Mediastinal Teratoma with Pulmonary Parenchyma Fistula: A Rare Diagnostic Endeavour
Dharma Ram1, Deepak Kumar Sharma2, LM Darlong3, Suhas K Rajappa4, Yogendra Singh Bhakuni5
1 Attending Consultant, Department of Surgical Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi, India.
2 Senior Resident, Department of Thoracic Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi, India.
3 Senior Consultant, Department of Thoracic Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi, India.
4 Attending Consultant, Department of Surgical Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi, India.
5 DNB Resident, Department of Surgical Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dharma Ram, Attending Consultant, Department of Surgical Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi-110085, India.
E-mail: drdharmapoonia@gmail.com
Teratoma is the most frequent mediastinal germ cell tumour amongst young population. They are often detected due to pressure symptoms or as an incidental finding on chest X-ray done for any other reason. Mediastinal teratoma is usually benign and rarely possesses diagnostic or therapeutic challenge unless they rupture into surrounding viscera. In such scenario, they may lead to acute life threatening condition and need prompt diagnosis and surgical extirpation. Here, we are reporting our experience of managing a young lady, who presented with short duration breathing difficulty and cough, and was diagnosed with ruptured mediastinal teratoma on imaging, which was further confirmed intraoperatively and histopathologically.
Extirpation, Mass, Pulmonary fistula, Ruptured
Case Report
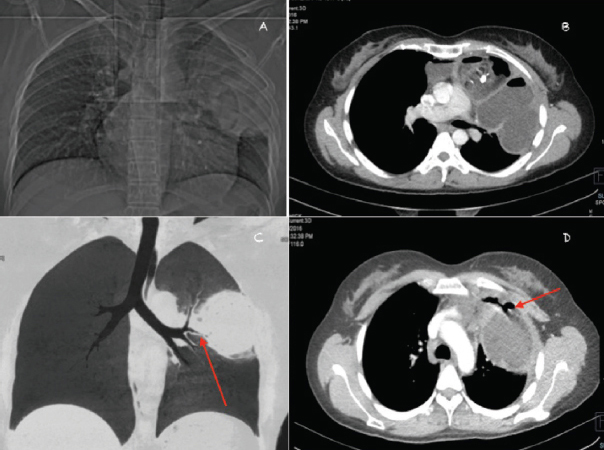
A 27-year-old female presented to thoracic outpatient clinic with complains of breathing difficulty, cough and pain in back of 2-weeks duration. Her physical examination revealed reduced air entry in left upper lung field with no evidence of toxaemia. Chest X-ray showed large left upper zone opacity. CT chest showed well circumscribed anterior mediastinal mass with internal fat fluid level and calcified component with evidence of localised rupture to anterior segment of left upper lobe of lung showing air fluid level. Lesion was inseparable from pericardium medially and chest wall laterally with fistulous tract between left upper lobe intra parenchymal component and anterior mediastinal mass, likely mature teratoma with pulmonary parenchymal fistula [Table/Fig-1]. Diagnostic bronchoscopy did not show any endobronchial abnormality. The provisional diagnosis of mediastinal teratoma with pulmonary parenchyma fistula was made.
a) Topogram revealing encapsulated left paramediastinal opacity with internal air and calcific foci associated with left upper zone consolidation; b) Axial post contrast CT image revealing encapsulated anterior mediastinal lesion with internal fat fluid level and calcified component with evidence of localised rupture to anterior segment of left upper lobe of lung showing air fluid level; c) Coronal lung window image with minimum intensity projection showing left upper lobe lesion and relation of involved lung segment with anterior segmental bronchus of left upper lobe (arrow); d) Axial post contrast CT image showing fistulous tract between left upper lobe intra parenchymal component and anterior mediastinal mass (arrow).
Tumour markers (AFP, hCG and LDH) were within normal limits. Abdominal USG was done to evaluate the retroperitoneum and gonads, which showed bilateral ovarian simple cysts and was negative for retroperitoneal lymph nodes. Gynaecological opinion was taken and patient was planned for diagnostic laparoscopy during definitive surgery. On laparoscopy, benign looking left ovarian cyst was seen, for which laparoscopic drainage was done. Midline sternotomy was done for the mediastinal mass. There was a large multilobulated anterior mediastinal mass with left phrenic nerve invasion. The whole of left upper lobe was replaced by cystic mass leaving thin rim of lung parenchyma in the apico-posterior segment and lingua with focal infiltration. Non anatomical stapled resection of the left upper lobe was done to remove the mass en block. Perioperative period was uneventful.
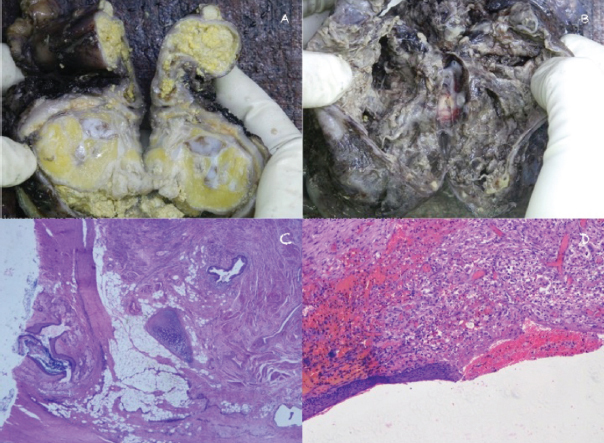
On gross pathological examination, a solid cystic mass containing pultaceous material with hair was noted. On microscopic analysis multiple components derived from all three germ cell layers in variable proportion was noted, suggesting mature cystic teratoma with a ruptured and infiltrative interface with lung, measuring 6×2 cm area with cystic areas [Table/Fig-2]. Patient was kept on regular follow up and was well six months after the surgery.
a) Cut section of mediastinal mass with areas of pultaceous material; b) Cystic lesion into lung with ragged margins; c) Haphazardly arranged skin with adenexal structures, mature hyaline cartilage, skeletal muscle and adipose tissue fragments (H&E,2X); d) Ulcerated cyst wall lining, partially lined by stratified squamous epithelium with subepithelial congestion and foreign body reaction (H&E, 10X).
Discussion
Mature teratoma is one of the most common causes of anterior mediastinal mass in young females. More than half of them are asymptomatic and the usual presentation is incidentally detected mass on chest radiography [1,2]. Rarely, they may also present with acute onset symptoms due to rupture into surrounding organs like lung, chest wall, and pericardium or rarely skin [1-3].
Pulmonary parenchymal or airway involvement of mediastinal teratoma is rare occurrence and variably labelled as pulmonary rupture or Pulmonary Parenchymal Teratoma Fistula (PPTF). The cause of these events is largely elusive and speculative including autolysis, ischaemia, infection and inflammation [2,4,5]. They pose diagnostic and therapeutic challenges.
The patient often presents with sudden onset of breathing difficulty. The differential diagnosis includes teratoma with secondary lung abscess, chemical pneumonitis and Intra Pulmonary Teratoma (IPT) [5-8]. The definitive differentiation is not always possible preoperatively particularly from large IPT. It is difficult to differentiate the two when a large mediastinal teratoma extends into the lungs [5,6].
The diagnostic clue includes acute onset of symptoms like breath-lessness and haemoptysis, mass infiltrating into lung parenchyma, mass infiltrating airways, air fluid levels in imaging, and documentation of intraluminal growth/defect with hair bronchoscopically. Teratoma with lung abscess is often associated with sign of toxaemia and more constitutional symptoms than other two conditions.
The ultimate diagnosis is often possible intraoperatively [2,4-8]. We were lucky to document PPTF on preoperative imaging, which is not always possible. Clinical history and examination, imaging with astute judgment help in the management of such cases. The basic principle is timely judgement for surgical intervention to prevent life threatening consequences. The clinical, bronchoscopic and imaging differentials are depicted in [Table/Fig-3].
Differentiating features of mediastinal teratoma, ruptured/Pulmonary Parenchymal Teratoma Fistula (PPTF), Intra Pulmonary Teratoma (IPT) and teratoma with lung abscess.
| Factor | Unruptured mediastinal teratoma | Ruptured/(PPTF) | Intra Pulmonary Teratoma (IPT) | Teratoma with lung abscess |
|---|
| Clinically | Young adult Asymptomatic Incidental | Young adult Almost always symptomatic | Children Often symptomatic Extremely rare | Young adult Always symptomatic Sign of toxemia |
| Imaging | Small masses | Large masses | Small masses | Variable size |
| Pushing and compressing adjacent structures | Infiltration to surrounding structure | Multi lobulated well contained mass within lung parenchyma | No specific findings |
| Homogeneity of their internal contents of each compartment | Inhomogeneous contents. | - | - |
| Air Fluid Level (AFL) uncommon | AFL found often | AFL level common | AFL common |
| Pleural effusion Uncommon | Pleural effusion > 57% cases | Pleural effusion uncommon | - |
| Bronchoscopy | Normal | Content/ defect may be visible | Content/defect may be visible | Non specific |
The surgical extirpation is not straight forward in these cases. The surgical challenges include pleural symphysis, dense adhesions to vital mediastinal structures such as the phrenic nerve, vena cava, pulmonary, aortic vessels, pericardium and lung due to inflammation and infiltration of ruptured teratoma [1,3]. In our case dense adhesions were noted intra operatively, which required careful mobilisation and partial excision of the pericardium. Phrenic nerve was sacrificed as it was engulfed in the tumour along with non anatomical wedge resection of the left upper lobe.
Conclusion
Ruptured mediastinal teratoma is a very rare event and poses a diagnostic challenge to the treating physician. As definitive diagnosis is not always possible preoperatively, the prompt decision making and desired surgical intervention, is the key to manage this challenging scenario.
[1]. Serraj M, Lakranbi M, Ghalimi J, Ouadnouni Y, Smahi M, Mediastinal mature teratoma with complex rupture into the lung, bronchus and skin: A case reportWorld Journal of Surgical Oncology 2013 11:125-27. [Google Scholar]
[2]. Choi SJ, Lee JS, Song KS, Lim TH, Mediastinal teratoma: CT differentiation of ruptured and unruptured tumoursAJR Am J Roentgenol 1998 171(3):591-94. [Google Scholar]
[3]. Chen RFC, Chang TH, Chang CC, Lee CN, Mediastinal teratoma with pulmonary involvement presenting as massive haemoptysis in 2 patientsRespiratory Care 2010 55:1094-96. [Google Scholar]
[4]. Bachh AA, Haq I, Gupta R, Boinapally RM, Sudhakar S, Benign mediastinal teratoma with intrapulmonary extension presenting with trichoptysisRespir Med CME 2010 3(3):189-91. [Google Scholar]
[5]. Sawant AC, Kandra A, Narra SR, Intrapulmonary cystic teratoma mimicking malignant pulmonary neoplasmBMJ Case Reports 2012 10:1136 [Google Scholar]
[6]. Morgan DE, Sanders C, Mcelvein RB, Intrapulmonary teratoma:? a case report and review of the literatureJ Thorac Imaging 1992 7:70-77. [Google Scholar]
[7]. Saini ML, Krishnamurthy S, Kumar RV, Intrapulmonary mature teratomaDiagn Pathol [Internet] 2006 1(1):38 [Google Scholar]
[8]. Pikin O, Kolbanov K, Kazakevich V, Korolev A, Mediastinal mature cystic teratoma perforating into the lungInteractive Cardiovascular and Thoracic Surgery 2010 11(6):827-29. [Google Scholar]