Ghost Cell Odontogenic Carcinoma Arising Denovo with Distant Metastasis: A Case Report and Review of Literature
Madhurya Namana1, Sumit Majumdar2, Divya Uppala3, Aditya Avv4, Ayyagari Kameswara Rao5
1 Postgraduate Student, Department of Oral Pathology, GITAM Dental College and Hospital, Visakhapatnam, Andhra Pradesh, India.
2 Head, Department of Oral Pathology, GITAM Dental College and Hospital, Visakhapatnam, Andhra Pradesh, India.
3 Reader, Department of Oral Pathology, GITAM Dental College and Hospital, Visakhapatnam, Andhra Pradesh, India.
4 Postgraduate Student, Department of Oral Pathology, GITAM Dental College and Hospital, Visakhapatnam, Andhra Pradesh, India.
5 Dental Assistant Surgeon, Community Health Center, APVVP, Vizianagaram, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ayyagari kameswara Rao, P.S.R. Colony, Vizianagaram-535002, Andhra Pradesh, India.
E-mail: calmua@gmail.com
Ghost Cell Odontogenic Carcinoma (GCOC) is a rare malignant odontogenic tumour of epithelial origin accounting about 0.37% to 2.1% of all odontogenic tumours. They are characterized by the presence of ameloblastic islands along with ghost cells representing aberrant keratinization. The aim of this case report is to present a rare case that was diagnosed in a 37-year-old male patient and to describe the behavior of the tumour.
Ameloblastic, Fatal case, Nodal and distant metastasis, Tumour
Case Report
A 37-year-old male patient visited the outpatient department with a chief complaint of pain in the lower right back tooth region since 4 months associated with swelling. Extraoral facial asymmetry was noted with extraoral swelling pushing the mandibular lower border [Table/Fig-1]. Right submandibular lymph node was fixed. Intraorally, an ill-defined, ulcer was noted in the mandibular right alveolar mucosa [Table/Fig-2] in the lower right back tooth region extending anteroposteriorly from distal aspect of 45 to the distal aspect of 47 involving the retromolar area, mesiodistally extending 0.5 cm on either side of the alveolar ridge. Ulcer was non-healing as patient gave history of previous extraction of mobile mandibular molars two months back. His panoramic radiograph revealed multilocular radiolucency extending anteroposteriorly from distal surface of 44 to 47 [Table/Fig-3].
Extraoral figure demonstrating swelling of the mandibular lower border.

Intraoral figure demonstrating an ill-defined, ulcer in the mandibular right alveolar mucosa.

Panoramic radiograph demonstrating multilocular radiolucency.

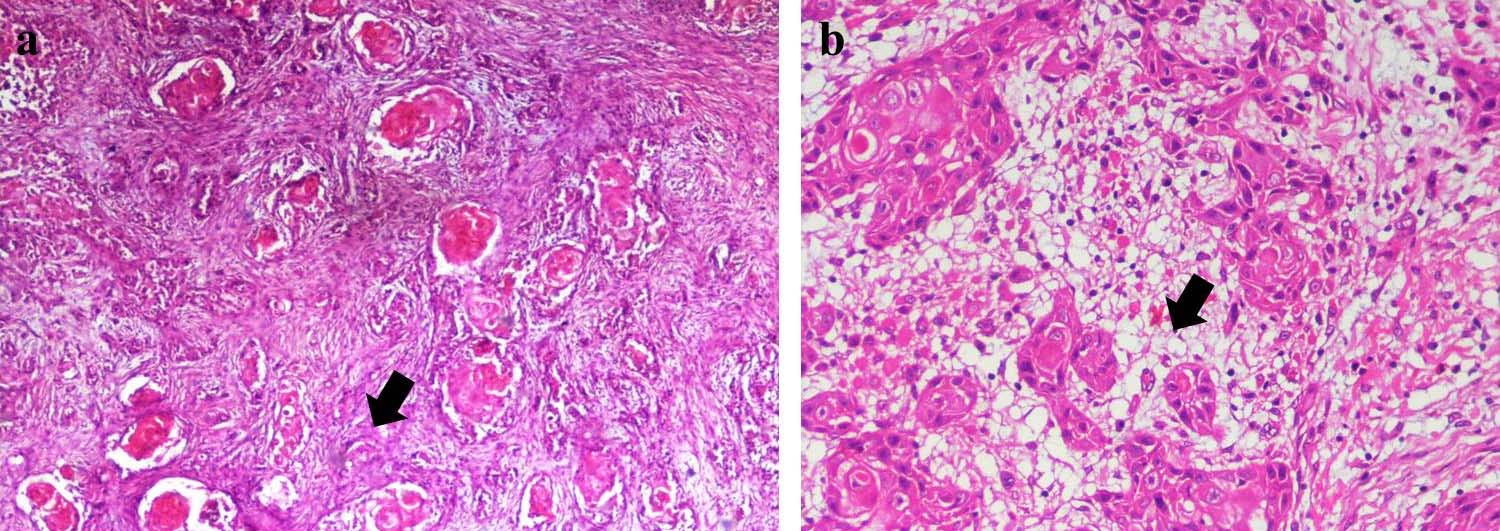
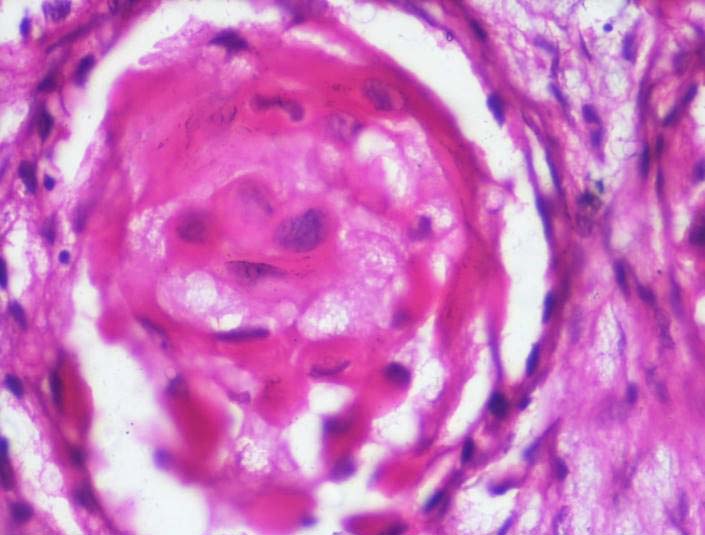
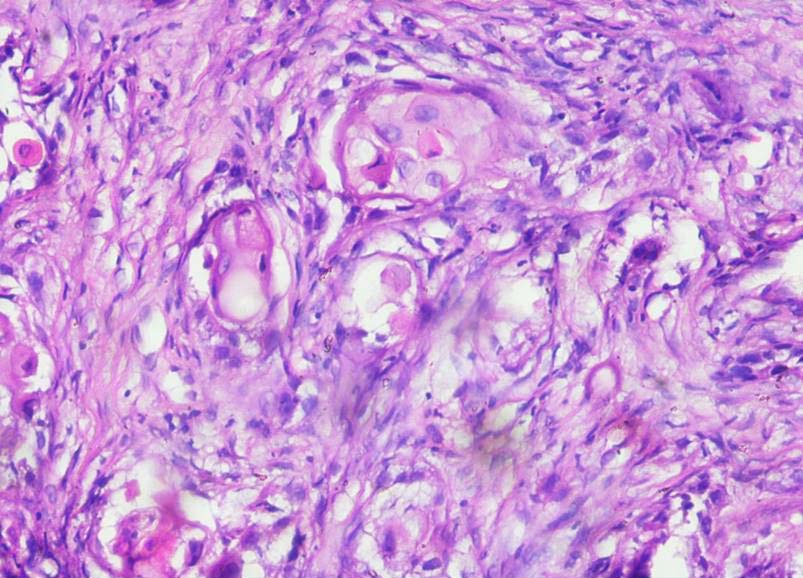
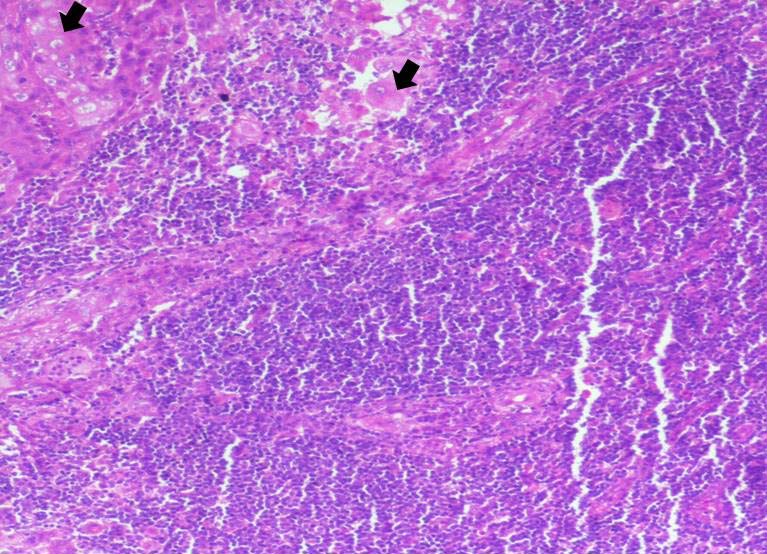
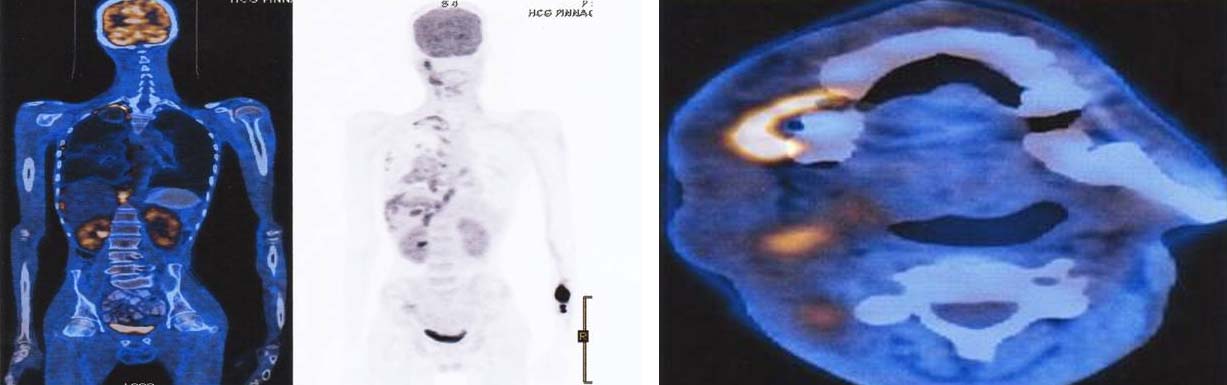
Incisional biopsy was taken under local anesthesia. Histopathologically, the hematoxylin and eosin stained section exhibited proliferation of odontogenic epithelial cells arranged in whorled and streaming pattern [Table/Fig-4a] and also clear cells [Table/Fig-4b]. Pale, swollen, eosinophilic cells were seen singly and in sheets containing nuclear and cytoplasmic organellar remnants [Table/Fig-5]. Odontogenic epithelial cells showed nuclear hyperchromatism, nuclear and cellular pleomorphism [Table/Fig-6]. A diagnosis of GCOC was made and radical neck dissection was done along with hemimandibulectomy. Level 1 and Level 2 lymph nodes also showed the metastatic ghost cells [Table/Fig-7] for which radiotherapy was also done. Patient was under continuous follow up, after one year of the treatment PET–CT scan was done which revealed poorly marginated metabolically active lesion in the gingivobuccal sulcus with erosions of adjacent maxilla suggestive of early recurrence of the disease, poorly marginated metabolically active soft tissues in the submental, right neck and posterior neck regions, extensive pleural and fissural right lung nodules suggestive of metastatic deposits [Table/Fig-8]. Before any further treatment could be started, patient expired.
a) Demonstrating odontogenic epithelial cells (arrows) arranged in whorled and streaming pattern (H&E 4X); b) Demonstrating clear cells (arrows) along with odontogenic islands (H&E 10X).
Demonstrating ghost cells (H&E 40X).
Demonstrating odontogenic epithelial cells with nuclear hyperchromatism, nuclear and cellular pleomorphism (H&E 10X).
Demonstrating metastatic ghost cells (arrow) in lymph nodes (H&E 4X).
PET –CT scan demonstrating poorly marginated metabolically active lesions in the gingivobuccal sulcus, submental, right neck and posterior neck, pleural and fissural right lung regions.
Discussion
GCOCs are malignant odontogenic tumours of epithelial origin [1]. They may arise de novo most commonly or from pre-existing Calcifying Odontogenic Cyst (COC), Calcifying Cystic Odontogenic Tumour (CCOT), Dentinogenic Ghost Cell Tumour (DGCT). WHO in 2005 classified GCOC under malignant odontogenic tumours of epithelial origin. GCOCs are designated with various terminologies including malignant COC, odontogenic ghost cell carcinoma, carcinoma arising in a COC, aggressive epithelial ghost cell odontogenic tumour, dentinogenic ghost cell ameloblastoma and malignant calcifying ghost cell odontogenic tumour [2]. These tumours are exclusively seen in intraosseous location, occurrence of approximately 7% in the head and neck region [1,2]. Their incidence in the oral cavity is about 0.37% to 2.1% of all odontogenic tumours. They occur most commonly in maxilla accounting for 67% [1].
Very few cases are reported in literature involving the mandible. First case though not well documented was reported by Pindborg in 1971 in Spanish, detail case report was presented by IKemura et al., in 1985 [2]. A thorough search was performed in PUB MED using the keywords such as “Ghost cell,” “Odontogenic carcinoma,” and “metasatic/” in various combinations. Till date, 34 cases have been reported [Table/Fig-9] and so this case manifests as a very rare entity [1-24]. Mean age of tumour was 37.3 years which is similar to the present case. The tumour has slight male predilection. Most of the cases reported were observed in Asiatic regions [1,3,4,25]. Many patients presented with pain, swelling and paresthesia, which were consistant with the chief complaint of patient in the present case. Radiographic features include a poorly demarcated radiolucency mixed with radiopacities [26]. Biological behavior of the tumour is unpredictable, as some tumours were indolent while in many they were aggressive and recurrences were high. Local recurrence and metastasis was observed [25]. In a study done by Lu Y et al., most common site of metastasis was lung, which was also observed in the present case. Some patients expired within one year and many patients were disease free even for 17 years, although the tumour recurred many times [2]. A 5-year survival rate was 73% [2]. Histologically GCOC is characterized by the presence of rounded, irregularly shaped tumour islands. Small basaloid epithelial cells with a sparse eosinophilic cytoplasm and rounded, dark, moderately pleomorphic nucleoli are seen along with varying sized islands of ghost cells. Ghost cells are not pathognomic of GCOC but are also observed in odontogenic lesions like COC, CCOT, DGCT, odontomas, amelobalstoma and also in craniopharyngiomas and pilomatricomas which are of non-odontogenic origin [27]. Ghost cells are large polygonal cells with homogeneous pale eosinophilic cytoplasm. The nuclei may be totally disintegrated and in some cases, remnants of chromatin may be seen. They represent aberrant keratinization as they show intense staining with high molecular weight keratins and reduced staining with involucrin. Various amounts of dystrophic calcification in the ghost cells are also seen. Clear cells may be admixed with the ghost cells as in the present case. The ghost cells differ from normal keratotic squames where the former appear larger, often vacuolated and the remnants of nuclear membranes are more prominent. Mitotic figures and necrosis within the central area of tumour islands is common [28]. Ghost cells do not express cytokeratins but express AE1/AE3 and 34bE12, indicating their antigenic alteration. Main stay of treatment for these tumours is surgical excision. It should be excised completely with tumour free wide surgical margins followed by radiotherapy and vigorous follow up [23].
| S.No | Author/ Reference | Sex/age | Site |
|---|
| 1. | Fernández MM et al., [1] | M/70 | Maxilla |
| 2. | Lu Y et al., [2] | M/45 | Maxilla |
| 3. | Ali EHM et al., [3] | M/21 | Maxilla |
| 4. | Rappaport MJ et al., [4] | F/64 | Mandible |
| 5. | Rappaport MJ et al., [4] | M/55 | Maxilla |
| 6. | Ikemura K et al., [5] | M/48 | Mandible |
| 7. | Ellis GL and Shmookler BM [6] | F/55 | Mandible |
| 8. | Ellis GL and Shmookler BM [6] | M/17 | Maxilla |
| 9. | Ellis GL and Shmookler BM [6] | M/46 | Maxilla |
| 10. | Grodjesk JE et al., [7] | M/46 | Maxilla |
| 11. | Scott J and Wood GD [8] | M/33 | Maxilla |
| 12. | McCoy BP et al., [9] | M/13 | Maxilla |
| 13. | Dubiel-Bigaj M et al., [10] | M/42 | Maxilla |
| 14. | Siar CH and Ng KH [11] | M/39 | Maxilla |
| 15. | Alcalde RE et al., [12] | F/72 | Maxilla |
| 16. | Lu Y et al., [13] | M/20 | Maxilla |
| 17. | Lu Y et al., [13] | M/24 | Maxilla |
| 18. | Lu Y et al., [13] | F/31 | Maxilla |
| 19. | Lu Y et al., [13] | M/19 | Maxilla |
| 20. | Lu Y et al., [13] | M/39 | Mandible |
| 21. | Kamijo R et al., [14] | M/38 | Maxilla |
| 22. | Kim HJ et al., [15] | M/33 | Mandible |
| 23. | Li TJ and Yu SF [16] | M/43 | Maxilla |
| 24. | Cheng Y et al., [17] | M/58 | Mandible |
| 25. | Cheng Y et al., [17] | M/70 | Maxilla |
| 26. | Cheng Y et al., [17] | M/50 | Maxilla |
| 27. | Cheng Y et al., [17] | M/50 | Mandible |
| 28. | Goldenberg D et al., [18] | M/36 | Maxilla |
| 29. | Sun ZJ et al., [19] | M/30 | Maxilla |
| 30. | Roh GS et al., [20] | M/55 | Mandible |
| 31. | Slama A et al., [21] | M/89 | Mandible |
| 32. | Li BH et al., [22] | M/47 | Mandible |
| 33. | Zhu ZY et al., [23] | M/51 | Maxilla |
| 34. | Arashiyama T et al., [24] | M/68 | Mandible |
| 35. | Present case | M/40 | Mandible |
Conclusion
Present case emphasized the biological behavior of GCOC. Adequate biopsy with meticulous histopathological examination of the multiple sections along with adjunctive IHC is the key for the definitive diagnosis to differentiate from conventional squamous cell carcinoma. As recurrence and metastasis are very frequent with GCOC, follow up for a long period should be advised.
[1]. Fernández MM, Ferranti MA, Madrid JAH, Atín CB, Ghost cell odontogenic carcinoma: A case report and review of literatureJ Clin Exp Dent 2014 6(5):e602-06. [Google Scholar]
[2]. Lu Y, Mock D, Takata T, Jordan RC, Odontogenic ghost cell carcinoma: report of four new cases and review of the literatureJ Oral Pathol Med 1999 28(7):323-29. [Google Scholar]
[3]. Ali EHM, karrar MA, El-Siddig AA, Gafer N, Satir AA, Ghost cell odontogenic carcinoma of the maxilla: A case report with a literature reviewPan Afr Med J 2015 21(260):01-06. [Google Scholar]
[4]. Rappaport MJ, Showell DL, Edenfield WJ, Metastatic ghost cell odontogenic carcinoma: description of a case and search for actionable targetsRare Tumours 2015 7(3):5813 [Google Scholar]
[5]. Ikemura K, Horie A, Tashiro H, Simultaneous occurrence of calcifying odontogenic cyst and its malignant transformationCancer 1985 56:2861-64. [Google Scholar]
[6]. Ellis GL, Shmookler BM, Aggressive (malignant?) epithelial odontogenic ghost cell tumourOral Surg Oral Med Oral Pathol 1986 61:471-78. [Google Scholar]
[7]. Grodjesk JE, Dolinsky HB, Schneider LC, Odontogenic ghost cell carcinomaOral Surg Oral Med Oral Pathol 1987 63:576-81. [Google Scholar]
[8]. Scott J, Wood GD, Aggressive calcifying odontogenic cyst: A possible variant of ameloblastomaBr J Oral Maxillofac Surg 1989 27:53-59. [Google Scholar]
[9]. McCoy BP, O’Carroll MK, Hall JM, Carcinoma arising in a dentinogenic ghost cell tumourOral Surg Oral Med Oral Pathol 1992 74:371-78. [Google Scholar]
[10]. Dubiel-Bigaj M, Olszewski E, Stachura J, The malignant form of calcifying odontogenic cyst: A case reportPatologia Polska 1993 44:39-41. [Google Scholar]
[11]. Siar CH, Ng KH, Aggressive (malignant?) epithelial odontogenic ghost cell tumour of maxillaJ Laryngol Otol 1994 108:269-71. [Google Scholar]
[12]. Alcalde RE, Sasaki A, Misaki M, Odontogenic ghost cell carcinoma: Report of a case and review of literatureJ Oral Maxillofac Surg 1996 54:108-11. [Google Scholar]
[13]. Lu Y, Mock D, Takata T, Jordan R, Odontogenic ghost cell carcinoma: report of four new cases and review of the literatureJ Oral Pathol Med 1999 28:323-29. [Google Scholar]
[14]. Kamijo R, Miyaoka K, Tacbikawa T, Odontogenic ghost cell carcinoma: report of a caseJ Oral Maxillofac Surg 1999 57:1266-70. [Google Scholar]
[15]. Kim HJ, Choi SK, Lee CJ, Such CH, Aggressive epithelial odontogenic ghost cell tumour in the mandible: CT and MR imaging findingsAJNR Am J Neuroradiol 2001 22:175-79. [Google Scholar]
[16]. Li TJ, Yu SF, Clinicopathologic spectrum of the so-called calcifying odontogenic cyst: A study of 21 intraosseous cases with reconsideration of the terminology and classificationAm J Surg Pathol 2004 27:372-84. [Google Scholar]
[17]. Cheng Y, Long X, Li X, Bian Z, Chen X, Yang X, Clinical and radiological features of odontogenic ghost cell carcinoma: review of the literature and report of four new casesDentomaxillofac Rad 2004 33(3):152-57. [Google Scholar]
[18]. Goldenberg D, Sciubba J, Koch W, Tufano RP, Odontogenic ghost cell carcinomaHead Neck 2004 26:378-81. [Google Scholar]
[19]. Sun ZJ, Zhao YF, Zhank L, Li ZB, Chen XM, Zhang WF, Odontogenic ghost cell carcinoma in the maxilla: a case report and literature reviewJ Oral Maxillofac Sur 2007 65:1820-24. [Google Scholar]
[20]. Roh GS, Jeon BT, Parket B, Ghost cellodontogenic carcinoma of the mandible: a case report demonstrating expression of tartrate-resistant acid phosphatase (TRAP) and vitronectin receptorJ Oral Maxillofac Surg 2008 36:419-23. [Google Scholar]
[21]. Slama A, Boujelbène N, Ben Yacoub L, Trabelsi A, Khochtali H, Sriha B, Odontogenic carcinoma with ghost cells of the mandibleRev Stomatol Chir Maxillofac 2010 111(3):158-61. [Google Scholar]
[22]. Li BH, Cho Y, Kim S, Kim MJ, Hong SP, Lee JH, Recurrent odontogenic ghost cell carcinoma (OGCC) at a reconstructed fibular flap: a case report with immunohistochemical findingsMed Oral Patol Oral Cir Bucal 2011 16:651-56. [Google Scholar]
[23]. Zhu ZY, Chu ZG, Chen Y, Ghost cell odontogenic carcinoma arising from calcifying cystic odontogenic tumour: a case reportKorean J Pathol 2012 46:478-82. [Google Scholar]
[24]. Arashiyama T, Kodama Y, Kobayashi T, Ghost cell odontogenic carcinoma arising in the background of a benign calcifying cystic odontogenic tumour of the mandibleOral Surg Oral Med and Oral Pathol 2012 114:35-40. [Google Scholar]
[25]. Sukumaran R, Somanathan T, Kattoor J, Odontogenic ghost cell carcinoma with pulmonary metastasisJOMFP 2015 19(3):371-74. [Google Scholar]
[26]. Barnes L, Eveson JW, Reichart P, Sidransky D, World Health Organization classification of tumours: Pathology and genetics of head and neck tumours 2005 LyonIARC Press:293-95. [Google Scholar]
[27]. Mehendiratta M, Bishen KA, Boaz K, Mathias Y, Ghost cells: A journey in the darkDent Res J 2012 9(Suppl 1):S1-S8. [Google Scholar]
[28]. Leon Barnes, Surgical pathology of head and neck 2009 3rd edNew yorkInforma Health care:67 [Google Scholar]