Patterns of Thyroid Cancers in Southeastern Nigeria: A 15 Year Histopathologic Review (2000-2014)
Francis Ikechukwu Ukekwe1, Daniel Bankole Olusina2, Philip C.N. Okere3
1 Lecturer/Consultant, Department of Morbid Anatomy, University of Nigeria, Enugu Campus, Enugu, Nigeria.
2 Senior Lecturer/Consultant, Department of Morbid Anatomy, University of Nigeria, Enugu Campus, Enugu, Nigeria.
3 Senior Lecturer/Consultant, Department of Radiation Medicine, University of Nigeria, Enugu Campus, Enugu, Nigeria.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Francis Ikechukwu Ukekwe, Lecturer/Consultant, Department of Morbid Anatomy, University of Nigeria, Enugu Campus-400241, Enugu, Nigeria.
E-mail: drikukekwe@hotmail.com
Introduction
Thyroid Cancer (TC) continues to be the most common endocrine cancer with a worldwide increase in incidence over the last three decades. This trend has been reported in all continents except Africa, where detection is adjudged to be insufficient, making it imperative for us to re-evaluate the patterns in our environment.
Aim
To determine the patterns of TCs in Southeastern Nigeria.
Materials and Methods
This was a 15-year retrospective review of all thyroidectomy specimens received at the Department of Morbid Anatomy, University of Nigeria, Enugu Campus, Enugu, Nigeria. The age, sex and histologic subtypes of diagnosed TCs were analysed using Predictive Analytics Software (PASW) Statistics for Windows, Version 18 (Chicago: SPSS Inc.) and the results were expressed in descriptive statistics.
Results
Sixty one cases of TCs were identified in this study constituting 10.8% of thyroid biopsies received at our centre during the period under review. There were 51 (83.6%) females and 10 (16.4%) males giving a ratio of 5.1:1, and a mean age of 45.9 years. The commonest histologic type was Papillary Thyroid Carcinoma (PTC) (42.6%), followed by; follicular thyroid carcinoma (37.7%), medullary thyroid carcinoma (4.9%), anaplastic carcinomas (3.3%), Non-Hodgkin lymphoma (1.6%) and metastatic squamous cell carcinoma (3.3%). Mixed papillary/ follicular carcinoma (4.9%) and mixed papillary/ anaplastic carcinoma (1.6%) were also identified.
Conclusion
TC continues to predominate amongst females, occurring mainly in early middle age group in Southeastern Nigeria. PTC is now the commonest histologic type.
Carcinoma, Histology, Pathology, Thyroidectomy
Introduction
Thyroid Cancer continues to be the most common endocrine cancer with a worldwide increase in incidence over the last three decades [1-3] and a preponderance of its papillary subtype [2]. Though a relatively rare neoplasm worldwide, it collectively constitutes approximately 1–1.5% of all cancers in females and < 2% in males with a fairly consistent female to male ratio of 3:1 in almost all geographic areas and ethnic groups [1]. Its incidence has grown globally to become the fifth most common cancer in women [4], and the second most frequent cancer in women below 45 years of age in countries like Italy [5] but has however decreased in a few others like Norway and Sweden [3]. This trend of increasing TC incidence has been reported in all continents but Africa [3], where the detection is adjudged to be insufficient [6].
Differentiated Thyroid Cancers (DTCs) are the commonest TCs (90%) occurring worldwide and consisting mainly of papillary and follicular cancers [7]. These cancers arise from the follicular cells of the thyroid gland and include follicular cancers which have been reported to predominate in regions where dietary intake of iodine is low [8]. Earlier review of trends of DTC from some West African Tertiary Centres in the 1980s showed a predominance of follicular over papillary cancer (35.8% vs 27.3%), but a further review from 1990 to 2004, showed a reversed predominance of papillary over the follicular cancer (35.7% vs 24.8%) [9].
With previous study of TCs in Southeastern Nigeria, done about three decades ago, it is imperative therefore for us to re-evaluate the patterns of TCs in our environment to be better prepared to manage our own share of TCs.
Materials and Methods
This was a 15 years retrospective study of 564 thyroidectomy biopsy specimens received at the Department of Morbid Anatomy, University of Nigeria Teaching Hospital, Ituku-Ozalla Enugu, Nigeria from the year 2000 to 2014. The study started in September, 2015 and ended in March 2016. This is the core referral centre, offering histopathology services to all the five states of the southeast region of Nigeria as well as the adjoining states in the north central and south-south geopolitical regions of Nigeria. The ethical clearance for this study was obtained from the Health Research Ethical Committee of University of Nigeria Teaching Hospital. Relevant clinical data of the patients such as; histology number, age, sex and other relevant clinical information of the patients were obtained from the duplicate copies of the request forms and case notes in the Department of Morbid Anatomy as well as the hospital medical record archive. All thyroid biopsies that were poorly fixed and processed were excluded from this study. In addition, cases with missing information on age and sex were also excluded from this study.
The tissue blocks of all the 564 thyroidectomy specimens were retrieved from the departmental archives and the sections made from them were stained with routine Haematoxylin and Eosin (H&E) stains. TCs were classified into; papillary, follicular, medullary, anaplastic (undifferentiated), and metastatic carcinomas as well as non-Hodgkin lymphoma, mixed follicular/ papillary and mixed papillary/anaplastic carcinomas. The slides were examined using binocular light microscope (Leica Microsystems-Wetzlar, Germany) and diagnosis of TC was made based on histopathology.
Statistical Analysis
The results obtained were analysed using Predictive Analytics Software (PASW) Statistics for Windows, Version 18 (Chicago: SPSS Inc.).
Results
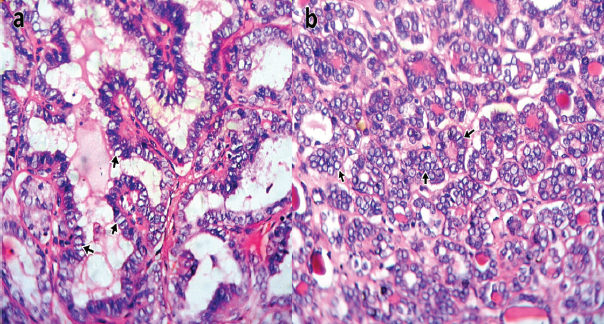
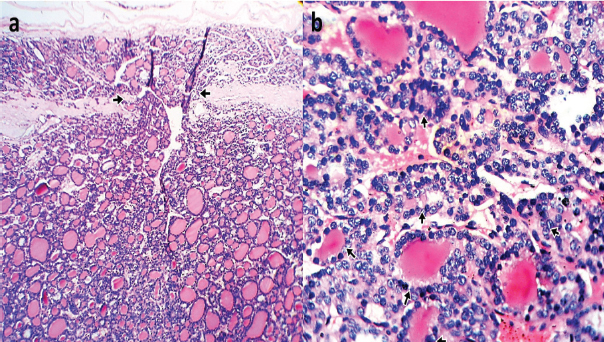
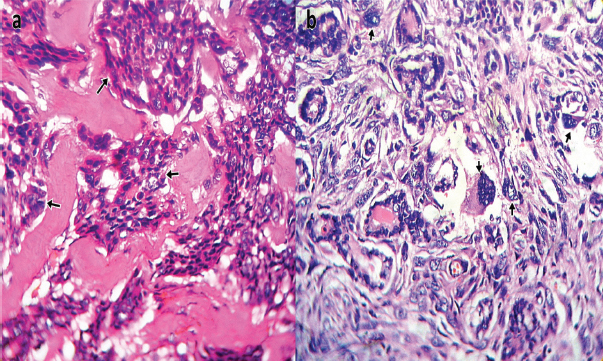
Sixty-one (61) cases of TCs were identified in this study constituting 10.8% (61/564) of thyroidectomy specimens received at our hospital’s Morbid Anatomy Department during the 15 year period under review. There were 51 (83.6%) females and 10 (16.4%) males giving a ratio of 5.1:1, and a mean age of 45.9 years [Table/Fig-1]. The most common histologic type was papillary thyroid carcinoma 26 (42.6%) cases [Table/Fig-2], followed by follicular carcinoma 23 (37.7%) cases [Table/Fig-3], medullary thyroid carcinoma 3 (4.9%) cases [Table/Fig-4a], anaplastic carcinomas 2 (3.3%) cases [Table/Fig-4b], Non-Hodgkin lymphoma 1 (1.6%) case and metastatic squamous cell carcinoma 2 (3.3%) cases. Three (4.9%) cases of mixed follicular/papillary carcinoma and one (1.6%) case of mixed papillary/anaplastic carcinoma were also identified in this study.
Age and sex distribution of thyroid cancers.
| Patient age | Sex | Total |
|---|
| Female | Male |
|---|
| 0-9 yrs | 0 | 0 | 0 |
| 10-19 yrs | 1 | 0 | 1 |
| 20-29 yrs | 7 | 0 | 7 |
| 30-39 yrs | 9 | 1 | 10 |
| 40-49 yrs | 14 | 4 | 18 |
| 50-59 yrs | 10 | 4 | 14 |
| 60-69 yrs | 5 | 1 | 6 |
| 70-79 yrs | 5 | 0 | 5 |
| Total | 51 | 10 | 61 |
| Ratio | 5.1 | 1 | |
Photomicrograph of Papillary carcinoma showing: (a) Conventional type with complex branching and randomly oriented malignant papillary structures lined by optically clear [Orphan Annie] nuclei [short arrows] (H & E Stain X400); (b) Follicular type with proliferating atypical follicles lined by optically clear [Orphan Annie] nuclei, [short arrows] (H & E Stain X400).
Photomicrograph of Follicular carcinoma of thyroid showing: (a) Capsular transgression [short arrows] by the malignant follicular proliferation (H & E Stain X100); (b) Proliferation of atypical follicles lined by hyperchromatic cells [short arrows] (H & E Stain X400).
Photomicrograph of: (a) Medullary carcinoma of the thyroid showing paragangliomatous and pseudopapillary growth patterns [short arrows] (H & E Stain X400); (b) Anaplastic carcinoma of thyroid, giant cell type showing tumor giant cells with bizarre hyperchromatic nuclei [short arrows] (H & E Stain X400).
Most 12 (19.7%) cases of TCs were received in 2013, followed by 10 (16.4%) cases in 2002 and the least 1 (1.6%) case in 2007. Most TCs also occurred in the 40-49 years age group with total of 18 (29%) cases and a male to female ratio of 1:3.5. While most papillary carcinomas 7 (26.9%) cases occurred in the 20-29 years age group, most follicular carcinomas 12 (52.2%) cases occur in the 40-49 years age group [Table/Fig-5]. The youngest patient with carcinoma was 15 years with papillary carcinoma while the oldest was 71 years with follicular carcinoma.
Histological type and age distribution of thyroid cancers.
| Histological type | Patient age | Total |
|---|
| 10-19 yrs | 20-29 yrs | 30-39 yrs | 40-49 yrs | 50-59 yrs | 60-69 yrs | 70-79 yrs |
|---|
| Follicular carcinoma | 0 | 0 | 1 | 12 | 5 | 3 | 2 | 23 |
| Metastatic neoplasms | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| Papillary carcinoma | 1 | 7 | 6 | 5 | 4 | 1 | 2 | 26 |
| Medullary carcinoma | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 3 |
| Undifferentiated /Anaplastic carcinoma | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| Non-Hodgkin lymphoma | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Mixed Follicular and Papillary carcinoma | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 3 |
| Mixed Papillary and Anaplastic carcinoma | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Total | 1 | 7 | 10 | 18 | 14 | 6 | 5 | 61 |
Discussion
TC remains an important form of patient presentation at our hospital, constituting a total of 61 cases and 10.8% of 564 thyroidectomy specimens received at our hospital’s Morbid Anatomy Department during the 15 years period under review. This indicates a 2.5% increase in TC incidence compared to a report of 8.3% from a previous study done in Enugu three decades ago [10]. It is however similar to the 10.9-15.1% reported in some Nigerian cities [11-14] but higher than the 8.1% and 7% reported by Adeniji KA et al., and Abdulkareem FB et al., from other Nigerian cities of Ilorin and Lagos respectively [15,16]. Thus, there is a rise in TC incidence in Nigerian cities over the last three decades [10-16]. There were 51 (83.6%) females and 10 (16.4%) males with TC, giving a ratio of 5.1:1 and a mean age of 45.9 years. Compared to 87.1% females and 12.9% males (6.8:1) from the previous study by Anidi AI et al., lesser females and more males now have TC in South eastern Nigeria [10]. However, when compared to the global ratio of 3:1, more females and fewer males have TCs in South Eastern Nigeria compared to the global trends [1].
Papillary carcinoma represented 4.6% of all the thyroid biopsies and 42.6% of TCs in our study, making it the predominant histological type of thyroid carcinoma in our study, followed by follicular carcinoma (37.7%). This is at variance with that of previous study in our environment [10], which reported an almost equal incidence between papillary and follicular carcinomas and those of other Nigerian [12,13,15-17] and foreign [18,19] studies which found follicular carcinoma to be the most common TC. Our finding of emerging papillary carcinoma predominance is however in tandem with to those of some Nigerian [11,14,20,21] and foreign studies [22-26]. Though, papillary carcinoma of the thyroid is the most common histologic type globally and in iodine sufficient areas, follicular carcinoma has higher frequency in iodine deficient areas [7,27]. South-eastern Nigeria and its adjoining communities are in the iodine deficient zones of Nigeria [28], with most TCs (29.5%) and PTCs (26.9%) occurring in the 40-49 years and 20-29 years age groups respectively. The emergence of PTC with a mean age of 39.0 years as the predominant pattern in our environment similar to those in developed countries could be attributable to previous widespread universal salt iodization programs as well as increased efforts at regulation of consumption of iodized salt and other food products in Nigeria [12,29,30] as well as a rise in socioeconomic status [20]. These efforts at decreasing iodine deficiency have also been reported to improve TC outcomes by changing TCs to less aggressive subtypes [9].
Follicular carcinoma is the second most common TC (37.7%) occurring mostly in the 40-49 years age group and with a mean age of 50.4 years. This is also in tandem with trends in developed countries with iodine sufficiency [7,27].
Medullary carcinoma is still relatively uncommon with only 3 (4.9%) cases identified in our study which is in agreement with findings from Port-Harcourt (one case), Ile-Ife (one case), Zaria (three cases) and Lagos (four cases) in Nigeria [11,13,16,21] as well as reports from Ethiopia (one case) [22] and Pakistan (four cases) [25].
Our study also recorded only 2 (3.3%) cases of anaplastic carcinoma. This is similar to those of studies in Port-Harcourt, Kano, Ile-Ife and Lagos that also reported 1-2% cases [11-13,16]. This rare type of TC often presents with a fatal disease course despite aggressive treatment modalities of surgery, chemotherapy, and radiotherapy, in contrast to the excellent prognosis of individuals diagnosed with DTC [31]. Two (3.3%) cases of metastatic squamous cell carcinoma were also noted in our study which is consistent with the finding of one case in a recent study in Kano [32]. Similarly, only 1 (1.6%) case of Non-Hodgkin lymphoma was discovered in our study.
The occurrence of mixed carcinomas which is the coexistence of two cancers in a patient was observed in four cases with three (4.9%) cases of mixed follicular and papillary carcinomas and one (1.6%) case of mixed papillary and anaplastic carcinoma identified in our study. Anaplastic thyroid carcinoma could occur de novo or by anaplastic transformation by dedifferentiation of pre-existing well-differentiated thyroid carcinomas such as papillary or follicular thyroid carcinomas [33-34]. In our study was a case of malignant transformation of the normally docile papillary tumour into a more rapidly invasive anaplastic form with increased metastatic potential. The finding of the youngest TC patient aged 15 years old with papillary thyroid carcinoma and the oldest aged 71-year-old with follicular thyroid carcinoma is agreement with reports from a similar study in Kano [32].
The mixed carcinomas could also represent foci of Second Primary Cancers (SPC) or Secondary Cancers With Transformation (SCT) [35]. Most SPC have very short detection intervals (including synchronous occurrences), suggesting that therapy with internal radiation was not contributory to the tumour development. When TCs occur as the second primary cancers, they usually follow radiotherapy to the head and neck region for treatment of the first primary tumour and tend to be of aggressive histologic types than the common well differentiated thyroid carcinomas [35].
Research using immunogenetic and immunohistochemical techniques would be of great essence in elucidating the biology of these tumours. The absence of these essential facilities in the laboratories of most developing countries such as ours [36], highlights the need to better equip our laboratories.
Limitation
The authors hereby acknowledge that this study may not be fully representative of the general population because the study was based on cases on which thyroid biopsy and histology were done with the exclusion of those for which biopsy and histology were not done.
Conclusion
TC continues to present with a high female predominance, occurring mainly in early middle age group in Southeastern Nigeria. The emergence of PTC as the commonest histologic type could be due to increased efforts at decreasing iodine deficiency by promotion and regulation of consumption of iodized salt and food products. The role of mixed TCs needs further evaluation.
[1]. Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, Cancer incidence in five continents 2007 IXLyon, IARCIARC Scientific Publications:160 [Google Scholar]
[2]. Aschebrook-Kilfoy B, Grogan RH, Ward MH, Kaplan E, Devesa SS, Follicular thyroid cancer incidence patterns in the United States 1980–2009Thyroid 2013 23(8):1015-21. [Google Scholar]
[3]. Kilfoy BA, Zheng T, Holford TR, Han X, Ward MH, Sjodin A, International patterns and trends in thyroid cancer incidence 1973–2002Cancer Causes and Control 2009 20:525-31. [Google Scholar]
[4]. Jemal A, Siegel R, Xu J, Ward E, Cancer statistics 2010CA Cancer J Clin 2010 60(5):277-300. [Google Scholar]
[5]. Dal Maso L, Lise M, Zambon P, Falcini F, Crocetti E, Serraino D, Incidence of thyroid cancer in Italy 1991–2005:time trends and age-period-cohort effectsAnn Oncol 2011 22:957-63. [Google Scholar]
[6]. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R, Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factorsJournal of Cancer Epidemiology 2013 2013:965212 [Google Scholar]
[7]. Mazzaferri EL, An overview of the management of papillary and follicular thyroid carcinomaThyroid 1999 9:421-27. [Google Scholar]
[8]. Kalk WJ, Sitas F, Patterson AC, Thyroid cancer in South Africa-an indicator of regional iodine deficiencyS Afr Med J 1997 87:735-38. [Google Scholar]
[9]. Woodruff SL, Arowolo OA, Akute OO, Afolabi AO, Nwariaku F, Global variation in the pattern of differentiated thyroid cancerAm J Surg 2010 200(4):462-66. [Google Scholar]
[10]. Anidi AI, Ejeckam AC, Ojukwu JO, Thyroid carcinoma in Enugu--Eastern NigeriaEast Afr Med J 1985 62(3):206-12. [Google Scholar]
[11]. Seleye-Fubara D, Numbere N, Etebu EN, Pathology of common diseases of the thyroid gland in Port HarcourtPort Hart Med J 2009 3:312-17. [Google Scholar]
[12]. Edino ST, Mohammed AZ, Ochicha O, Thyroid diseases in KanoNiger Postgrad Med J 2004 11:103-06. [Google Scholar]
[13]. Nggada HA, Ojo OS, Adelusola KA, A histopathological analysis of thyroid diseases in Ile-Ife, Nigeria: A review of 274 casesNiger Postgrad Med J 2008 15:47-51. [Google Scholar]
[14]. Ijomone EA, Duduyemi BM, Udoye E, Nwosu SO, Histopathological review of thyroid diseases in southern Nigeria-a ten year retrospective studyJournal of Medicine and Medical Sciences 2014 5(6):127-32. [Google Scholar]
[15]. Adeniji KA, Anjorin AS, Ogunsulire A, Histological pattern of thyroid diseases in a Nigerian populationNiger Q J Hosp Med 1998 8:241-44. [Google Scholar]
[16]. Abdulkareem FB, Banjo AA, Elesha SO, Histological review of thyroid lesions: A 13-year retrospective study (1989-2001)Niger Postgrad Med J 2005 12:210-14. [Google Scholar]
[17]. Nggada HA, Gali BM, Khalil MIA, Thyroid carcinoma in North Eastern Nigeria: A review of 26 casesHighland Medical Research Journal 2006 4(1):46-52. [Google Scholar]
[18]. Nkanza NK, Carcinoma of the thyroid at Harare histopathological laboratory (Zimbabwe)Cent Afr J Med 1990 36:34-43. [Google Scholar]
[19]. Omram M, Ahmed ME, Carcinoma of the thyroid in KhartoumEast Afr Med J 1993 70:159-62. [Google Scholar]
[20]. Thomas JO, Ogunbiyi JO, Thyroid cancers in Ibadan, NigeriaEast Afr Med J 1995 72(4):231-33. [Google Scholar]
[21]. Ahmed SA, Rafindadi AH, Iliyasu Y, Shehu SM, Patterns of thyroid cancers in ZariaHighland Medical Research Journal 2007 5(2):7-10. [Google Scholar]
[22]. Tsegaye B, Ergete W, Histopathological pattern of thyroid diseaseEast Afr Med J 2003 80:525-28. [Google Scholar]
[23]. Othman NH, Omar E, Naing NN, Spectrum of thyroid lesions in hospital universiti sains Malaysia over 11-year and a review of thyroid cancers in MalaysiaAsian Pac J Cancer Prev 2009 10:87-90. [Google Scholar]
[24]. Hill AG, Mwangi I, Wanga L, Thyroid disease in a rural Kenyan HospitalEast Afr Med J 2004 81:631-33. [Google Scholar]
[25]. Hussain N, Anwar M, Nadia N, Ali Z, Pattern of surgically treated thyroid diseases in KarachiBiomedica 2005 21:18-20. [Google Scholar]
[26]. Albasri A, Sawaf Z, Hussainy AS, Ahmed Alhujaily A, Histopathological patterns of thyroid disease in Al-Madinah region of Saudi ArabiaAsian Pac J Cancer Prev 2014 15(14):5565-70. [Google Scholar]
[27]. Khan A, Surgical pathology of endocrine and neuroendocrine tumors 2009 New York, NYHumana Press:49 [Google Scholar]
[28]. Ekpechi OL, Pathogenesis of endemic goitre in Eastern NigeriaPrint J Nutr 1967 21:537-45. [Google Scholar]
[29]. Lantum DN, Did universal salt iodization help reduce the infant mortality rate in Nigeria?IDD Newsletter 2009 32(2):6-7. [Google Scholar]
[30]. Egbuta J, Onyezili F, Vanormelingen K, Impact evaluation of efforts to eliminate iodine deficiency disorders in NigeriaPublic Health Nutr 2003 6(2):169-73. [Google Scholar]
[31]. Khairy G, Anaplastic transformation of differentiated thyroid carcinomaInt J Health Sci (Qassim) 2009 3(1):93-96. [Google Scholar]
[32]. Solomon R, Iliyasu Y, Mohammed AZ, Histopathological pattern of thyroid lesions in Kano, Nigeria: A 10-year retrospective review (2002-2011)Niger J Basic Clin Sci 2015 12:55-60. [Google Scholar]
[33]. Togashi S, Oka K, Kanayama R, Koyamatsu S, Tobita T, Yatabe Y, Thyroid anaplastic carcinoma transformed from papillary carcinoma in extrathyroid areaAuris Nasus Larynx 2004 31:287-92. [Google Scholar]
[34]. Besic N, Gazic B, Sites of metastases of anaplastic thyroid carcinoma: Autopsy findings in 45 cases from a single institutionThyroid 2013 23(6):709-13. [Google Scholar]
[35]. Okere P, Olusina DB, Shamim SA, Shandra V, Tushar M, Sellam K, Pattern of second primary malignancies in thyroid cancer patientsNiger J Clin Pract 2013 16:96-99. [Google Scholar]
[36]. Adeyi OA, Pathology services in developing countries-the West African experienceArch Pathol Lab Med 2011 135(2):183-86. [Google Scholar]