Insulin Injection Site Adverse Effect in a Type 1 Diabetes Patient: An Unusual Presentation
Ranjana Ajit Sahasrabudhe1, Tejas Yashwant Limaye2, Vidya Sanjay Gokhale3
1 Associate Professor, Department of Pharmacology, BVDU Medical College, Pune and Research Fellow, Diabetes Unit, KEM Hospitals, Pune, Maharashtra, India.
2 Senior Research Fellow and Diabetes Educator and Nutritionist, Diabetes Unit, KEM Hospitals Pune, Maharashtra, India.
3 Diabetes Educator and Medical Social Worker, Diabetes Unit, KEM Hospitals, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjana Ajit Sahasrabudhe, 6(45) Vasant Apts, Opp Kothrud Bus Stand, Pune-411038, Maharashtra, India. E-mail : ranjanas2003@yahoo.co.in
Insulin is an integral part of Type 1 diabetes management. Patient education is of utmost importance to ensure proper injection technique for getting appropriate glycaemic control as well as to avoid injection site adverse effects. Commonest injection site adverse effect is lipodystrophy, attributable to localized manifestation of the pharmacological action of insulin. However, we present a case where incorrect injection technique led to an unusual presentation of injection site adverse effect. Apart from the abnormal skin changes, the incorrect technique also adversely affected the glycaemic control. Though less prominent, some marks are still evident one and a half years after correction of the injection technique. However, the glycaemic control has substantially improved. This emphasizes the need of proper patient education regarding insulin injection technique.
Insulin injection technique, Patient education, Skin pigmentation, Site rotation
Case Report
A 14.5-year-old male reported to our clinic in quest of insulin pump. He had type 1 Diabetes Mellitus (DM) since 3.5 years and was on twice daily regimen of premixed human insulin (30% soluble insulin and 70% isophane insulin) along with insulin glargine at bed time. He complained of nausea and had bouts of vomiting, which were attributed by his parents to acidity. General examination showed signs of dehydration like sunken eyes and altered skin turgidity. Urine tested positive for ketones when tested by urine dipsticks and post breakfast Blood Sugar Level (BSL) was 363 mg% by glucometer. Fasting BSL of the same day in the glucometer records was 425 mg%. His weight (43 kg) was low for his age (25th centile - IAP guidelines) [1].
He gave history of persistently high blood sugars, with frequent nausea and vomiting. Hypoglycaemia had never been a problem, except two years ago, when BSL had once dropped to 35 mg%. Reportedly, Self Monitoring of Blood Glucose (SMBG) was being done only intermittently. They were not aware of the need to monitor HbA1c.
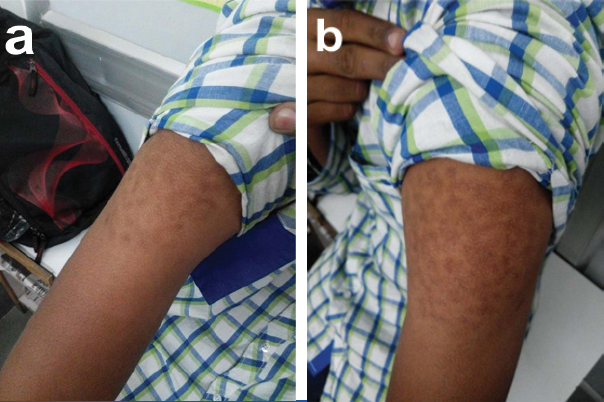
On physical examination, both arms and thighs showed raised areas on injection sites indicating lipohypertrophy. These hypertrophied injection sites also had unusual scar marks showing varied grades of pigmentation [Table/Fig-1].
Affected injection sites showing lipohypertrophy and injection scar marks of varying grades of pigmentation. a) Right arm; b) Left arm; c) Right thigh

Insulin injections were routinely being given by his mother. When “asked” how she held the syringe, she explained that she held the syringe “straight” as she had been “told” at the time of initiation of insulin treatment. When asked to demonstrate, it was evident that she was holding the syringe parallel to the skin. She raised the skin by pinching and inserted the needle parallel to the skin, instead of perpendicular to the skin as required for giving subcutaneous injections.
Actions Taken: The patient and his parents were demonstrated the proper injection technique, including the angle of needle insertion, proper sites for injection and importance and methods of site rotation. Under supervision, the patient was taught to take injections himself. Symptoms of both hyperglycaemia and hypoglycaemia were explained, along with the preventive and corrective actions to be taken. Importance of monitoring HbA1c and SMBG was emphasized. An effort was made to convince them that a pump cannot be a substitute for knowledgeable and active involvement of the patient and his family in the management of Type 1 diabetes.
Outcome and Follow up: The patient has started taking injections himself with the right technique. In the subsequent three follow up visits over six months, BSL improved, with subsequent improvement in physical growth. Patient’s appearance also improved and the perpetual complaint of nausea and vomiting disappeared. One and a half years after correction of the injection technique, injection injury marks appeared faded, but were still visible [Table/Fig-2]. His weight also improved from 43 kg to 55 kg (Improvement from 25th centile to nearly 50th centile - IAP guidelines) [1].
Affected injection sites showing faded injection scar marks 1.5 years after correction of injection technique. a) Right arm; b) Left arm
Discussion
Insulin is the life line for Type 1 DM patients. Inappropriate use of insulin can be hazardous. Since patients are expected to take the injections themselves, proper patient and family education is imperative for optimal management of diabetes [2].
Conventionally, insulin needs to be injected in the subcutaneous fat tissue. Various global and national forums have defined the guidelines for correct injection technique [3,4]. These guidelines form an essential component of patient education at the initiation of insulin treatment. Incorrect injection technique can lead to localized cutaneous reactions like lipodystrophy, which in turn compromise the glycaemic control [5]. Lipohypertrophy is the commonest injection site adverse effect today, with reported prevalence as high as 76% in Type 1 DM patients [6]. Being the local manifestation of insulin action itself, it is not restricted to any particular type of insulin.
In the case reported here, in addition to localized lipohypertrophy, incorrect injection technique resulted in small scars showing abnormal pigmentation at the injection sites as well as poor glycaemic control. Detailed discussion with the mother who had been giving the injections revealed that, at the initiation of insulin treatment, the injection technique had only been explained verbally. She had neither been demonstrated the technique nor asked to inject under supervision. Correctness of the patient’s technique had also never been ensured in follow up visits, resulting in incorrect injections jeopardizing patient’s health. This underlines the need for proper patient education, with injection technique being taught with demonstration and practice under supervision. Correctness of the patient’s technique needs to be confirmed in the subsequent follow up visits.
We came across two other reports of similar skin injury. One report attributed the manifestation to post-inflammatory hyper pigmentation after micro trauma caused due to repeated use of the needle [7]. The other report attributed it to intradermal injections leading to localized insulin allergy, that resolved after switching to subcutaneous injection [8].
The scar marks in our patient have also faded after correcting the injection technique and no new marks have appeared since then. This would implicate faulty injection technique as the cause, though investigations with skin biopsy would throw more light on the aetiology.
Conclusion
Any psychomotor skill like the injection technique needs to be taught by demonstration and actual practice under supervision. Verbal instructions may be misinterpreted, resulting as it did, in our patient, in injurious injections, with poor control of diabetes. Correctness of Injection technique also needs to be ascertained regularly at the follow up visits.
[1]. Khadilkar V, Yadav S, Agrawal KK, Tamboli S, Banerjee M, Cherian A, Revised IAP growth charts for height, weight and body mass index for 5-18 year old Indian childrenIndian Pediatrics 2015 52:47-55. [Google Scholar]
[2]. Shrivastava SR, Shrivastava PS, Ramasamy J, Role of self-care in management of diabetes mellitusJournal of Diabetes and Metabolic Disorders 2013 12:14 [Google Scholar]
[3]. Tandon N, Kalra S, Balhara YPS, Baruah MP, Manoj Chadha M, Chandalia HB, Forum for Injection technique (FIT), India: The Indian recommendations 2.0, for best practice in insulin injection technique 2015IJEM 2015 19(3):317-31. [Google Scholar]
[4]. The Forum for Injection Technique - FIT odcTM International. Accessed on 8th March 2016 from http://www.fit4diabetes.com [Google Scholar]
[5]. TA Chowdhury, V Escudier, Poor glycaemic control caused by insulin lipohypertrophyBMJ 2003 327:383-84. [Google Scholar]
[6]. Blanco M, Hernández MT, Strauss KW, Amaya M, Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetesDiabetes & Metabolism 2013 39:445-53. [Google Scholar]
[7]. GU Sawatkar, S Dogra, S Kumar, Insulin injection: cutaneous adverse effectsIJEM 2015 19(4):533-34. [Google Scholar]
[8]. Sanyal T, Ghosh S, Chowdhury S, Mukherjee S, Can a faulty injection technique lead to localized insulin allergy?IJEM 2013 17S1:S358-59. [Google Scholar]