Esthesioneuroblastoma Presenting with Bilateral Proptosis and Blindness in a Child: A Case Report
Mahdi Shahriari1, Nader Shakibazad2, Mehrpour Moradi3
1 Associate Professor, Department of Paediatrics, Division of Paediatric Haematology and Oncology, Shiraz University of Medical Sciences, Shiraz, Fars, Iran.
2 Paediatric Oncology and Haematology Fellow, Department of Paediatrics, Division of Paediatric Haematology and Oncology, Shiraz University of Medical Sciences, Shiraz, Fars, Iran.
3 Paediatric Oncology and Haematology Fellow, Department of Paediatrics, Division of Paediatric Haematology and Oncology, Shiraz University of Medical Sciences, Shiraz, Fars, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nader Shakibazad, Paediatric Oncology and Haematology Fellow, Department of Paediatrics, Division of Paediatric Haematology and Oncology, Shiraz University of Medical Sciences, Shiraz, Fars, Iran.
E-mail: nshakibazad@gmail.com
Esthesioneuroblastoma is a rare malignant tumour of the olfactory epithelium. The most common symptom is related to unilateral nasal obstruction. It rarely presents with bilateral proptosis and blindness. We report a 21-month-old girl with esthesioneuroblastoma in sphenoid and ethmoid sinus in a child presenting with bilateral proptosis, blindness, and irritability. The diagnosis was confirmed by histopathology.
Exophthalmos, Olfactory neuroblastoma, Sinus tumour, Visual loss
Case Report
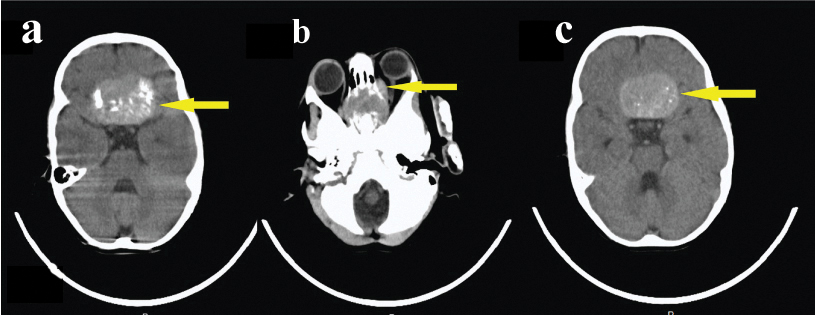
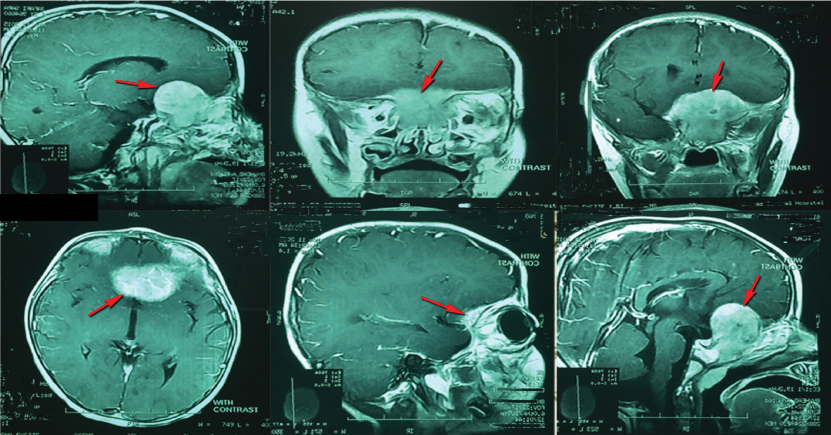
A 21-month-old girl presented with bilateral proptosis, blindness, and irritability since 15 days prior to admission. She was referred to the Paediatric Oncologist with the suspicion of rhabdomyosarcoma. On eye examination by ophthalmologist excessive lacrimation, decreased vision (light perception), strabismus, extraocular movement, paralysis and pale disc were detected. Her vital signs were normal. Other physical examinations including head circumference, thyroid, liver, and spleen also were normal. The laboratory workups are listed below: White Blood Cells: 5900×103/μL, Haemoglobin: 9.9 gm/dL, Mean Corpuscular Volume: 85 fL, platelets: 463×103/μL, Lactate Dehydrogenase: 712 U/L, Erythrocyte Sedimentation Rate: 28 mm/hr, Alanine Aminotransferase: 53 U/L, Alanine transaminase: 20 U/L. Brain CT scan revealed anterior base skull tumour invading orbit and ethmoid sinuses [Table/Fig-1]. MRI of the brain, orbit, and paranasal sinuses showed enhancing soft tissue mass lesion measuring about 34 mm × 28 mm × 22 mm involving sphenoid sinus and posterior aspect of ethmoid sinuses at the midline of anterior base of skull compressing optic chiasma and nerve and also destroying both orbits [Table/Fig-2].
a, b, and c: Brain CT scan-multiple images in different plains - shows anterior base skull tumour invading orbit and ethmoid sinuses.
Brain MRI- multiple images in different plains- shows a large extra-axial mass measuring about 34 mm ×28 mm ×22 mm arising from the floor of the anterior fossa. It involves sphenoid sinus and posterior aspect of ethmoid sinuses at the midline of the anterior base of skull compressing optic chiasma and nerve and also destroying both orbital cavities.
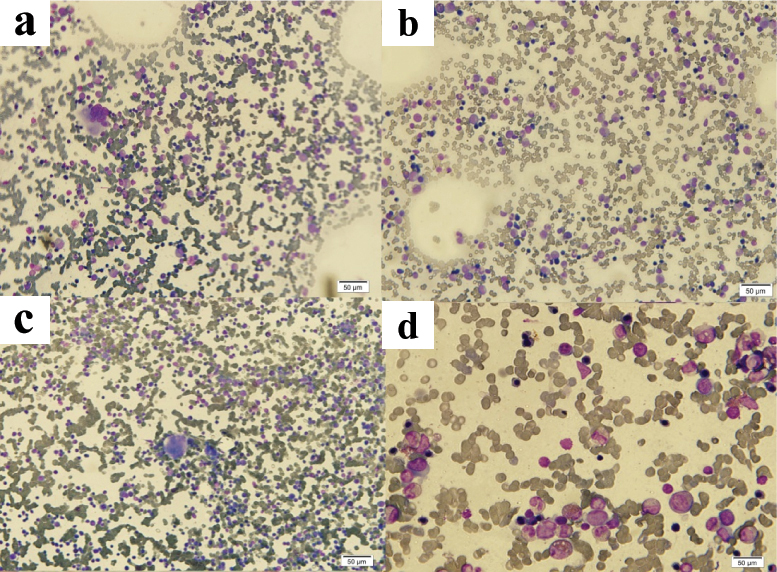
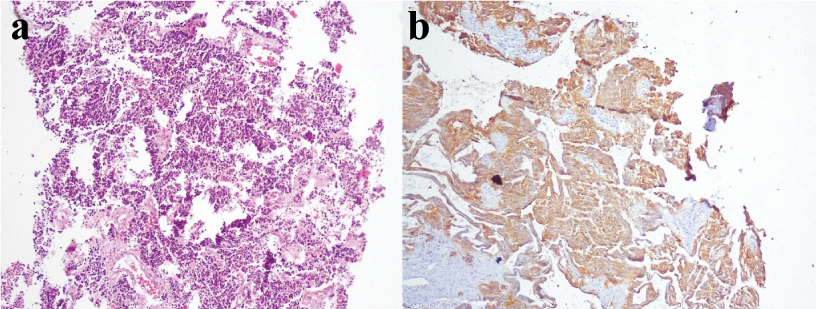
Bilateral bone marrow biopsy and aspiration showed normocellular marrow with no evidence of metastasis [Table/Fig-3]. She was operated by Neurosurgeon and histopathology of the mass [Table/Fig-4] revealed malignant small round cell tumour and Immunohistochemical (IHC) study showed positive chromogranin, cytokeratin, and synaptophysin but S-100, CD99, and EMA were negative [Table/Fig-5]. Ki67 was 80% positive. IHC findings were in favour of olfactory neuroblastoma (esthesioneuroblastoma). The patient was treated with VAC protocol (vincristine, actinomycin-D, and cyclophosphamide) with improvement after receiving four courses of chemotherapy (about four months after diagnosis) but not completely. Her vision and strabismus became better and proptosis also improved. The patient is on regular follow up. It should be noted that written informed consent was taken from her parents before this report.
a, b, c and d shows bone marrow aspiration slides (Hematoxylin and Eosin stain) with polymorphic and normal cellularity, megakaryocyte is adequate, and no cluster of abnormal cells seen (a-20X, b-40X, c-10X, d-100X).
a and b section of brain mass slides which show nice crush artifact of small round cell tumour (H&E), High power and low power- a- 4X, b-10X; c and d section of brain mass slides which show small round cell malignant tumour with high N/C ratio and hyperchromatic nuclei (H&E- c- 10X, d- 40X).
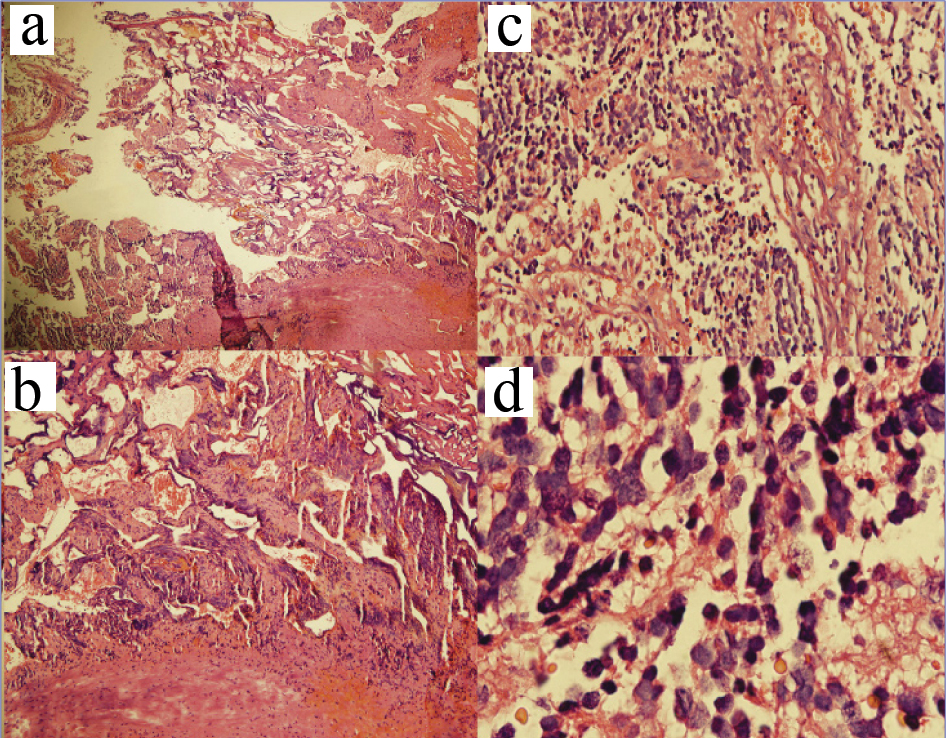
a) Section of brain mass shows small cell malignant tumour with high N/C ratio and hyperchromatic nuclei (H&E, 100X); b) Section of brain mass shows Immunohistochemistry for synaptophysin is positive.
Discussion
Esthesioneuroblastoma is a rare malignant neuroectodermal tumour that originates from the olfactory epithelium. It accounts for about 3% of all sinus tumours [1,2]. The incidence of the tumour is about 0.4-1/1,000,000 population per year and, it can occur at any age with incidence peaks is in the second and fifth decades of life [3]. The most common symptoms of esthesioneuroblastoma are unilateral nasal obstruction and epistaxis [4].
The differential diagnosis of proptosis in children is different from an adult. In the adult, thyroid disease is the most common cause, while in children; orbital cellulitis is the most common cause [5,6]. The common causes of proptosis among paediatric age groups include orbital cellulitis, capillary haemangioma, dermoid cyst, hyperthyroidism and malignancy such as retinoblastoma, rhabdomyosarcoma, optic glioma, myeloid leukaemia, chloroma, lymphoma, histiocytosis, Ewing sarcoma, esthesioneuroblastoma and metastasis [6,7]. Our case presented mainly with orbital manifestations. Symptoms due to local extension of tumour include anosmia due to tumour invasion of cribriform plate, orbital manifestation due to orbital involvement, and otitis media due to blockage of the eustachian tube. The diagnosis often occurs with delay [8-10]. Because some symptoms are non specific and it needs a high index of suspicion.
In our case, according to orbital manifestation and ophthalmology consult, brain lesion affecting chiasma was suspected, therefore imaging study was done and revealed mass lesion. The final diagnosis was done by IHC study on biopsy specimen. Tumour staging in our case according to Kadish system [11] was stage C.
Olfactory neuroblastoma is a soft, polypoid and haemorrhagic mass. Microscopically, it shows a variety of features. Typically it exhibits a lobular shape with overriding highly vascularized fibrous stroma. Tumour cells are monomorphic with the contextual neurofibrillary matrix. The nuclei consist of salt and pepper chromatin. Olfactory neuroblastoma can exhibit mitosis, calcification, and necrosis [12-14].
Three tumours may be confused with esthesioneuroblastoma, which includes sinonasal undifferentiated carcinoma, rhabdomyosarcoma and Ewing sarcoma, they should be differentiated from each other [15]. These tumours can be differentiated by morphology and immunohistochemically. For example, in Ewing sarcoma CD99 is positive, rhabdomyosarcoma shows myogenic marker and sinonasal undifferentiated carcinoma exhibits diffuse positivity of cytokeratin [14].
Treatment includes surgical resection combined with radiotherapy and/or chemotherapy [2, 4]. Esthesioneuroblastoma is an aggressive and chemosensitive tumour in paediatric patients. In children, chemotherapy is preferred modality than invasive surgery [3].
The prevalence of local recurrence in esthesioneuroblastoma is 20%-40% [16]. Relapse may be occurred years after finishing treatment, often happens more than 10 years, thus long term follow up is required [9].
Conclusion
Esthesioneuroblastoma should be differentiated from other malignant tumours even it presents with rare manifestation. A multidisciplinary approach is necessary for better patient care. Regular long term follow up is needed because the rate of local recurrence is high.
[1]. Lopez R, Mazzoni L, Chaput B, Jalbert F, Olfactory neuroblastoma presenting with exclusive orbital manifestationsJ Craniofac Surg 2013 24(2):667-69. [Google Scholar]
[2]. Olmo HR, Stokes SM, Foss RD, Olfactory neuroblastoma: A case reportHead Neck Pathol 2016 10(2):256-60. [Google Scholar]
[3]. Bisogno G, Soloni P, Conte M, Podda M, Ferrari A, Garaventa A, Esthesioneuroblastoma in pediatric and adolescent age. A report from the TREP project in cooperation with the Italian neuroblastoma and soft tissue sarcoma committeesBMC Cancer 2012 12:117 [Google Scholar]
[4]. Uslu GH, Canyilmaz E, Zengin AY, Mungan S, Yoney A, Bahadir O, Olfactory neuroblastoma: A case reportOncol Lett 2015 10(6):3651-54. [Google Scholar]
[5]. Dhir SP, Jain IS, Jain GC, Proptosis in childrenIndian Pediatr 1977 14(6):475-77. [Google Scholar]
[6]. Massoud F, Proptosis; differential diagnosisBr J Ophthalmol 1946 30:622-30. [Google Scholar]
[7]. Rao AA, Naheedy JH, Chen JY, Robbins SL, Ramkumar HL, A clinical update and radiologic review of pediatric orbital and ocular tumoursJ Oncol 2013 2013:975908 [Google Scholar]
[8]. Song CM, Won TB, Lee CH, Kim DY, Rhee CS, Treatment modalities and outcomes of olfactory neuroblastomaLaryngoscope 2012 122(11):2389-95. [Google Scholar]
[9]. Ward PD, Heth JA, Thompson BG, Marentette LJ, Esthesioneuroblastoma: Results and outcomes of a single institution’s experienceSkull Base 2009 19(2):133-40. [Google Scholar]
[10]. Jethanamest D, Morris LG, Sikora AG, Kutler DI, Esthesioneuroblastoma: a population-based analysis of survival and prognostic factorsArch Otolaryngol Head Neck Surg 2007 133(3):276-80. [Google Scholar]
[11]. Kadish S, Goodman M, Wang CC, Olfactory neuroblastoma. A clinical analysis of 17 casesCancer 1976 37(3):1571-76. [Google Scholar]
[12]. Lund VJ, Howard D, Wei W, Spittle M, Olfactory neuroblastoma: past, present, and future?Laryngoscope 2003 113(3):502-07. [Google Scholar]
[13]. Lund VJ, Milroy C, Olfactory neuroblastoma: clinical and pathological aspectsRhinology 1993 31(1):01-06. [Google Scholar]
[14]. Haroon S, Tariq MU, Memon A, Fatima S, Hasan SH, Olfactory neuroblastoma: A clinicopathological experience of a rare entity from PakistanPak J Med Sci 2016 32(3):585-90. [Google Scholar]
[15]. Mezzelani A, Tornielli S, Minoletti F, Pierotti MA, Sozzi G, Pilotti S, Esthesioneuroblastoma is not a member of the primitive peripheral neuroectodermal tumour-Ewing’s groupBr J Cancer 1999 81(4):586-91. [Google Scholar]
[16]. Dulguerov P, Allal AS, Calcaterra TC, Esthesioneuroblastoma: a meta-analysis and reviewLancet Oncol 2001 2(11):683-90. [Google Scholar]