Vision impairment and blindness in children resulting in decreased productivity in the long term remains a challenge to healthcare policy makers. Studies report 16.3% to 37% of blindness in Indian children as avoidable [1,2]. URE still causes majority of the vision impairment seen in Indian children [3].
The SES program was set up by the National Program for Control of Blindness in 1994 to address this need where trained teachers are supposed to conduct the screening however URE still remains a public health problem in India including South India [4].
We decided to explore the current prevalence of this problem in school children from sixth to ninth grades in rural Tamil Nadu, India, with a view to screen for children with uncorrected visual acuity <20/40, assess response to referral, determine prevalence of refractive error and finally determine the NNS to find a child with vision impairment/blindness form hitherto URE in this age group.
Materials and Methods
This was a school-based cross-sectional study carried out in the Kaniyambadi block of Vellore district in the year 2011 after securing permission from the District Education Officer. The district has 83 villages having a total population of over 1 lakh individuals. Of the 70 government schools, 22 schools had sixth to ninth grades. Children in sixth to ninth grades in all these 22 schools who were willing to participate were included in the study; this age group was chosen because they are adolescents who are likely to have progressive myopia and can understand the procedures with respect to screening. Parents were informed through heads of schools.
The screening was carried out between June 2011 and August 2011 in the 22 government schools; those identified in screening with possible visual deficit were referred to the Department of Ophthalmology.
The study was approved by the Institutional Ethics and Review Board and conformed to the Declaration of Helsinki and the ethical guidelines for biomedical research on human participants enunciated by the Indian Council of Medical Research.
Visual acuity screening was done by assessing the uncorrected visual acuity at distance by E-optotypes (equivalent to 20/40 of Snellen’s acuity) by a team consisting of an ophthalmologist (Principal investigator) and an optometrist with an experience in the field of optometry for five years. Based on the ability of the child to identify these optotypes, child was either declared “seeing” or “not seeing”. This cut off has been previously alluded to as being a good screening tool for school screening [5].
All students not seeing 20/40 E-optotype were referred to undergo a comprehensive eye check on Saturdays in the Department of Ophthalmology (base hospital), which included assessment of uncorrected and best corrected visual acuity using Snellen’s visual acuity charts for distance, retinoscopy (Heine) refraction under cycloplegia, slit lamp examination of anterior segment, media, fundus and intraocular pressure measurement. A letter with information in Tamil regarding the child’s problem was sent to the parents of all those referred and further every class teacher was given a list of names of children who were referred to encourage them to bring the child for further evaluation. For children being evaluated in the hospital, assent from child and informed consent from the parent or guardian who accompanied the child was obtained.
If the child needed spectacles after the above examination, prescription of glasses along with first pair of spectacles alone was provided free of charge.
After the initial screening of all the government schools, the number of children who came to the eye hospital for confirmation of refractive error was few. To assess the validity of the screening, the two larger of the 22 schools were revisited and children referred from the initial screening who had not come to the hospital were comprehensively examined and spectacles provided in the school itself. They underwent all the components of the comprehensive examination as done in the base hospital, the only difference being the use of a hand held slit lamp (HEINE HSL 150) for anterior segment assessment and Tonopen XL (MEDRONIC SOLAN) for measurement of intraocular pressure. Since, there were no false positives among the children who screened positive from these two schools, we did not find it necessary to revisit all the other 20 schools.
For the purposes of this study: ‘blindness’ was uncorrected visual acuity less than 20/200 in the better eye; ‘low vision’ was similarly 20/200 or better but less than 20/60. Significant refractive error was: myopia of less than -0.5D, hypermetropia of more than +2D, astigmatism cylindrical error of more than 0.75D. Amblyopia was defined as unilateral or bilateral subnormal vision, at least two lines less than normal or two lines less than the fellow eye in unilateral cases [6].
Where p= prevalence of visual acuity of 20/40 or worse in atleast one eye which is around 5% [7,8].
q=100-p =95
d = 20% of p
If half was due to refractive error (in the study 53% of these were from refractive error) [8] the size required to study for prevalence of refractive error would be 3800 students.
Statistical Analysis
The results were analysed using SPSS Version 17.
Results
Twenty two government schools from Kaniyambadi block were studied, where total number of children on the rolls between sixth to ninth grades was 4739. Of these, 4138 (87.3%) were present on the days of screening. The mean age was 12.39 years (SD 1.26).
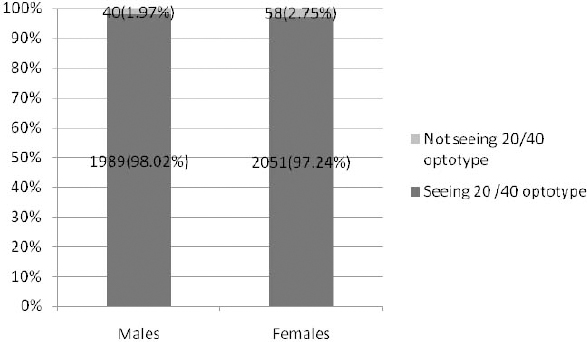
There were 2029 (49%) boys and 2109 (51%) girls. The number of children who could not see the 20/40 optotype with one or both eyes unaided was 98; 40 (40.82 %) boys and 58 (59.18%) girls. There was no statistically significant difference (p=0.1) in the proportion of male and female children who could not see the 20/40 optotype on screening as shown in [Table/Fig-1].
Distribution of screening outcomes by gender among children screened (N=4138).
Chi-square 2.704, (p 0.1)
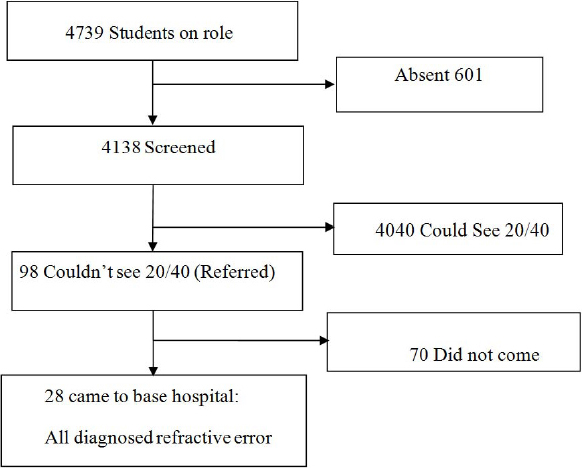
Prevalence of children unable to see the 20/40 optotype in either eye (uncorrected) was (98 of 4138) 2.30% (95% CI 1.834 to 2.766). They were all referred to the base hospital. Only 28 (28.57%) of those referred came to the base hospital for comprehensive eye check up, all of whom were confirmed to have refractive error as shown in [Table/Fig-2a].
In two of the larger schools which contributed 1322 of the 4138 children screened, 29 children had been referred to the base hospital with suspected visual deficit. Of these only 12 had presented to the hospital for confirmation. The remaining 17 children were provided a comprehensive examination at the school. All 29 children were confirmed to have visual deficits as shown in [Table/Fig-2b] and provided refractive correction with spectacles.
Flow of study after revisiting 2 of 22 schools.
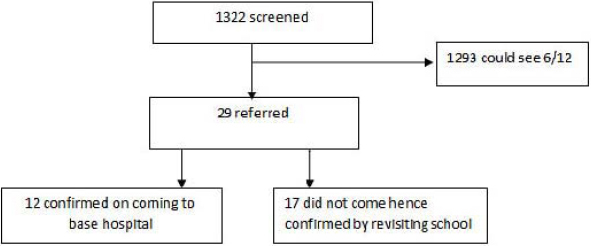
Since, there were no false positives among those referred from these two schools, it indicates near 100% specificity for using 20/40 optotype as a screening tool. Prevalence of refractive error in these two revisited schools was (29 x 100/ 1322) 2.19% (95% CI 1.73 – 2.65) which is the realistic estimate. As revisiting the two schools confirmed another 17 cases in addition to the original 28 cases, there were a total of 45 cases of refractive error diagnosed and treated in the study. Therefore, the prevalence of refractive error in all studied was: 45×100/4138 = 1.09% (95% CI =0.77 to 1.41).
Using the definition for childhood blindness (visual acuity less than 6/60 in the better eye) for presenting visual acuity [9] among the 4138 screened, 3 (0.07%) children were blind and 19 (0.46%) had low vision.
In the revisited schools, (n=1322), among children with no previous history of spectacle wear, we found one blind child from refractive error (high myopia), and eight with low vision. Therefore, we needed to screen 1322 children to find one hitherto undiagnosed child with avoidable blindness. If we now included the ones with low vision, the NNS becomes 1322/ (8+1) which is equal to 147 children. In other words, we need to screen 147 school children studying in grades sixth to ninth to detect one child with low vision or blindness. Among the confirmed cases, 18 (40%) of them had myopia, 25 (55.5%) of them had myopic astigmatism and two (4.44%) of them were found to have hypermetropic astigmatism.
Eight (17.7%) of the 45 alone were previously diagnosed with a refractive error and gave a history of spectacle wear (which included children previously screened at schools or examined elsewhere) and 37 of them were newly diagnosed cases of refractive error. Two (4.4%) of the 45 patients gave a history of being examined previously. Amblyopia was the most common comorbidity seen among six (13.3%) students with refractive errors.
Among the students with refractive errors, one was a diagnosed and treated case of congenital glaucoma under control, one other had a corneal opacity as a result of corneal tear suturing, two had squint for which they were referred to the squint clinic for further management and a fifth had lattice degenerations in the periphery of the fundus not requiring further treatment. The rest of the 40 cases had no significant ocular comorbidities at the time of examination.
Discussion
This cross-sectional study highlights prevalence of refractive errors, spectacle use, low vision and blindness among school children in sixth to ninth grades in a rural block. “The Refractive Error Study in Children (RESC)” reported population (children aged 5 to 15 years) based prevalence of presenting visual acuity ≤ 20/40 in both eyes in urban and rural India as 7.4% and 4.9% respectively with 81% and 53% of this being due to refractive errors [7]. Kariapatti paediatric eye evaluation project in children (0-15 years) of rural South India reported prevalence of refractive errors to be 0.55%, (95% CI: 0.41, 0.69) [10].
School based studies are summarized in [Table/Fig-3], they report prevalence between 2.6% to 8.8% [11-14].
Studies on refractive error in Indian high school children.
| Authors | Place | Year | Age/ grade | Sample size | Screening cut off for uncorrected visual acuity | Prevalence of refractive error % | Myopia (as a% of all RE) |
|---|
| Pavithra MB et al., [11] | Bangaluru, Karnataka | 2013 | 7-15 yrs | 1378 (urban + rural) | (<6/12) | 7.03 | 62.6 |
| Warad C et al., [12] | Davangere Karnataka | 2013 - 14 | 5-7 grade | 7496 | (<6/9) | 6.4 | 82.6 |
| Rahman M et al., [13] | Dibrugarh, Assam | 2013 - 14 | 10-15 yrs | 600 | (<6/6) | 8.83 | 81 |
| Padhye AS et al., [14] | Pune/ Solapur Maharashtra | 2004 - 05 | 6-15 yrs | Urban 5021 Rural 7401 | (<6/12) | 5.46 2.63 | 57.9 55 |
| Our study | Vellore, Tamil Nadu | 2011 | 6-9 grade | 4138 (rural) | (<6/12) | 2.2 | 40 |
Prevalence of uncorrected visual acuity of worse than 20/40 in our study was 2.3%. This is comparable to the prevalence noted in the population based study in children aged 7-15 years in urban area of Ahmedabad, Gujarat, India, which found prevalence of uncorrected visual acuity of 20/40 or worse in the better eye to be 2.7% [15]. It is also comparable to the prevalence noted in school children of rural Maharashtra (2.6%) [14] and rural Cambodia(2.5%) [16]. Prevalence was lower when compared to the study done in Hyderabad which estimated the prevalence of refractive error among children aged 3-18 years to be 3.1% [17]. The difference in the prevalence can be attributed partly to different populations studied and also due to different age groups and different methodologies, techniques and different definitions used to measure refractive error.
Among the children with refractive error, prevalence of myopia was 40% and astigmatism was 60% in our study, when compared to the prevalence that has been reported in a population based study done in rural India in which among the total screened, myopia was seen in 8.4%, and astigmatism ≥ 0.50D and ≥ 1.25D in 10.3% and 2.4% of the children respectively.
The occurrence of myopia was more among females 11 (61.1%) when compared to males seven (36.8%) in our study and the occurrence of astigmatism was also noted to be more among females 15 (55.6%) when compared to males 12 (44.4%) which was similar to the result of Czepita D et al., [18]. The most important cause of uncorrectable visual loss in our study was found to be amblyopia, (13.3%) mostly caused by refractive errors which is comparable with the results of population based study of Gujarat (12%) [15].
From the program perspective, we need to screen only 147 school children from sixth to ninth grades to find one child with low vision or blindness. Considering that these children were around 12-year-old, they have a huge number of person years ahead of them.
The specificity of using 20/40 Snellen’s optotype (performed by a trained ophthalmologist/optometrist) as a cut off was near 100% in our study, similar to that recommended by Saxena R et al., [5]. In the light of this, the SES program should move to using this for the screening protocol from the current 20 /30. Since we had not re-examined all children who saw the 20/40 optotype, we are unable to comment on the sensitivity in this exercise. However, as the children had seen the single line tumbling E-optotype randomly presented they were unlikely to be false negatives.
Of the 45 cases of refractive error in all the schools, 37 (82.2%) were not previously diagnosed with a refractive error. This issue has not been reported in other studies for making comparisons.
Only 28% of those referred for complete evaluation came to the hospital, this could be a potential barrier to any screening program in these children which will require completion of evaluation at the school itself.
Modelling has shown primary eye care to be more cost effective than school based screening [19]. However, further research is required to ascertain which is better. The mobile clinic model has also been used from the primary care set up to improve follow up of those failing the initial screening at the school [20]. This will perhaps be a better way to integrate SES with the general School Health program of which it is meant to be part of after addressing barriers to uptake of spectacle wear [21].
These factors validate the need for vision screening of school children in most parts of the country and the developing world. Thus, screening could serve a useful purpose in detecting correctable causes of decreased vision early in life and minimizing long term permanent visual disability. As significant proportion of children are not going to school in rural India and other parts of the developing world, a more complete assessment of visual impairment in children would be possible with population based studies not restricted to school children.
Limitation
As 12.68% of the children on rolls were absent on the days of screening, if this was due to low vision or blindness, our study would have missed that. The low response to referral from screening formed a limitation which was overcome in only two of the 22 schools. It was not possible to ascertain sensitivity of the screening tool.
Conclusion
The low NNS substantiates the need for continued screening. The screening tool used should be the 20/40 optotype. Monitoring and evaluation of the School Eye Screening program SES needs to be done by the NPCB. The poor response rate of referrals highlights the need to strengthen the follow up component by ensuring that those children identified on screening are assessed, dispensed spectacles and followed up in the school itself.