Spontaneous Intracranial Hypotension
Ankit Balani1, Sandhya Shantilal Sarjare2, Amit Kumar Dey3, Anjani D Kumar4, Sapna S Marda5
1 Resident, Department of Radiology, Yashoda Hospital, Secunderabad, Telangana, India.
2 Resident, Department of Radiology, Yashoda Hospital, Secunderabad, Telangana, India.
3 Intern, Department of Radiology, Seth GS Medical College and KEM Hospital, Parel, Mumbai, Maharashtra, India.
4 Consultant, Department of Radiology, Yashoda Hospital, Secunderabad, Telangana, India.
5 Consultant, Department of Radiology, Yashoda Hospital, Secunderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amit Kumar Dey, Intern, Department of Radiology, Seth GS Medical College and KEM Hospital, Parel, Mumbai-400012, Maharashtra, India.
E-mail: amit5kem@gmail.com
Computed tomography, Headache, Magnetic resonance imaging
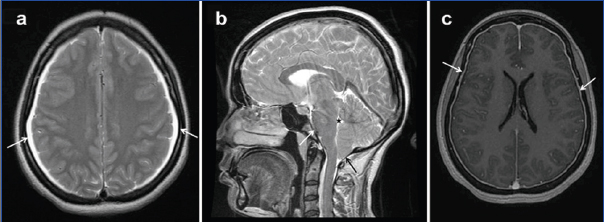
A 34-year-old female patient presented to the outpatient department of our hospital with long standing history of occipital headache for almost five years. The headache was diffuse, dull in nature and was relieved in recumbent position. There was no other significant medical or surgical history. Her physical examination was unremarkable. Headache generally worsened within 20 minutes of assuming the upright position. MRI brain was advised which revealed bilateral thin subdural collections extending along the entire cerebral convexities [Table/Fig-1a]. There was downward displacement (sagging) of the brainstem with tonsillar herniation and effacement of prepontine cistern and fourth ventricle [Table/Fig-1b]. Gadolinium enhanced MRI showed diffuse pachymeningeal enhancement with venous engorgement [Table/Fig-1c]. Computed Tomography (CT) myelography failed to reveal any obvious leak. A diagnosis of Spontaneous Intracranial Hypotension (SIH) was suggested. The patient was treated conservatively with adequate bed rest, oral intake of surplus fluids and increased salt intake in the diet. The symptoms were significantly relieved on three months follow up.
a) MRI brain revealed bilateral thin subdural collections extending along the entire cerebral convexities (arrows); b) MRI brain showed downward displacement (sagging) of the brainstem with tonsillar herniation (black arrow) and effacement of prepontine cistern (white arrow) and 4th ventricle (asterisk); c) Gadolinium enhanced MRI showed diffuse pachymeningeal enhancement (arrows) with venous engorgement.
SIH generally occurs due to spontaneous dural tear and is usually triggered by lumbar puncture, spinal surgery, trauma, sexual intercourse, sneezing or even bending down [1]. One third of cases have a history of trauma and in the remaining two thirds of cases, physical examination usually shows evidence of a connective tissue disorder. SIH headache is often misdiagnosed as aseptic meningitis, subarachnoid haemorrhage, subdural haematoma, Chiari Type I malformation with cerebellar tonsillar herniation, or secondary to intracranial hypertension [1]. Although not as definite as MRI, CT shows subdural fluid collections or obliteration of subarachnoid cisterns and ventricular collapse. Radionuclide cisternography has been used extensively in the evaluation of SIH too but with limited consistency. Typically in SIH, Cerebrospinal Fluid (CSF) opening pressure is less than 60 mm H2O and can be unmeasurable. However, some patients have normal CSF opening pressures. Examination of CSF often demonstrates a primarily lymphocytic pleocytosis, an elevated protein content (up to 1000 mg/dL), or xanthochromia. Typically, lumbar puncture is contraindicated in cases with SIH [2].
Conservative approach consists of bed rest, oral hydration and use of an abdominal binder. Administration of steroids, intravenous caffeine or theophylline all have been advocated but their effectiveness is limited. Surgical treatment is reserved for those patients in whom these nonsurgical measures have failed. The mainstay of treatment is the so called epidural blood patch [2,3]. This case highlights the typical imaging findings of SIH which is a rare cause of positional headache usually remains undiagnosed unless an MRI is done.
[1]. Vaghela V, Hingwala DR, Kapilamoorthy TR, Kesavadas C, Thomas B, Spontaneous intracranial hypo and hypertensions: an imaging reviewNeurol India 2011 59(4):506-12. [Google Scholar]
[2]. Schievink WI, Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotensionJAMA 2006 295(19):2286-96. [Google Scholar]
[3]. Davidson B, Nassiri F, Mansouri A, Badhiwala J, Witiw C, Shamji M, Spontaneous intracranial hypotension: A review and introduction of an algorithm for managementWorld Neurosurgery 2017 101:343-49. [Google Scholar]