Hernia is an abnormal protrusion of contents of a body cavity through a normal or abnormal opening in that body cavity. Most of the hernias occur through the abdominal wall and amongst them, inguinal hernias are the commonest. The incidence of inguinal hernia has been reported to be around 5%-7% [1].
The definitive treatment of inguinal hernias is surgery which in most cases is done on an elective basis. Approximately 20 million inguinal hernia repairs are performed all over the world annually [2]. Majority of the repairs are done by open method. However laparoscopic approach has become an attractive alternative. Presently, the trend is towards tension free mesh repairs.
Various biomaterials in the form of mesh are nowadays available and can be used for the repair of groin hernia offering unique advantages and disadvantages. Use of mesh reduces the recurrence by 30%-50% [3].
The ideal mesh should be chemically inert, not modified by body fluids, not invoke an inflammatory reaction, have no malignant potential, have no anaphylactic reaction, could be molded in the desired form, cost effective, easily available, resistant to infection, able to bear mechanical strains, should behave more like an autologous tissue. The search for such a mesh continues to date.
The standard 15 cm x 15 cm size non absorbable polypropylene mesh is the most common variety used [4]. It is inexpensive, easily available and provides good strength. The concern with it is chronic postoperative pain (inguinodynia) and foreign body sensation. The densely woven structure of the mesh (pore size 0.8 mm) produces an intense inflammatory reaction, leading to a firm scar with reduced elasticity of the abdominal wall.
Composite meshes are a kind of hybrid meshes that incorporate an absorbable component which not only lends pliability to the mesh and aids in mesh placement but are having larger pore size (>3 mm).
Few studies have been done comparing the early outcomes such as postoperative pain, seroma/haematoma formation, foreign body sensation and return to work activities, associated with the use of non absorbable polypropylene and partially absorbable composite meshes in laparoscopic repair of inguinal hernia.
The aim of the present study was to compare early outcomes using non absorbable polypropylene and partially absorbable composite mesh in the laparoscopic TAPP repair of inguinal hernia.
Materials and Methods
The above study was conducted in the Department of Surgery at Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi over a period of 18 months. All patients between the age group of 15-60 years, presenting to the Outpatient Department (OPD) with unilateral inguinal hernia were included in the study. Total 60 patients were included in the study. They were divided in two groups of thirty each using the randomization technique of sealed envelope. We used 7.6 cm x 15 cm composite ULTRAPRO Mesh (Johnson & Johnson International) in Group-1 and 8.5 cm x 13.7 cm non absorbable polypropylene BARD 3D Max Mesh (Davol Inc.) in Group-2. All the patients underwent TAPP repair of inguinal hernia and tacks were used for the fixation of mesh to the anterior abdominal wall and also for the peritoneal flap over the mesh. The patients were informed about the procedure, the study and written informed consent for the same was taken. The study protocol was approved by the Local Ethical Committee. All the patients were discharged after 48 hours of surgery.
Inclusion Criteria
Patients in the age group of 15-60 years having unilateral inguinal hernia.
Exclusion Criteria
Patients with bilateral inguinal hernia;
Hernia patients who developed irreducibility, obstruction or strangulation and presented as an emergency;
Patients with recurrent inguinal hernia;
Patients having contraindications to laparoscopic surgery.
Following parameters were analyzed in the study subjects at the time of discharge and three months after the procedure.
Pain – assessed using the Visual Analogue Scale (VAS).
Sensation of heaviness.
Presence of a lump at hernial site.
Return to normal work activities.
Statistical Analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± Standard Deviation (SD) and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected then non parametric test was used. Statistical tests were applied as follows:
Quantitative variables were compared using Unpaired t-test/Mann-Whitney U Test (when the data sets were not normally distributed) between the two groups.
Qualitative variables were correlated using Chi square test /Fisher’s-exact test.
A p-value of <0.05 was considered statistically significant.
The data were entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
Of the 60 patients enrolled in the study, 35 (58.3%) were found to have indirect inguinal hernia while 25 (41.7%) had a direct type. Almost all the patients included were males (95%) with only 3 (5%) female patients. Mean age of patients was found to be 41.91 years with a SD of 10.925. In the group receiving composite mesh (Group-1), the mean age of patients was found to be 39.6 ± 11.33 years while in the non absorbable mesh group (Group-2), the mean age was found to be 44.23±10.52 years. Both groups were comparable in demographic characteristics. A total of 68.3% patients had hernia of the right side while 31.7% had it on the left side.
The two groups were compared in the postoperative period for pain, foreign body sensation, presence of a lump at hernia site, and time to return to normal work activities.
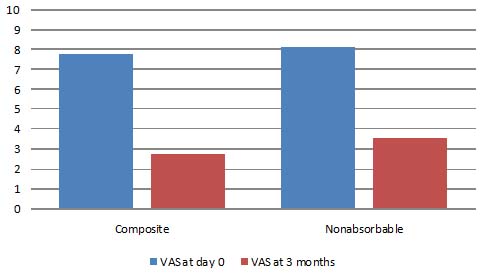
Postoperative pain: In the immediate postoperative period, at the time of discharge, mean VAS score in Group 1 was 7.77±0.678 while in Group 2, it was 8.10±0.661 (VAS 0). The overall mean VAS was 7.93±0.669. The difference in the two groups was not found to be significant (p-value = 0.087) using the Mann–Whitney U test.
After three months, the severity of pain decreased in both the groups with a mean VAS score of 2.73±0.944 in the composite group and for the non absorbable group, mean VAS score was 3.53 ± 0.973 (VAS 3). This difference was found to be significant with a p-value of 0.003 using the Mann–Whitney U test [Table/Fig-1].
Comparison of pain with mean VAS score.
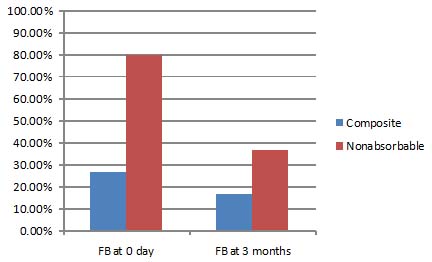
Sensation of heaviness: This was described by patients as something rubbing against their groin on the side of their hernia. In the immediate postoperative period, it was reported by eight patients (26.7%) in the composite group while in the other group, it was reported by 24 patients (80%). However, after three months, this sensation persisted in five patients from Group-1 (16.7%) and in 11 patients in Group-2 (36.6%). Using the Chi square and McNemar tests, the results were found to be significant in the immediate postoperative period (p-value<0.005) but after three months, the significance is lost (p-value 0.08) [Table/Fig-2].
Foreign Body (FB) sensation in percentage.
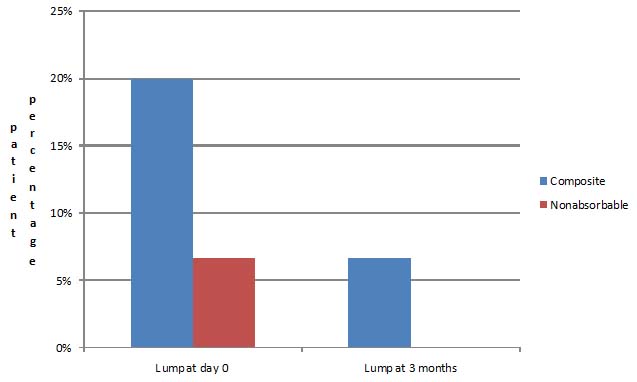
Presence of lump: Patients were evaluated for the presence of any lump (seroma/haematoma) at the hernia site. In Group-1, six patients (20%) developed a lump at the hernia site in the immediate postoperative period. Out of these six, lump resolved in four patients and only two of them had it after three months. In Group-2, only two patients had a lump in the immediate period which disappeared over three months [Table/Fig-3]. Using the Fisher’s exact test, the results were not significant (p-value of 0.254).
Presence of lump at hernia site (seroma/haematoma).
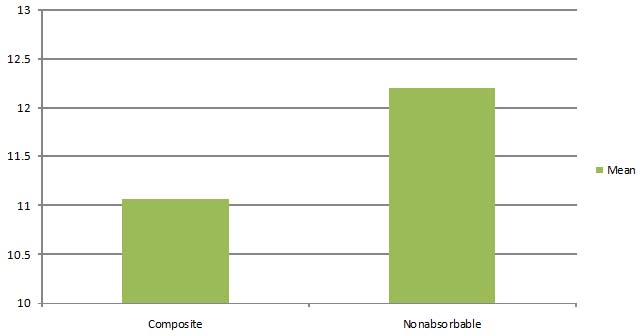
Return to work: Patients who received the composite mesh (Group-1) reported back to work earlier (mean of 11.07±2.227 days) while patients who received non absorbable mesh (Group-2), the mean number. of days before return to work were 12.20±1.883. This difference was found to be significant using the student independent t-test with a p-value of 0.038 [Table/Fig-4].
Mean number of days to return to work.
Discussion
Inguinal hernia repair is probably the most commonly performed procedure under the domain of general surgery. Estimates are that 20 million of inguinal hernia repairs are performed globally every year [2]. Various techniques have been described for repair. Tension free repairs are in vogue presently because of lower rates of recurrences associated with them.
The use of mesh was first described by Usher in 1958 but popularized by Liechtenstein around 30 years later. Presently one million meshes are being used across the globe annually [5]. Over the years, the different types of meshes available to the surgeons have grown tremendously. Light weight meshes were introduced in 1998 and are now accepted superior to heavy weight meshes. Chronic postoperative pain and return to work are now the primary outcomes over which the supremacy of any mesh is being evaluated.
Composite meshes were thus introduced which combined absorbable materials with the non absorbable ones and are the basis of most new mesh designs. The essential advantage with these meshes is that their intraperitoneal placement causes minimal adhesion formation.
Few studies have been conducted where composite meshes are compared with non absorbable meshes in laparoscopic hernia repair for a short period (three months).
The mean age of the patients in the two groups was 41.91 years with a SD of 10.952 years. The incidence of hernia increases with age [6]. In one review, the median age at presentation was 60 to 79 years for women compared with 50 to 69 years for men. Male to female ratio was 19:1. The ratio was found to be 6:1 by Read RC and White HJ [7,8]. There was preponderance of right sided inguinal hernia (41 vs 19) and a slight predominance of indirect inguinal hernia over the direct one (35 vs 25). The results are similar to a study by Schopf S et al., [9].
In our study, the VAS-0 score in immediate postoperative period was less in composite mesh group as compared to nonabsorbable mesh group (7.77±0.678 v/s 8.10±0.661) but the difference was not statistically significant. At follow up after three months of surgery, the degree of pain was considerably lower in composite mesh group. It was also statistically significant (p-value=0.003).
In a study by Shah BC et al., three times higher incidence of pain was reported in the group receiving non absorbable polypropylene mesh than the group receiving lightweight polyester mesh [10]. Another study by Smietanski M, reported less pain with the use of composite mesh (36.2%) than polypropylene one (55.2%) in the early postoperative period [11]. This trend persisted after three months (17.1% vs 9.8%). In our study also, pain scores remained higher in the group receiving the non absorbable mesh (3.53 vs 2.73). The higher pain associated with non absorbable meshes can be attributed to their smaller pore size (0.8 mm). Meshes with smaller pore size give rise to the phenomenon of granuloma bridging. Normally, granulomas form around individual mesh fibers as part of the foreign body reaction. Bridging is described as the process by which individual granulomas join each other and encapsulate the whole mesh. This produces a stiff scar plate and reduced flexibility [5], but a study by Bringman S et al., [12] has contradictory findings.
Sensation of heaviness was significantly higher in the non absorbable group in our study which can be attributed to more intense fibrous reaction that occurs with non absorbable polypropylene meshes as the composite mesh uses less but more pliant foreign material. Our finding corroborates with study conducted by Bringman S et al., [13]. In this study, it was found that 22.6% of the patients with polypropylene mesh implanted in them had foreign body sensation as compared to 14.6% in the lightweight mesh group. Horstmann R et al., compared functional outcomes with the use of ProleneTM, VyproIITM and titanium coated meshes in 672 patients [14]. Postoperatively, a greater number of patients complained of foreign body sensation in the ProleneTM group as compared to VyproIITM or titanium groups (9.1% vs 5.5% vs 3.5%). Paajanen H reported that there was non significant difference between the foreign body sensation with polypropylene and composite meshes [15]. The results in a study by Post S et al., showed higher rates of foreign body sensation with the use of standard polypropylene mesh (43.8% vs 17.2%) at the end of six months [16], but in a study by Bittner R et al., comparing polypropylene and lightweight titanium meshes, there was no such difference [17].
The frequency of a lump at the hernia site was higher in the composite group in our study, but it was not statistically significant. Only one study by Bringman S et al., reports higher seroma rate with the use of composite mesh [18]. A 2012 study by Bangash A et al., showed a higher frequency of seroma formation with the use of polypropylene mesh [19]. Similar results were demonstrated in study by Schumpelick V et al., [20].
An earlier return to work activities in the group receiving composite mesh was found in our study (11.07 days vs 12.20 days). The difference however is numerically trivial but statistically significant. The less postoperative pain associated with composite meshes could be the reason behind it. Bringman S et al., demonstrated similar findings between the use of ProleneTM and VyproTM (11 days vs 9 days) [18]. Chowbey PK et al., had compared ProleneTM with UltraproTM and found out that return to normal daily activities and work was earlier in patients of the composite group [21]. However, the earlier return to daily activities was significant while earlier return to work was not significant. Heikkinen T et al., reported a non-significant difference in return to work between the polypropylene and composite groups (13 vs 12 days, p-value 0.7) [22]. Langenbach MR et al., compared three meshes (polypropylene, smooth polypropylene and composite) in TAPP hernia repair [23]. The results showed a delayed return to work with the use of standard polypropylene mesh (38.1 days vs 32.6 days vs 33.5 days, p-value < 0.05). Another study by the same group [24] sometime later compared the results in a randomized trial by doing a 60 month follow up. They reported similar findings with a p-value of 0.02.
Limitation
Our study had its limitations of a small sample size and short duration of study period.
Conclusion
Use of composite meshes in laparoscopic inguinal hernia repair is associated with greater patient satisfaction in terms of less postoperative pain and earlier return to work activities, thereby decreasing the morbidity and economic burden. However, more and longer duration of studies are required to further justify their unanimous usage in current surgical practice.