A Huge Ovarian Dermoid Cyst: Successful Laparoscopic Total Excision
Hacer Uyanikoglu1, Abdurrahim Dusak2
1 Assistant Professor, Department of Obstetrics and Gyneacology, Harran University, Sanliurfa, Turkey.
2 Professor, Department of Radiology, Harran University, Sanliurfa, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hacer Uyanikoglu, Harran University Medical Faculty, Sanliurfa-46100, Turkey.
E-mail: huoglu@hotmail.com
Giant ovarian cysts, ≥15 cm in diameter, are quite rare in women of reproductive age. Here, we present a case of ovarian cyst with unusual presentation treated by laparoscopic surgery. On histology, mass was found to be mature cystic teratoma. The diagnostic and management challenges posed by this huge ovarian cyst were discussed in the light of the literature.
Huge ovarian cyst, Laparoscopy, Young woman
CASE REPORT
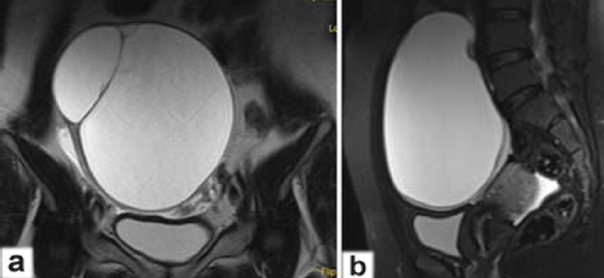
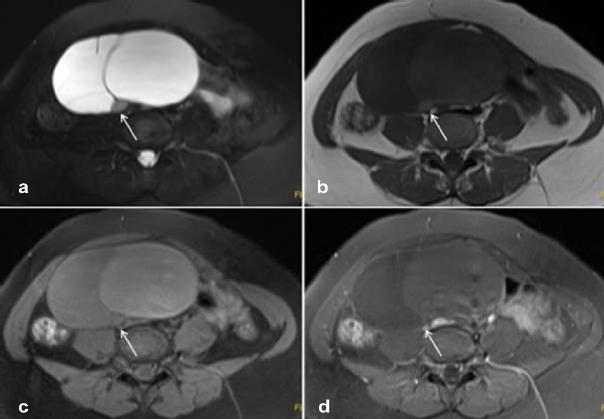
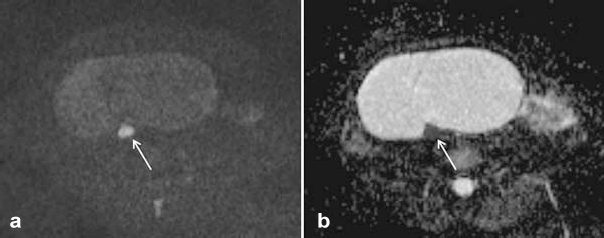
A 28-year-old patient (gravida-0) reported to the Gynaecology Outpatient Department with generalised abdominal pain since a year. The patient’s past obstetrical and gynaecological history was insignificant. She had noticed severe abdominal pain spreading from her left lower quadrant to the umbilicus, since two days. Her past medical history was also unremarkable. Abdominal examination suggested the presence of a tender pelvic mass. Ultrasonographic (USG) examination (Voluson 730 Expert scanner, USA) revealed a semi-homogeneous (cystic with minimal solid areas) 15 x 14 x 10 cm mass, arising from left adnexa containing echogenic material. It was extending from supraumbilical region to pelvis. USG suggested, that consistency of diagnosis with a mature cystic teratoma (dermoid cyst) of the ovary. Magnetic Resonance Imaging (MRI) was also performed to support the diagnosis and evaluate its relation with adjacent organs. MRI of the abdomen revealed a well-defined 15 x 15 x 10 cm left adnexal lesion [Table/Fig-1] with intralesional fat, calcification, and diffusion restricted area involving the left ovary [Table/Fig-2,3] which was diagnosed as an ovarian dermoid. The left ovarian dermoid was adjacent to but not compressing the distal left ureter. Some tumour markers, Ca-125, carcino-embyogenic antigen, and Ca-19.9 were with in normal range. An elective laparoscopic surgery was planned to remove dermoid cyst.
a) Coronal; and b) Sagittal; images revealed a well-defined 15 x 15 x 10 cm left adnexal lesion involving the left ovary.
a) Axial fat saturated T2W; b) T1W; c) fat saturated T1W; and d) contrast enhanced fat saturated T1W images; demonstrated non enhanced with intralesional fat left ovarian cystic lesion.
a) Axial Diffusion W and b) Apparent Diffusion Coefficient (ADC) mapp; images show diffusion restricted area.
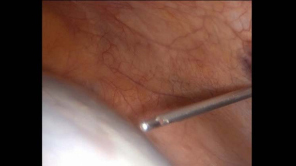
Surgery was performed using a laparoscopic approach with a 10 mm port placed in 3 cm upper from umbilicus through a 10 mm 0-degree telescope. Two 5 mm working ports at the right and left iliac fossae and a 10 mm port at 8 cm upper from left port were placed. The whole peritoneal cavity was seen to confirm the diagnosis, exclude malignancy, and the contralateral ovary was also inspected. The left ovary was consistent with a huge cyst [Table/Fig-4], the right ovary had normal appearance and uterus could not be seen because of the huge cyst. In addition, there was no evidence of torsion or rupture. The wall of the cyst was smooth. Contents of the dermoid cyst (seromucinous fluid and sebaceous material) were aspirated by vacuum aspirator using veress needle [Table/Fig-5] to prevent spillage. In order to excise the cyst wall harmonic scalpel (Ethicon, US) was used on the anti-mesenteric border [Table/Fig-6]. A piece of tissue was removed and sent to pathology department for frozen section. The result was mature cystic teratoma. Then, the collapsed cystic mass was gently removed by peeling from the surrounding ovarian tissue. Ovarian haemostasis was achieved using suture (No.0 vicryl), and the cyst was retrieved with an endo-bag through the 10 mm port site. Spillage of the cyst content into peritoneal cavity did not occur. Nevertheless, abdominal irrigation was applied for the prevention of chemical peritonitis. The abdominal cavity was finally inspected to control haemostasis and the absence of adjacent organ injury.
A huge cyst in left ovary.

Beginning of aspiration procedure of the cyst by veress needle.
Cyst wall excision harmonic scalpel (Ethicon, US).

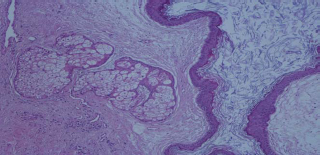
Pathological analysis of the specimen revealed ovarian dermoid cyst. The biggest piece of ovarian cyst measured 10 x 7 x 0.2 cm. Some hair and sebaceous materials were seen in the cyst lumen. Microscopic examination showed no malignant transformation [Table/Fig-7].
Histopathological 100X view shows keratinized epidermis on surface and sebaceous glands in deeper.
The patient recovered uneventfully and was discharged from hospital two days after the surgery. The patient did not have any problems in her follow ups three months later.
DiSCUSSiON
Dermoid cysts are the most common ovarian tumours generally occurring in the second and third decade of life. Giant ones (> 15 cm) are very rare and can be symptomatic. Because of the associated symptoms such as mass effect and the doubt of ovarian malignancy, they usually require resection (mostly as oophorectomy) [1]. Most women with dermoid cysts are asymptomatic. If present, symptoms depend upon the size of the mass. Torsion is common and rupture of dermoid cysts with spillage of sebaceous material into the abdominal cavity can occur, but is uncommon. Shock and haemorrhage are the immediate sequelae of rupture; a marked granulomatous reaction (chemical peritonitis) may subsequently develop and lead to formation of dense adhesions [2].
Imaging modalities are important for the diagnosis of ovarian cysts. Ultrasound allows reasonably accurate non invasive diagnosis in many cases. The reported sensitivity is 85% [3]. The sensitivity of MRI is nearly 100% in ovarian dermoid mass [4]. Nevetheless, definitive diagnosis is made at the time of surgical excision.
The advantages of laparoscopic management in ovarian cysts include lesser postoperative pain, shorter hospitalisation and recovery periods, and better cosmetic consequences, as compared to laparotomy. Several criteria have been reported for laparoscopic management of ovarian cysts such as age of the patient (premenopause), size of the mass (≤ 5 cm), characteristics of the mass on ultrasound, and normal range of tumor markers [5]. Some authors recommended conservative therapy by laparoscopy to preserve ovarian function in young patients with dermoid cyst [6]. Also, Briones-Landa CH et al., demonstrated that laparoscopy did not increase complication rates in comparison with the open approach of benign ovarian cystectomy [7]. We did not consider malignancy in our patient because of the findings of MRI and the normal levels of tumour markers. Thus, we preferred laparoscopic surgery for our patient.
Katke RD suggested that giant cysts require resection because of their compressive symptoms and malignancy risks. However, he recommended that benign cysts should be managed conservatively in young women and requires laparotomy to prevent perforation and spillage of the cyst fluid into the cavity [8]. Conventional treatment of giant ovarian cysts is usually full midline laparotomy, followed by a cystectomy or oophorectomy [1,9]. The midline vertical laparotomy, and the resulting loss of an ovary from this procedure caused both a visible vertical scar and reduce the patient’s fertility capacity. These results of treatment are unacceptable for many younger and nulliparous patients. In our patient, we chose conservative laparoscopic method both to protect her reproductive health and to provide better skin appearence cosmetically.
Chemical peritonitis following dermoid spillage is a very serious complication of laparoscopic extraction of the cyst. Cases of chemical peritonitis with adhesion formation and granulomatosis have been reported following intraperitoneal spillage of cyst contents [10,11]; however, a study has reported the absence of complications with spillage when this was followed by generous irrigation of the abdominal cavity [10]. Because of the rarity of malignancy risk in dermoid cysts, the risk in spillage of malignant cells following the rupture is often minimised [12]. If spillage occurs, complete removal of spilled contents and copious irrigation should be performed to avoid peritonitis. Although peritonitis following rupture of the cyst is very rare, being aware of this complication is the key to appropriate management [6]. Campo S and Garcea N suggested that to minimise spillage of the cyst’s contents and subsequent complications, the surgeon should choose a more effective and less traumatic technique to the patient [10]. In this case, we successfully retrieved the cyst through an endo-bag after aspiration procedure of the cyst. At the same time we applied abdominal lavage to prevent chemical peritonitis. Therefore, chemical peritonitis did not occur after the operation.
Conclusion
We presented a case of complete laparoscopic extirpation of a giant ovarian cyst. Laparoscopic surgery seems to be appropriate and secure for therapeutic management of huge benign ovarian cysts. Because of the laparoscopic approach supplies both conservative treatment and excellent cosmetic results in terms of skin as compared to midline abdominal incision, it should be chosen especially for young and nulliparous women, even if her cyst was huge.
[1]. Dolan MS, Boulanger SC, Salameh JR, Laparoscopic management of giant ovarian cystJSLS 2006 10(2):254-56. [Google Scholar]
[2]. Esmaeili M, Shahbazi S, Seylani K, Nazari N, Ovarian dermoid cyst and neuromuscular manifestationNurs Pract Today 2015 2(4):171-73. [Google Scholar]
[3]. Patel MD, Feldstein VA, Lipson SD, Chen DC, Filly RA, Cystic teratomas of the ovary: diagnostic value of sonographyAJR Am J Roentgenol 1998 171:1061 [Google Scholar]
[4]. Takeda A, Imoto S, Mori M, Yamada J, Nakamura H, Early abdominal pregnancy complicated by parasitic dermoid cyst: diagnosis by diffusion-weighted magnetic resonance imaging and management by laparoendoscopic single-site surgeryJ Minim Invasive Gynaecol 2012 19(5):647-50. [Google Scholar]
[5]. Drolet J, Dubuc-Lisoir J, Guidelines for the laparoscopic management of the adnexal massSOGC 1998 76:1-7. [Google Scholar]
[6]. Tarcoveanu E, Vasilescu A, Georgescu S, Danila N, Bradea C, Lupascu C, Laparoscopic approach to ovarian dermoid cystsChirurgia (Bucur) 2012 107(4):461-68. [Google Scholar]
[7]. Briones-Landa CH, Ayala-Yanez R, Leroy-Lopez L, Anaya-Coeto H, Santarosa-Perez MA, Reyes-Munoz E, Comparison of laparoscopic vs. laparotomy treatment in ovarian teratomasGinecol Obstet Mex 2010 78(10):527-32. [Google Scholar]
[8]. Katke RD, Giant mucinous cystadenocarcinoma of ovary: A case report and review of literatureJ Midlife Health 2016 7(1):41-44. [Google Scholar]
[9]. Mülayim B, Gürakan H, Da-lı V, Mülayim S, Aydin O, Akkaya H, Unaware of a giant serous cyst adenoma: a case reportArch Gynaecol Obstet 2006 273:381-83. [Google Scholar]
[10]. Campo S, Garcea N, Laparoscopic conservative excision of ovarian dermoid cysts with and without an endobagJ Am Assoc Gynaecol Laparosc 1998 5(2):165-70. [Google Scholar]
[11]. Lin P, Falcone T, Tulandi T, Excision of ovarian dermoid cyst by laparoscopy and by laparotomyAm J Obstet Gynaecol 1995 173:769-71. [Google Scholar]
[12]. Mayer C, Miller DM, Ehlen TG, Peritoneal implantation of squamous cell carcinoma following rupture of a dermoid cyst during laparoscopic removalGynaecol Oncol 2002 84(1):180-83. [Google Scholar]