Decreased Foetal Movements Secondary to Uterine Septum: A Case Report and Proposed Algorithm of Management
Eram Ali1, Tamkin Khan2, Deeba Khanam3
1 Senior Resident, Department of Obstetrics and Gynaecology, Jawaharlal Nehru Medical College, Aligarh, Uttar Pradesh, India.
2 Professor, Department of Obstetrics and Gynaecology, Jawaharlal Nehru Medical College, Aligarh, Uttar Pradesh, India.
3 Assistant Professor, Department of Obstetrics and Gynaecologya, Jawaharlal Nehru Medical College, Aligarh, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Eram Ali, Senior Resident, Department of Obstetrics and Gynaecology, Jawaharlal Nehru Medical College, Aligarh-202002, Uttar Pradesh, India.
E-mail: eramali1987@gmail.com
Congenital uterine anomaly has been well established as cause of infertility and recurrent pregnancy loss. However, only few studies have reported the association of mullerian anomalies and adverse pregnancy outcome in third trimester. We are hereby reporting a case of 25-year- old female second gravida who presented at 36 weeks six days pregnancy with complaint of decreased foetal movements for the past two weeks. The female had previous history of multiple admissions on account of decreased foetal movements in the third trimester. Ultrasonography for biophysical profile and cardiotocography were done on each admission which revealed normal findings. Decision to terminate the pregnancy was taken because of persistent decreased foetal movements. She was induced with dinoprostone gel 0.5 mg intracervically; however she underwent lower segment caesarean section on account of non reassuring cardiotocography. Peroperative findings confirmed the presence of partial uterine septum.
Mullerian anomaly, Non reassuring cardiotocography, Reduced foetal movements
Case Report
A 25-year-old female second gravida with one live deliver with previous one lower segment caesarean section at 36 weeks six days pregnancy reported to the emergency with chief complaint of decreased foetal movements for the past two weeks. Patient perceived 3-4 foetal movements per day in last two weeks.
On examination her vitals were normal. Her systemic examination revealed no positive abnormal finding. On per abdominal examination uterine height was corresponding to term pregnancy and foetal heart rate was regular, cardiotocography was done which showed accelerations of foetal heart rate coinciding with foetal movements, indicating healthy foetus with normally functioning autonomic nervous system. However, patient was not able to feel any movement during the cardiotocography. In view of this and to rule out additional risk factor, ultrasonography was undertaken. Ultrasonography revealed amniotic fluid volume of 15, expected baby weight of 3.1 kilogram and manning score of 10/10.
Patient was unsatisfied after sonographic confirmation of foetal well being saying that the movements are not good enough as earlier. This was followed by repeated admissions for the same complaint three times a week.
Similar complaint of decreased foetal movement was also present in her previous pregnancy. At that time she was induced with three doses of dinoprostone gel 0.5 mg which was followed by syntocinon augmentation. However, she had undergone lower segment caesarean section due to foetal distress but she was not informed about the uterine anomaly at that time.
Keeping a track of foetal movement and responding to change in movement as first line of defence against still birth and perinatal hypoxia, decision was taken to induce the patient with dinoprost gel at 37 weeks four days after well informed patient consent. After receiving two doses at eight hour interval, patient was taken up for lower segment caesarean section in view of non reassuring cardiotocography. Peroperative findings revealed partial uterine septum. Birth weight of the foetus was 3.1 kg with APGAR score of 6,8,10 at 0, 1, and 5 minute respectively. Both mother and baby were healthy in post operative period.
Discussion
Incidence of mullerian duct anomaly is 1-3% in women. [1] Literature have reported septate uterus as one of the most common types of mullerian anomaly [1]. Uterine septum may be incomplete in which wedge-like partition may involve only the superior part of the cavity. Less frequently, it may involve the whole length of the uterine cavity (complete septum) or even cervix leading to morphologically double cervix. This septation may also continue into the vagina resulting in a double vagina. Serosal surface of the uterus is usually normal but less commonly may have a groove or indurations. [1] Congenital uterine anomaly has been well established as cause of infertility and recurrent pregnancy loss [2]. However, only few studies [2,3] have reported the adverse pregnancy outcome of mullerian anomaly in third trimester which include pre term labour, pre term premature rupture of membrane, placenta previa, breech presentation, and caesarean section. Compared with the rest of the uterus, septal tissue has been shown to have decreased vascular supply and abnormal overlying endometrium. [4, 5]
In a study reported by Fedele et al on 42 patients over reproductive outcomes with complete septate uterus, spontaneous abortion rate of 27%, preterm delivery rate of 12%, term delivery rate of 61%, and live birth rate of 72% have been identified [4]. Sometimes the condition may not be detected in the affected individual as it may not cause any reproductive problem as is the case being presented here. However, pregnancy in partial uterine septum presenting with recurrent episodes of decreased foetal movements has not been reported till now in literature. In our case, the lady underwent repeated admissions on account of decreased foetal movements. Ultrasonography for biophysical profile and cardiotocography were done on each admission which revealed normal findings.
Foetal movements may be defined as any discrete kick, flutter, swish or roll perceived after 18 weeks of pregnancy [6]. Any reduction in foetal movements is a potentially important clinical sign indicating foetal distress or even impending foetal death. Studies have reported that around 55% of women with still births had history of reduced foetal movements prior to diagnosis of still birth. Women with reduced foetal movement on two or more occasion are twice at risk of poor perinatal outcome as compared to those who experience it on only one occasion [7].
Foetal movements are often a variable and subjective phenomenon depending upon perception of pregnant mother; this is the reason why a clear definition for it does not exist in literature. Reduced foetal movements in septate uterus have not been mentioned in literature; however, its mechanism seems to be very obvious. Implantation and initial phase of embryonic development in septate uterus if at all occurs usually in a normal way. However, reduced space in septate uterine cavity does not provide enough space for developed foetus for free movements. Intra uterine growth retardation and limb deformity are some other outcomes of this reduced space in septate uterus which has been mentioned in literature [8]. Few authors have mentioned abnormal uterine blood flow and decreased muscle mass as a cause of Intrauterine Growth Restriction (IUGR) in septate uterus and other uterine anomalies [9].
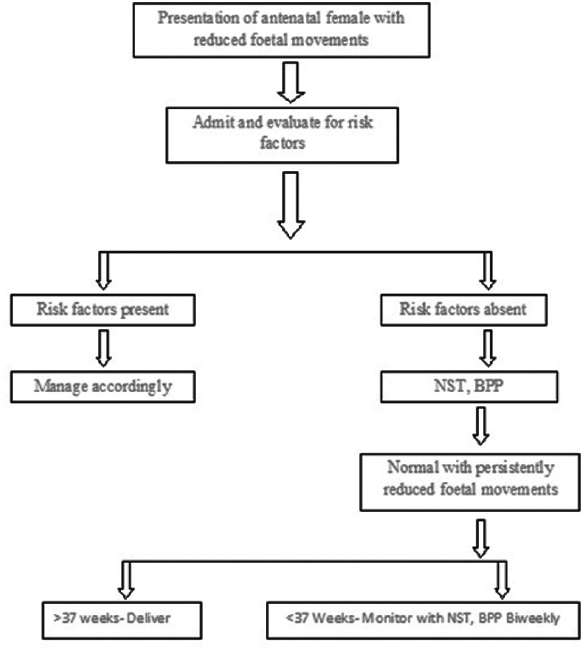
Various authors have proposed a definite algorithm [7] for the management of patients with reduced foetal movements. Simplified algorithm for the mother presenting with reduced perception of foetal movements is hereby mentioned [Table/Fig-1].
Algorithm for the mother presenting with reduced perception of foetal movements. NST: Non Stress Test, BPP: Biophysical Profile.
As regard to septate uterus three-dimensional ultrasonography (transvaginal) is an extremely sensitive tool for the diagnosis of uterine septum and other congenital mullerian anomalies [10]. However, it is useful only in the interpregnancy interval or in very early pregnancy. Two-dimensional ultrasound has low precision in differentiating between arcuate, bicornuate and septate anomaly due to restricted view and focus on uterine fundus [11]. In our case the diagnosis was missed as she reported to us late in pregnancy so final diagnosis was made on per operative findings.
Surgical treatment for uterine septum is indicated in women with recurrent pregnancy loss. Hysteroscopic septoplasty has low morbidity with excellent outcomes and is advocated by many [12]. In asymptomatic patients with incidental diagnosis of uterine septum treatment guidelines are disputed with few authors in favour of surgical resection to avoid future pregnancy related complications while others advocating to leave septum as such [13]. In our case we did not remove the septum to avoid complicating the emergency caesarean section with sepsis and post partum haemorrhage.
Conclusion
Patient presenting with persistent decreased foetal movement should undergo repeated evaluation. Mullerian anomalies including septate uterus can be one of the various differential diagnosis for persistent perception of decreased foetal movements, especially with healthy foetus on evaluation. Approach of management depends on foetal risk factors and period of gestation.
[1]. Heinonen PK, Complete septate uterus with longitudinal vaginal septumFertil Steril 2006 85(3):700-705. [Google Scholar]
[2]. Reichman D, Lauger MR, Robinson BK, Pregnancy outcomes in unicornuate uteri: a reviewFertil Steril 2009 91:1886-94. [Google Scholar]
[3]. Akar ME, Bayar D, Yildiz S, Reproductive outcome of women with unicornuate uterusAust N Z J Obstet Gynaecol 2005 45:148-50. [Google Scholar]
[4]. Fedele L, Bianchi S, Marchini M, Ultrastructural aspects of endometrium in infertile women with septate uterusFertil Steril 1996 65:750-752. [Google Scholar]
[5]. Dabirashrafi H, Bahadori M, Mohammad K, Septate uterus: new idea on the histologic features of the septum in this abnormal uterusAm J Obstet Gynecol 1995 172:105-107. [Google Scholar]
[6]. Efkarpidis S, Alexopoulos E, Kean L, Liu D, Fay T, Case-control study of factors associated with intrauterine fetal deathsMedGenMed 2004 6:53 [Google Scholar]
[7]. O’Sullivan O, Stephen G, Martindale E, Heazell AE, Predicting poor perinatal outcome in women who present with decreased fetal movementsJ Obstet Gynaecol 2009 29:705-10. [Google Scholar]
[8]. Adesiyun AG, Avidime S, Umar H, Akafa R, Aliyu R, Term Pregnancy in a Patient with Septate Uterus: Incidental Finding at Caesarean SectionCase Reports in Clinical Medicine 2014 3:114-117. [Google Scholar]
[9]. Moutos D, Damewood M, Schlaff W, A comparison of the reproductive outcome between women with a unicornuate uterus and women with a didelphic uterusFertil Steril 1992 58:88-93. [Google Scholar]
[10]. Faivre E, Fernandez H, Deffieux X, Gervaise A, Frydman R, Levaillant JM, Accuracy of Three Dimensional Ultrasonography in Differential Diagnosis of Septate and Bicornuate Uterus Compared with Office Hysteroscopy and Pelvic Magnetic Resonance ImagingJournal of Minimally Invasive Gynecology 2012 19:101-10. [Google Scholar]
[11]. Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH, Diagnosis of Uterine Anomalies: Relative Accuracy of MR Imaging, Endovaginal Sonography and HysterosalpingographyRadiology 1992 183:795-800. [Google Scholar]
[12]. Homer HA, Li TC, Cooke ID, The Septate Uterus: A Review of Management and Reproductive OutcomeFertility and Sterility 2000 73:1-14. [Google Scholar]
[13]. Ozgur K, Isikoglu M, Donmez L, Oehninger S, Is Hysteroscopic Correction of an Incomplete Uterine Septum Justified Prior to IVF?Reproductive BioMedicine Online 2007 14:335-340. [Google Scholar]