Gallbladder disease is very common in Northern India resulting in various morphological patterns, most common of which is chronic cholecystitis. Very rarely EC can be seen which represents 0.25% to 6.4% of all cholecystitis [1]. It generally presents in the absence of gallbladder stones [2]. Eosinophilic cholecystitis is diagnosed histopathologically when more than 90% of the cellular infiltrate comprises of eosinophils present transmurally. In cases where eosinophilic infiltrate is 50-75% and other inflammatory cells are also present it is known as lympho-eosinophilic cholecystitis [1].
Although there are quite a few case reports describing eosinophilic cholecystitis in association with other conditions, the aetiopathogenesis of disease still remains obscure [3,4].
Various probable causes have been suggested which include allergies, parasites, eosinophilic enteritis, and local reaction to gall stones. However, if a postoperative histopathological diagnosis of EC is made, then the patient must be investigated thoroughly to rule out other associated disease conditions, which may have a worse prognosis than cholecystitis itself.
While reviewing the literature it was found that EC has mainly been reported as case reports and very few large series study have been done on this entity [3,4]. Keeping this in mind, this study was undertaken to determine the prevalence and clinicopathological profile of EC diagnosed over a period of five years at a tertiary care hospital of New Delhi.
Materials and Methods
This was a retrospective clinicopathological study done in the Histopathology section of Pathology department, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India. A total of 1370 cholecystectomy specimens received over a period of five years were reviewed. All the patients who underwent cholecystectomies between January 2011 and December, 2015 were included in the study. Clinical history, other relevant findings and investigations of the patients were obtained from the hospital records. Original pathology reports were retrieved for providing the histopathological data. Those patients about whom complete information was not available or the hospital records were incomplete were excluded from the study. Ethical clearance was obtained from the Institutional Ethical Committee (IEC).
All those cases in which more than 90% of the inflammatory infiltrate in the gallbladder wall comprised of eosinophils were diagnosed as eosinophilic cholecystitis while cases with 50%-75% eosinophils along with other inflammatory cells were termed lympho-eosinophilic cholecystitis.
Slides of eosinophilic cholecystitis were retrieved and various histologic features and pattern of the inflammatory infiltrate were studied, i.e., whether both muscle and mucosa showed eosinophilic infiltration or only mucosal involvement was present. Association of eosinophilic cholecystitis with other medical diseases, drugs and allergic states was also studied from the history available in the case records.
Results
EC was diagnosed histopathologically in 22 (1.6%) of the cholecystectomy specimens. A total of 43 (6.4%) specimens showed fair number of eosinophils ranging from 50%-75% but there was also presence of other types of inflammatory cells including neutrophils and lymphocytes.
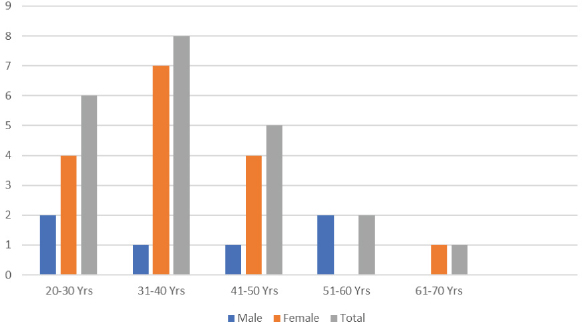
Age of the patients ranged from 25-64 years with maximum in the age range of 31-40 years.
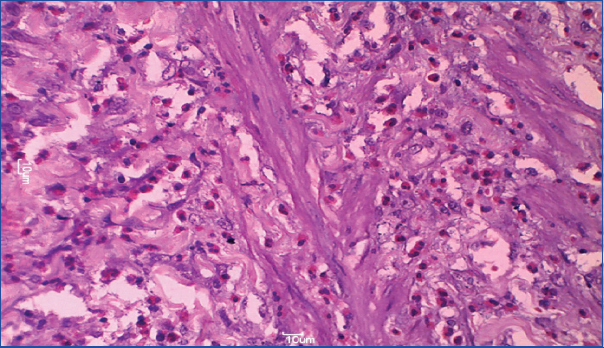
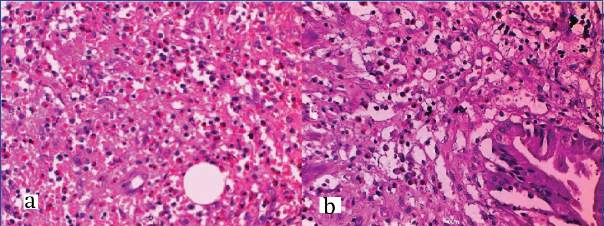
EC was more common in females i.e., 16 out of 22 cases, male to female ratio being 1:2.7 [Table/Fig-1]. Clinically, 7 of these 22 EC patients had a clinical diagnosis of acute cholecystitis while all others were diagnosed as chronic cholecystitis or cholelithiasis alone. Most common symptom reported was abdominal pain (59.1%) followed by dyspepsia (31.8%) and rarely jaundice (9.1%). All of the 22 cases except two had gallstones on imaging. Only two of the total EC cases showed peripheral eosinophilia (09%). Clinical and histological findings in gallbladder of patients with eosinophilic cholecystitis are summarized in [Table/Fig-2]. Muscle infiltrate alone was seen in 27.3% of cases [Table/Fig-3] while both mucosal and muscular eosinophilic infiltrate was seen in 72.6% cases [Table/Fig-4], EC did not show any association with drug therapy, allergies or other pre-existing medical conditions, although four patients did give history of allergy to allopathic drugs, the names of which they were not able to recall.
Distribution of cases of eosinophilic cholecystitis based on age and sex.
Clinico-pathological profile of patients with eosinophilic cholecystitis.
| S.No | Age | Sex | Clinical Diagnosis | Gallstones | Allergy | Eosinophilia | Predominant Symptom | Eosinophilic Infiltrate | Mucosal ulceration | Perimuscular fibrosis |
|---|
| Muscle and Mucosa | Muscle only |
|---|
| 1. | 42 | F | Cholelithiasis | + | - | - | Abdominal pain | + | - | + | - |
| 2 | 35 | F | Mucocele | + | - | - | Abdominal pain | + | - | + | + |
| 3 | 29 | M | Cholelithiasis | + | - | - | Dyspepsia | + | - | + | + |
| 4 | 32 | F | Acute Cholecystitis and Cholelithiasis | + | + | + | Abdominal pain | - | + | - | - |
| 5 | 39 | F | Cholelithiasis | + | - | - | Abdominal pain | + | - | + | - |
| 6 | 40 | F | Acute Cholecystitis | - | - | - | Abdominal pain | + | - | + | - |
| 7 | 24 | F | Cholelithiasis | + | - | - | Dyspepsia | - | + | + | + |
| 8 | 32 | F | Chronic Cholecystitis and Cholelithiasis | + | - | - | Abdominal pain | - | + | - | - |
| 9 | 32 | F | Acute cholecystitis | + | - | - | Jaundice | + | - | - | - |
| 10 | 30 | M | Cholelithiasis | + | - | - | Dyspepsia | + | - | - | - |
| 11 | 25 | F | Chronic Cholecystitis and Cholelithiasis | + | - | - | Abdominal pain | + | - | - | - |
| 12 | 45 | M | Cholelithiasis | + | - | - | Dyspepsia | + | | + | + |
| 13 | 46 | F | Cholelithiasis | + | - | - | Dyspepsia | - | + | + | - |
| 14 | 29 | F | Acute Cholecystitis and Cholelithiasis | + | + | + | Abdominal pain | + | - | - | - |
| 15 | 32 | M | Chronic Cholecystitis and Cholelithiasis | + | - | - | Abdominal pain | - | + | - | - |
| 16 | 51 | M | Cholelithiasis | + | - | - | Dyspepsia | - | + | + | + |
| 17 | 50 | F | Acute Cholecystitis | - | + | - | Abdominal pain | + | - | + | |
| 18 | 38 | F | Chronic Cholecystitis, Cholelithiasis | + | - | - | Abdominal pain | + | - | + | - |
| 19 | 46 | F | Acute Cholecystitis | + | - | - | Dyspepsia | + | - | | + |
| 20 | 60 | M | Empyema | + | - | - | Abdominal pain | + | - | - | - |
| 21 | 64 | F | Chronic Cholecystitis | + | - | - | Abdominal pain | + | - | + | + |
| 22 | 26 | F | Acute Cholecystitis | + | + | - | Jaundice | + | - | - | + |
Photomicrograph showing infiltration of muscle layer with eosinophils (H&E stain, 40X).
a) Photomicrograph showing intense eosinophilic infiltrate in the gallbladder wall. (H&E Stain, 40X); b) Photomicrograph showing mucosal infiltration by eosinophils. (H&E Stain, 40X).
Discussion
EC is a rare entity first described in 1949 in the French literature [5]. The prevalence of EC varies from 0.25% to 6.4% as reported in various studies across the world [1,2,4,5]. In our study it was 1.6%. EC is much more common than previously recognized and probably represents a hypersensitivity type of inflammatory response to altered bile which is seen in some patients. EC like other gall bladder lesions is more common in females. In our study, it was found in 16 females out of total of 22 cases (72.7%) which is comparable with other studies [1]. Most commonly affected age group was 30-40 years. Average age of presentation of eosinophilic cholecystitis is around 37 years [6].
Clinical presentation of EC is similar to that of typical cholecystitis. In cases where it presents as acute cholecystitis, it is very difficult to suspect the diagnosis preoperatively unless there is evidence of peripheral eosinophilia [3]. In our study, eight patients presented with cholelithiasis, seven presented with acute cholecystitis, five with chronic cholecystitis and one each with empyema and mucocele. Usually, it is an acalculous cholecystitis, but in 40% of cases, calculi are found [6,7]. Dabbs DJ et al., found that EC and LEC are more commonly associated with acalculous cholecystitis [1]. However, one interesting finding in our study was that gallstones were found in almost 90% of the EC cases. Only two cases did not show gallstones. This was contrary to other similar studies by Dabbs DJ et al., and Shakov R et al [1,3]. One of the major reasons could be that in our institute cholecystectomies are mostly done in those patients who have gallstones.
Eosinophilic cholecystitis may either be seen as a single entity or may coexist with other conditions. It may be seen in association with eosinophilic gastroenteritis, eosinophilic cholangitis, eosinophilia-myalgia syndrome, idiopathic hypereosinophilic syndrome, parasitic infestations such as clonorchis sinensis and hydatid cyst and antibiotics like erythromycin and cephalosporins [8-12]. EC association with eosinophilic cystitis has also been described [13]. None of our patients showed any association with the above mentioned conditions, although four patients did give history of allergy to allopathic drugs, the names of which they were not able to recollect. Study on EC by Dabbs DJ et al., also did not show any association with drug therapy or other pre-existing medical conditions [1].
Peripheral blood eosinophilia has been reported in association with EC; where sometimes it may present as a likely manifestation of hypereosinophilic syndrome. Kim YH et al., reported that peripheral eosinophilia occurred in four out of 15 cases [12]. In our study only two out of 22 cases showed peripheral eosinophilia. It could be attributed to seasonal variations.
Apart from EC, eosinophilic infiltration of the gastrointestinal tract may occur in hypereosinophilic syndrome, eosinophilic cholangiopathy, eosinophilic gastroenteritis, eosinophilic granulomatous hepatitis and eosinophilic ascites [14]. The symptoms depend on the location and depth of the gastrointestinal tract affected [15]. It has been suggested that symptoms such as postprandial nausea and vomiting, weight loss, iron deficiency anaemia, steatorrhea, malabsorption, and protein-losing enteropathy are seen more commonly with mucosal invasion by eosinophils while symptoms such as nausea and vomiting with abdominal distention and intermittent bowel obstruction are seen in invasion of muscularis propria. With subserosal invasion by eosinophilic infiltrate, abdominal pain, distention, pleural effusion, and ascites occur [16]. The diagnosis of EC is based on classical symptoms of cholecystitis along with the histopathological presence of >90% eosinophilic infiltrate within the gallbladder wall. Histologically, EC is distinguished from other types of cholecystitis by a dense transmural infiltration of eosinophils comprising 90% or more of the leukocytes [2]. It has been reported that in the cases where infiltrate is made up of an abundant amount of eosinophils, there are signs of inflammation, granulation tissue, and fibroblast propagation [17]. In a study by Fox H and Mainwaring AR, 16 of 625 cholecystectomies done during a two-year period showed eosinophilic infiltration out of which three cases comprised only of eosinophilic infiltrate [18]. Dabbs DJ et al., reviewed 217 gallbladders over a two-year period and 14 cases (6.5%) of EC were observed [1]. They also found that eosinophils in the inflammatory infiltrate were three times more common in patients with acalculous cholecytitis. In a recent study conducted by Kumar V et al., in 2016, a total of 867 cases were examined, out of which EC was found in 15 patients (1.73%) [19]. In our study, 22 cases out of 1370 cholecystectomies showed transmural eosinophilic infiltrate of more than 90% i.e., 1.6%. This is comparable to the recent study by Kumar V et al., [19]. However, this was higher than incidence of 0.5% given by Fox H and Mainwaring AR and much lower than 6.5% incidence given by Dabbs DJ et al., [1,18]. EC may show invasion of the mucosal surface by eosinophils. Considerable infiltration of the muscularis by eosinophils with vascular occlusion calls for surgery, whereas involvement of the mucosa or adventitia without vascular changes usually responds well to steroids [9]. In our study six cases showed only muscular involvement, while 16 cases showed both mucosal and muscular involvement.
As there is no specific clinical presentation of eosinophilic cholecystitis, histopathological evaluation is the main modality for diagnosing this condition. The treatment of choice remains cholecystectomy. However, in case of association with eosinophilic gastroenteritis or cholangitis steroids may be used as an adjuvant therapy [9].
Limitation
The major limitation of the study was that since it was a retrospective study we had included only those cases which were reported as cholecystitis, and it is quite possible that other reporting histopathologists might not have been stringent enough to label EC in all those cases where eosinophilic infiltrate was more than 90%. Thus, few cases might have been missed out.
Conclusion
To conclude, EC is a well known entity of which gastroenterologists, pathologists and surgeons need to be aware. It does not have a specific clinical presentation. However, once the diagnosis of Eosinophilic cholecystitis is made histopathologically, it is very important to identify the underlying etiology and to exclude other organ involvement. In case it is found treatment more than a cholecystectomy maybe warranted.