CAG in pterygium surgery can be attached by sutures or fibrin glue or autologous in situ blood coagulum. Attaching CAG with autologous in situ blood coagulum is a new technique that is in practice for the past few years. The advantages of autologous in situ blood coagulum are ready availability of patient’s own blood, no additional cost, no risk of transmission of blood related diseases and no suture related complications. Some studies have shown good results with the new technique [1-9].
Comparison of one technique over the other in terms of recurrence has been carried out by some authors [3-9]. Singh PK et al., found no difference in the recurrence rate between fibrin glue and suture groups; similarly, Choudhary S et al., found no difference between conjunctival fixation with sutures and autologous in situ blood coagulum, and Sati A et al., found equal recurrence in all these three techniques [3-5]. However, these studies included all grades of pterygia and the comparison was not uniform in a single grade of pterygium. Doing the comparison in a single grade would enable us to see the effects of such procedures in a more uniform way.
To the best of our knowledge, uniformly in advanced pterygia alone, no study has compared the recurrence rate and other parameters between CAG with sutures and autologous in situ blood coagulum. Therefore, our aim was to compare and evaluate the outcome of sutureless, glue-less CAG with autologous in situ blood coagulum versus CAG with sutures in advanced, Grade 3 pterygia as per Tan et al’s., classification [10].
Materials and Methods
This was a prospective, interventional pilot study conducted at the Department of Ophthalmology of North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, India from April 2014 to May 2015. Institute Ethical Clearance was taken and the study adhered to the tenets of the Declaration of Helsinki. Written informed consent was taken from every patient.
Thirty eyes of 30 patients with primary, nasal, advanced, grade 3 pterygia were randomized into two groups by computer generated random numbers, as a pilot study for only the higher grade pterygia. In Group 1, 15 cases underwent sutureless, glue-less CAG with autologous in situ blood coagulum and in group 2, 15 cases underwent CAG with 8-0 vicryl sutures. Inclusion criteria were primary, nasal, grade 3 pterygia as per the Tan et al., classification {Grade T3 (fleshy) denoted a thick pterygium in which episcleral vessels underlying the body of the pterygium were totally obscured} [10].
Exclusion criteria were recurrent pterygium, temporal pterygium, pseudo-pterygium, ocular surface disorders, and cases with positive serology for HIV and Hepatitis B.
Under topical anaesthesia with proparacaine 0.5% HCL ophthalmic solution (Paracain, Sunways Pvt. Ltd., Mumbai), the affected eye was cleaned and draped. Speculum was inserted. Betadine was instilled in the conjunctival sac and washed. Lignocaine 2% (Lox 2%, Neon Lab. Ltd., Mumbai) was injected into the body of the pterygium and allowed to spread to other areas of the pterygium. The pterygium was dissected from the apex with a took’s knife. It was then removed in toto. The corneal surface was smoothened with the edge of a crescent knife. The desired rectangular area of the bare scleral bed needed to be covered with CAG was measured with the help of a calliper. Lignocaine 2% was injected into the inferior subconjunctival space and the conjunctiva was ballooned out. A thin conjunctiva devoid of tenon’s tissue and equal to the size of bare sclera already measured with caliper was resected.
In Group 1, bleeding was encouraged from the episcleral vessels to form a coagulum. If there was excessive bleed, it was removed to adequate amount to form a coagulum. The resected donor conjunctiva was immediately placed on the recipient area taking care of proper orientation. Uniform pressure was applied on this graft with the help of McPherson forceps for 10 minutes so that the graft gets adhered to the underlying sclera with the help of the blood coagulum. The patient was asked to adduct or abduct his/her eye to see whether the graft remained in place on ocular movements. If the adherence was satisfactory, the speculum was removed and the graft stability was rechecked with eye blinking. If the graft was found to be stable, one drop of preservative free moxifloxacin 0.5% ophthalmic solution (Vigamox@, Alcon Laboratories Inc., Texas) was instilled and the eye was patched. If the graft stability was not satisfactory the above procedure for graft adherence was repeated. The eye was patched for 24 hours.
In Group 2, the graft was immediately placed on the recipient area and sutured with 8-0 vicryl in its four corners. If the graft was long, 1-2 more sutures were applied. Mitomycin C (MMC) was not applied in either of the groups. Postoperatively, patients were given antibiotic steroid combination (Apdrop-DM, Ajanta Pharma Ltd., Mumbai) in tapering doses over one month and lubricating eye drops (Tears Naturale Forte, Alcon Laboratories Inc., Texas).
Outcome parameters evaluated were graft stability and symptoms of pain, foreign body sensation and watering (epiphora) at day 1, day 7, day 14, one month, three months and six months using the 5 point scale adapted from Lim-Bon-Soong R et al., and recurrence at six months [11]. A 5-point pain scale was used to measure the amount of pain. The following descriptions were used: none = no pain at all; very mild = presence of pain but easily tolerated; mild = presence of pain causing some discomfort; moderate = presence of pain causing discomfort that interferes with usual activity or sleep; and severe = presence of pain that completely interferes with usual activity or sleep [11]. Similarly, we adopted 5 point abnormal sensations scale (0 = none, 1 = somewhat bothersome but easily tolerated, 2 = bothersome causing some discomfort, 3 = very bothersome interfering with activities partially, 4= extremely bothersome, interfering completely with normal activities and sleep) to determine the amount of foreign body sensation and watering (epiphora). Similarly, the graft stability was graded as Grade 0 = all four sides of graft are well attached to the sclera, Grade 1 = displacement of one side of the graft from the scleral bed, 2= displacement of two sides of the graft, 3 = displacement of three sides of the graft and 4 = complete displacement of the graft from the scleral bed. Here, lower the grade, more the graft stability and higher the score, lesser the stability of the graft. Recurrence was defined as any conjunctival re-growth onto the cornea from the same area of pterygium excision.
Statistical Analysis
Clinical characteristics were found by descriptive statistics. Comparison of outcome variables between two groups was done using non-parametric Mann-Whitney U test. Graphs were plotted using Multiple line charts. A 5% level of significance was adopted. Therefore, a p-value of <0.05 was considered statistically significant. Statistical analysis was performed using the SPSS software package (SPSS for Windows, version 22.0; SPSS, Inc., Chicago, IL).
Results
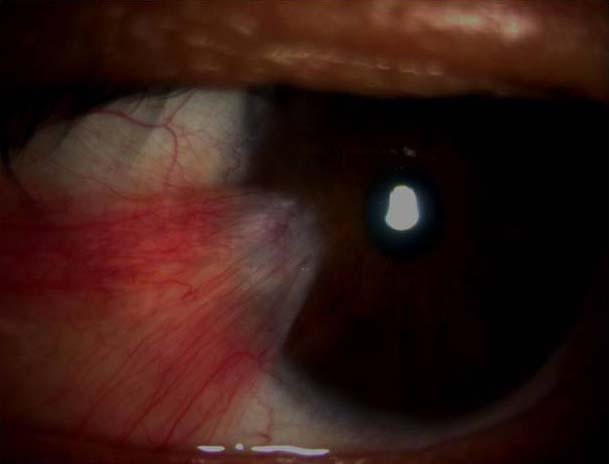
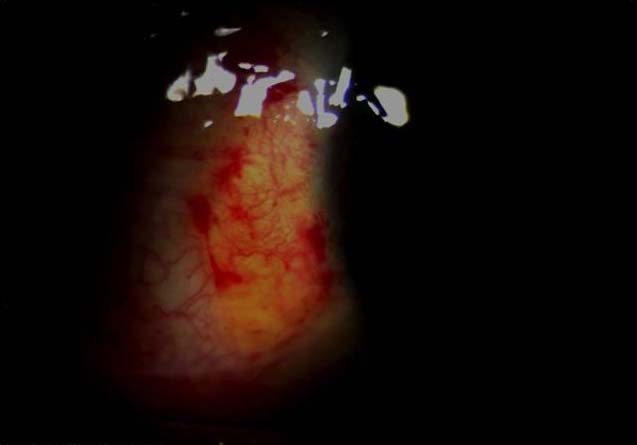
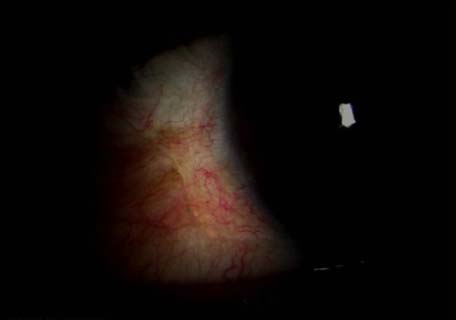
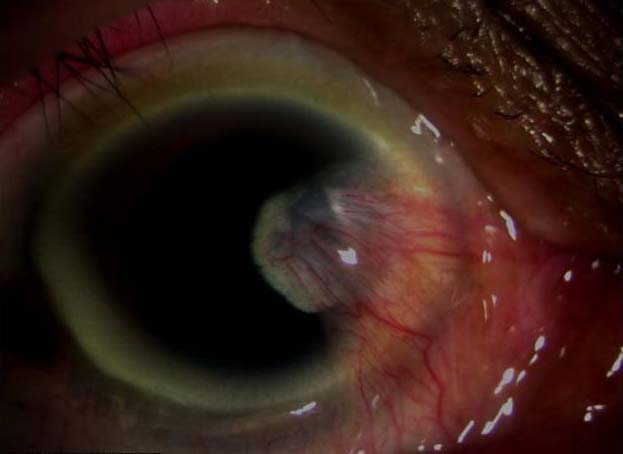
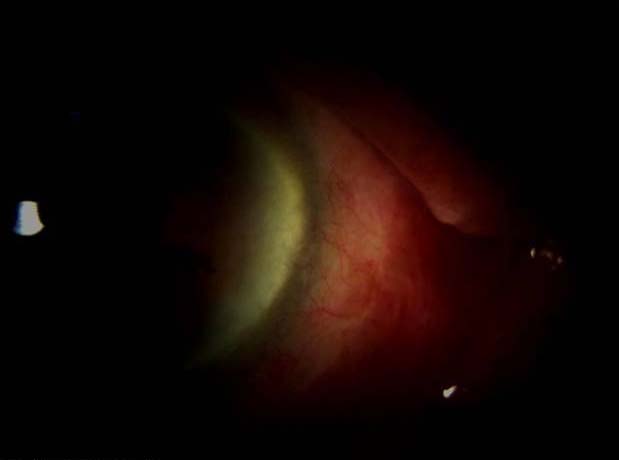
The mean age in the study was 44.77±13.74 years. Images of a case in Group 1 and 2 in the preoperative period and day 14 and day 30 postoperative periods are shown in [Table/Fig-1,2 and 3] and [Table/Fig-4,5 and 6] respectively.
Preoperative photograph of a case of primary, grade 3, nasal pterygium in the left eye of Group 1.
Postoperative appearance following pterygium surgery using CAG with autologous in situ blood coagulum in the same patient on day 14.
Postoperative appearance following pterygium surgery using CAG with autologous in situ blood coagulum in the same patient on day 30.
Preoperative photograph of a case of primary, grade 3, nasal pterygium in the right eye of Group 2.
Postoperative appearance following pterygium surgery using CAG with sutures in the same patient on day 14.

Postoperative appearance following pterygium surgery using CAG with sutures in the same patient on day 30.
There was statistically significant difference in the two groups in the scores of the postoperative foreign body sensation, pain, epiphora and graft stability (p<0.05).
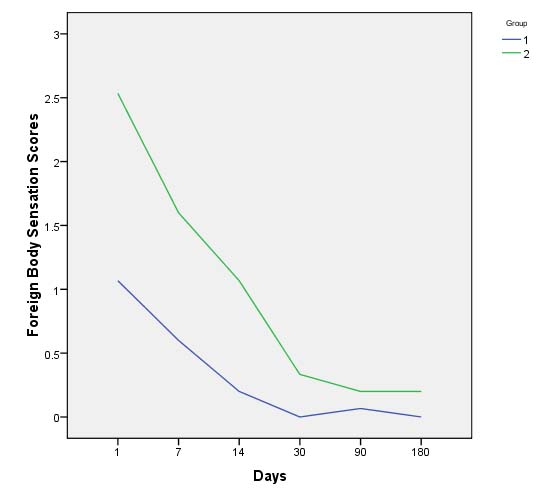
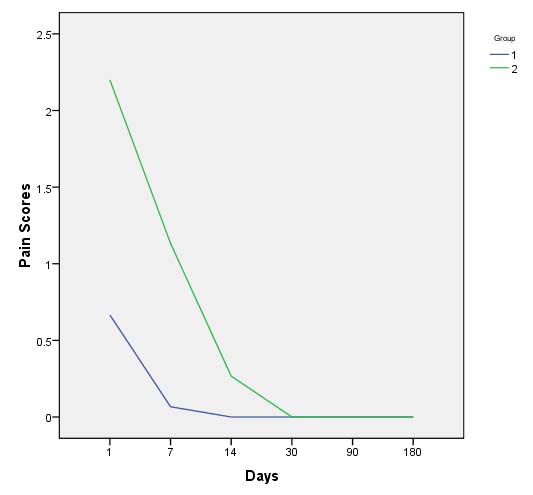
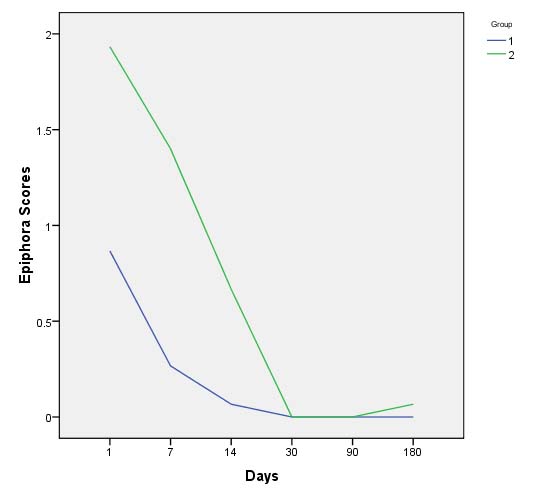
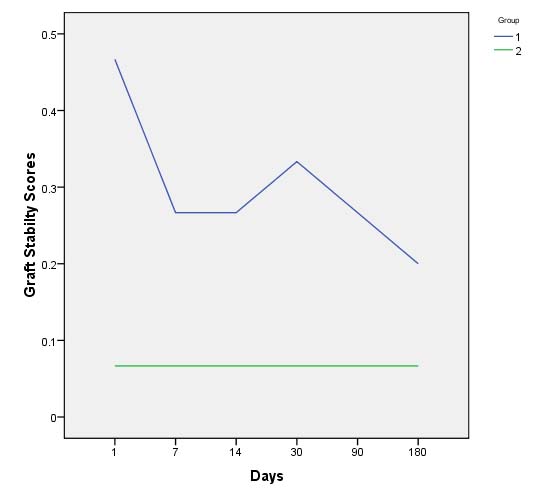
The line graphs showing the scores of the foreign body sensation, pain, epiphora, and graft stability over six months duration in the two groups are shown in [Table/Fig-7,8,9 and 10] respectively. [Table/Fig-7,8 and 9] show that the foreign body sensation, pain and epiphora scores are more in Group 2 as compared to Group 1. [Table/Fig-10] shows that graft stability is more in Group 2, since lesser score means more stability as per the grading. All the patients completed the follow up period.
Line graphs showing comparison of foreign body sensation scores on a five-point scale in the two groups, wherein Group 2 has higher foreign body sensation scores as compared to Group 1 throughout the study period, meaning Group 2 has more foreign body sensations.
Line graphs showing comparison of pain scores on a five-point scale in the two groups. From day 1 till day 30, Group 2 has higher pain scores than Group 1. Subsequently, both the groups have equal pain scores.
Line graphs showing comparison of epiphora scores on a five-point scale in the two groups., From day 1 till day 30, Group 2 has higher epiphora scores than Group 2. Subsequently, both the groups have almost equal scores.
Line graphs showing comparison of graft stability scores on a five-point scale in the two groups. Group 2 has lower scores than Group 1 throughout the study period, meaning Group 2 has more graft stability, since lower score means more stability as per the grading system.
Group 1 had better scores in symptom parameters than Group 2 (p<0.05). Graft stability was better in Group 2 (p<0.05). In Group 1, 3 (20%) patients had one side displacement and 3 (20%) patients had full displacement/loss of graft [Table/Fig-11]. The grafts with one side displacements were reposited to its proper position with McPherson forceps under the slit lamp on day 1 under topical anaesthesia. In patients with full displacements/loss of graft, the surgical procedure was repeated by taking a new graft from the upper conjunctiva. The grafts remained in place after the repeat surgeries. At 6 months, 4 (26.6%) patients in Group 1 had recurrence whereas in Group 2, 5 patients (33.3%) had recurrence, the difference of which was not statistically significant (p=0.446). These patients were re-operated with CAG and MMC, the follow up details of which are beyond the scope of this study.
Summary of difference in symptom parameters and graft stability seen in the two groups.
| Symptom Parameters | Graft stability |
|---|
| Scores | Group 1 scored better than Group 2. | Group 2 scored better than Group 1. |
| p-value of difference in groups (by Mann-Whitney test) and percentage of graft displacement. | p<0.05 | p<0.05; 20% - one sided displacement and 20% full displacement/loss of graft seen in Group1. |
N.B.: Symptom parameters were based on foreign body sensation, Pain and Epiphora.
Discussion
Recurrence following pterygium surgery is a cause of concern for both the patient and the treating surgeon. Pterygium surgery using CAG with in situ blood coagulum has been carried out by some authors in all grades of pterygia [1-9]. However, no study has been done to see its effect uniformly in advanced Grade 3 pterygia.
In pterygium surgeries, CAG can be fixed to the sclera by sutures, fibrin glue or in situ blood coagulum. It has not been proven in which of these techniques the recurrence is the least. Classically, CAG is attached to the sclera with the help of sutures. Fibrin glue has also been found to be effective in attaching the CAG in pterygium surgeries [12-16]. However, there are certain concerns with the commercially available fibrin glue. There is risk of transmission of human infection of parvovirus B19 and prions [17,18]. Also, fibrin glue is costly and cannot be afforded by patients from poor socio-economic status, who are more susceptible to formation of pterygium. Therefore, we have tried to compare the surgical outcome in advanced cases of pterygia between the suture group and in situ blood coagulum group. Sutures are easily available and are cheap and in situ blood coagulum is readily available from the patient’s own blood. As per Sati A et al., sutures do not incite more inflammation than the non-suture group since postoperative steroids take care of the postoperative inflammation [5]. According to them it is the barrier effect of CAG that plays an important role in preventing recurrences. Therefore, comparing a suture group with in situ blood coagulum group is justified.
In the present study, high rate of recurrence is noted in our cases of both the groups. This could probably be because of the higher grade of pterygia since advanced cases are more fleshy and progressive in nature. However, the recurrence rates we got (26.6-33.3%) are well within the recurrence rates that were found in some prospective, randomised trials of CAG in high risk population (16-39%) [19,20]. Other authors got lesser recurrence (2.5-10%) as compared to us since they included all grades of pterygia [1-9]. Some of them have tried comparing one technique over the other in terms of recurrence [3-9]. Singh PK et al., found no difference in the recurrence rate between fibrin glue and suture groups [3]. Similarly, Choudhary S et al., found no significant difference in the recurrence rate between conjunctival fixation with sutures and autologous in situ blood coagulum [4]. Sati A et al., also found equal recurrence rate in all the three techniques [5]. However, these studies included all grades of pterygia. In terms of recurrence, we did not get any statistically significant difference between the two groups. This is in agreement with the previously mentioned studies [3-9]. However, Boucher S et al., found more recurrence in the autologous in situ blood group in comparison to the fibrin glue group [9]. Recurrence has been found to be a common problem following pterygium surgery [21-24].
Overall, Group 1 had better scores in symptom parameters than Group 2 (p<0.05) whereas graft stability was better in Group 2 (p<0.05). Better symptom parameter scores in CAG with in situ blood coagulum group as compared to suture group has been established in previous studies too [4-6,8]. The technique of attaching CAG with in situ blood coagulum appeared to be unpredictable in our experience. In Group 1, three patients (20%) had one side displacement and three patients (20%) had full displacement/loss of graft. Boucher S et al., also found that CAG with autologous in situ blood coagulum resulted in less stable conjunctival autografts [9]. They had six numbers of total graft loss out of 40 patients (15%), in the autologous in situ blood group. Choudhury S et al., also had one case of total graft dehiscence in the autologous in situ blood group [4]. Therefore, it may be inferred that CAG with in situ blood coagulum may be unpredictable in nature for attaching CAG to the sclera. Graft retraction and partial displacement have been common complications of CAG reported in similar studies [4-6,9].
There are obvious advantages using autologous in situ blood coagulum for CAG in pterygium surgeries. It has less postoperative discomforts, no extra cost involved, easy to use and shorter operating time. However, according to our findings, it has the disadvantage of unpredictability in attaching the CAG. A surgeon can never be very sure if the CAG will be uniformly attached to the scleral bed and have no graft loss, when the eye pads are removed. This is not the case with sutures or fibrin, where it is unlikely to have full graft displacement or loss unless there is vigorous rubbing of the operated eye or trauma.
Limitation
There are certain limitations in our study. Firstly, the duration of follow up was only six months. It would have been better if it was for one year or more. We could not do so because many patients were from other states and they were unwilling for longer follow up. Secondly, although it was a pilot study on advanced pterygium with a limited number of subjects, it would have been better if the sample size was larger. Thirdly, mitomycin C was not used concurrently with CAG. Its use could have reduced the recurrence rate, although it has its own risks.
Conclusion
In this pilot study with advanced pterygia, although sutureless, glue-less pterygium surgery with autologous in situ blood coagulum was better in symptom scores and worse in graft stability than the suture group, no statistically significant difference was found in the recurrence rates between the two groups. Although there is no doubt that CAG with in situ blood coagulum has a definite role in pterygium surgery, CAG with sutures may remain a gold standard for pterygium surgery.
Declaration
This paper was presented as an original article at the 74th All India Ophthalmological Conference held at the Science City-Milan Mela Complex, Kolkata from 25th-28th Feb 2016.
N.B.: Symptom parameters were based on foreign body sensation, Pain and Epiphora.