denture base resin as it determines the longevity of prosthesis. Poor flexural strength results in increase incidence of fracture of denture both intraorally and extraorally. It is influenced by many factors like residual monomer content, composition of resin, amount of plasticiser present, absorbed water etc., [24]. In the present study, only one denture base material was used to control variation in composition or amount of plasticizer. To eliminate the residual monomer content, all the samples were stored in distilled water for 24 hours prior to immersion in various cleansers. Also standard curing cycle was used to prepare all acrylic specimens.
Result of the present study revealed that immersion in 1% NaOCl resulted in significant decrease (p<0.05) in flexural strength. This is similar to findings of Davi LR et al., and Pisani MX et al., who also reported decrease in flexural strength with use of 1% NaOCl [7,25]. Pisani MX et al., attributed the decrease in strength to alteration of polymer resin chain by NaOCl [25]. However, flexural strength values were still above the minimum value of 65 MPa set forth by ADA Sp. No.12 [26]. Vinegar and fittydent tabs did not significantly alter the flexural strength. Sato S et al., also reported no change in flexural strength when sodium perborate based cleansers were used [9]. Contrary to our study, Paranhos HDFO et al., Arruda CNF et al., and Peracini A et al., reported no change in flexural strength with use of NaOCl, but the concentration of disinfectant, duration of immersion and type of acrylic resin is different from present study [5,10,27].
Surface roughness is another important property which influences the bio-film formation by providing retentive areas for food debris and microorganisms. Increase in surface roughness can cause further difficulty in removal of biofilm. Quirynen M and Bollen CM stated that bacteria when once adheres to rough surface can survive for long period of time and cannot be easily removed by regular hygiene methods thus, smooth surface is important to prevent microorganisms retention [28]. They also suggested that surface roughness should be ≤2 μm, above which dramatic bacterial colonization occurs. Williams DW and Lewis MAO also supported the fact that surface roughness increase colonization by microorganisms and cause indirect injury to tissue [29]. Literature cited that roughness of smooth acrylic surface is only 0.12 μm which is well below the critical value of 2 μm [8].
In present study, fittydent and vinegar did not cause much change in surface roughness (p>0.05) as compared to sodium hypochlorite (p<0.05) which increased roughness of acrylic specimens. Results of present study are similar to Porwal A et al., Paranhos HDFO et al., Carvalho CF et al., Da Siva FC et al., and Pisani MX et al., who found that sodium hypochlorite caused change in surface roughness of acrylic [4-6,21,25]. In contrary, Garcia RCMR et al, found that use of sodium perborate cleanser increases surface roughness because of inability to remove pellicle formed on acrylic surface [30]. Ural C et al., also did not find any difference in commercial cleansers and sodium hypochlorite with respect to their effect on surface roughness [8]. Difference in the results could be attributed to different denture base resins used, difference in immersion time and period chosen.
Limitation
There were certain limitations in the present study like effect of different chemical cleansers was studied only on one type of denture base resin, true simulations of oral conditions i.e., composition and pH of saliva and presence of biofilm was not done and time period of the study was limited to three months although, denture cleansers may be used for much longer time.
Conclusion
With regard to flexural strength immersion in 1% sodium hypochlorite for 10 minutes caused significant decrease in strength as compared to vinegar and fittydent tablets and hence, should be used with caution when used for longer duration. However, clinical interpretation of result should be done carefully as flexural strength values in all test groups were within acceptable range. Sodium hypochlorite also resulted in increase in surface roughness as compared to fittydent and 100% Vinegar thus, can be detrimental to prosthesis when used for longer duration.
Further studies can be directed to assess the effect of varying concentrations and immersion periods of chemical cleansers on other relevant physical properties of denture base resins, so as to help the clinician choose the best material.