Oral cavity is the mirror of general body and so is the oral health an integral part of general health. Dental caries is a complex disease affecting a large proportion of the world. The prevalence of dental caries in developing countries like India is increasing at an alarming level in comparison to the developed countries because of the variety of preventive measures carried out at the community and individual level.
Dental caries is a multifactorial disease. Various host, agent and environmental factors play an important role in the development of dental caries and various strategies for controlling dental caries are focussed on disrupting the interaction between all the risk factors [1].
The best method for prevention of caries includes dietary modification, adequate oral hygiene practices, antimicrobial agents, pit and fissure sealants and use of varnishes. All these measures target the oral microflora. Various antimicrobials have been used in oral cavity with varying efficacy to suppress the growth of microorganisms responsible for dental caries. Among all the species, Streptococcus Mutans (SM) has found to be a predominant organism responsible for dental caries [2]. Longitudinal studies have found a significant association between increased proportion of S. mutans in saliva and incidence of dental caries [2,3].
The varnishes adhere to the tooth surface for longer period and prevent its immediate loss, thus acting as slow-releasing reservoirs [5]. It was stated that though fluoride is one of the most successful agents in caries prevention, it has only limited antimicrobial effect and the other drawback is that it is not advisable in patients with fluorosis and patients with kidney disorders [6].
Chlorhexidine is a broad spectrum anti-microbial agent that has marked caries inhibiting effect. Unfortunately some side effects of chlorhexidine that limit its wide spread use among patients include brown staining on teeth, bitter taste, dulling of taste sensation and epithelial desquamation [7].
The new concept of minimal intervention dentistry was introduced which strives on prevention of the disease by arresting the caries progression [8]. A novel dental caries preventive material Casein Phosphopeptide- Amorphous Calcium Phosphate (CPP-ACP) is a milk product which helps in remineralization and prevents dental caries by forming a calcium phosphate reservoir, buffering the activities of free calcium and phosphate ions, consequently help in maintaining a state of supersaturation that inhibits demineralization and enhances remineralization. Recently, MI varnish was introduced which has the properties of fluoride along with remineralizing properties of CPP-ACP.
Materials and Methods
An in vivo study was designed, analysed and interpreted according to the Consolidated Standards of Reporting Trials (CONSORT). Ethical clearance was obtained from the Institutional Review Board prior to the study which was according to the Declaration of Helsinki for biomedical research involving human subjects. Voluntary written informed consent was obtained from parents and assent from all the children. All patients between 6-12 years of age, visiting the Department of Paedodontics and Preventive Dentistry, KLE University’s KLE VK Institute of Dental Sciences, Belagavi, Karnataka, India, were screened for inclusion and exclusion criteria.
The inclusion criteria includes Decayed-Missing-Filled Teeth/decayed extracted filled teeth score (DMFT/deft) should be 3-5; children residing in Belagavi city and consuming water from same municipal source; written informed consent obtained from the parents/guardians.
The exclusion criteria includes the patient who are suffering from any systemic illness; children with special health care needs; children who were on antimicrobial therapy in past three months; children with any intraoral device/developmental defect.
Sample size: Sample size was calculated by Cohen’s method, with type I error of 0.05 and power of 80%, the sample size to compare mean of three groups with (eta)2 of 0.15 the sample size estimated was 60 i.e., 20 patients per group [9]. Considering 20% drop out in each group, the sample size in each group was 24. The children were allocated into three groups randomly by lottery method.
The study groups were as follows:
Group I: Fluoride varnish applied on 24 subjects (Bifluorid 12, VOCO GmbH, Germany) {Sodium fluoride and calcium fluoride in 6% w/w}
Group II: Chlorhexidine varnish applied on 24 subjects (Cervitec plus, Ivoclar Vivadent, Liechenstein) {Chlorhexidine diacetate 10% w/w and thymol 10% w/w}
Group III: Fluoride varnish with CPP-ACP applied on 24 subjects. (MI, GC Corporation, Japan) {Sodium fluoride 5% w/w and CPP-ACP 2% w/w} [Table/Fig-1].
Shows the three different varnishes used in the study.

Random allocation was done by an investigator who was neither involved in varnish application nor measurement of outcomes, to achieve allocation concealment.
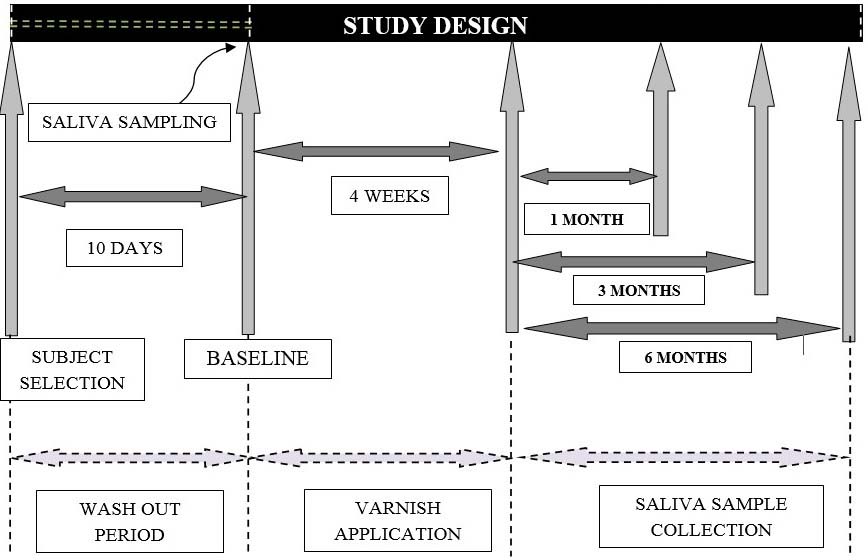
A detailed case history was recorded and the necessary treatment was provided. Oral hygiene instructions, diet counselling and a fluoridated toothpaste were given during the study period. A wash out period of 10 days was kept and the study initiated on 11th day [10] [Table/Fig-2].
Shows the study design followed in the trial.
Saliva Collection
The subjects were asked to refrain from eating or drinking two hours prior to collection of saliva. The saliva was collected between 9 am to 11 am [11]. Collection of sample was carried out by suction method using sterile disposable syringes [12] [Table/Fig-3]. Standardized oral hygiene practices were explained to the patient and reinforced at every visit. Salivary sample was collected and processed for microbiological evaluation of Streptococcus mutans count on four occasions: baseline (before the intervention), 1 month, 3 months and 6 months.
Shows the collection of saliva by suction method.

Varnish Application Procedure
After baseline, saliva samples were obtained from each subject, varnish application was carried out for each subject in the respective groups with the applicator tips using paint on brush technique [Table/Fig-4]. Teeth were dried by the three way syringe and isolated using cotton rolls and saliva ejector. Approximately 0.1 ml of varnish was applied to all the teeth of subjects in the respective group and allowed to dry for 30 seconds. Subjects were instructed not to rinse their mouth, not to eat/drink for three hours and not to brush till the next morning. The procedure was repeated once in every week for four consecutive weeks [13].
Shows the application of varnish using paint on brush technique.

Microbiological Procedure
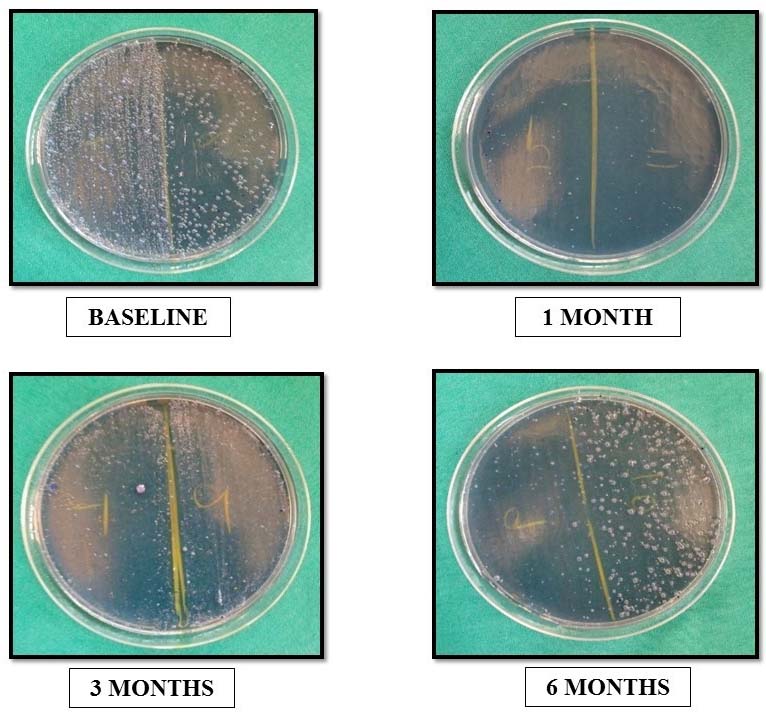
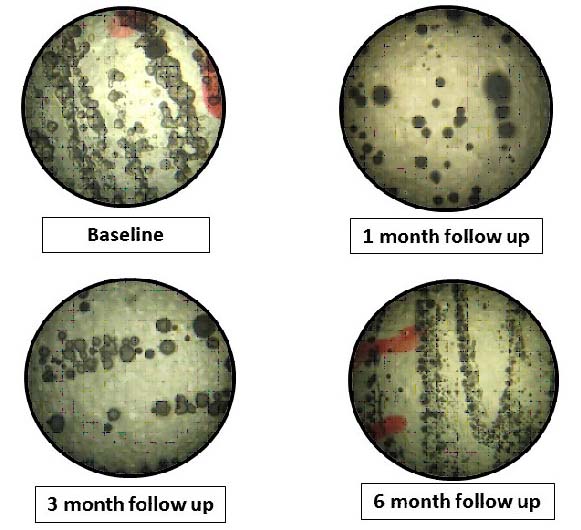
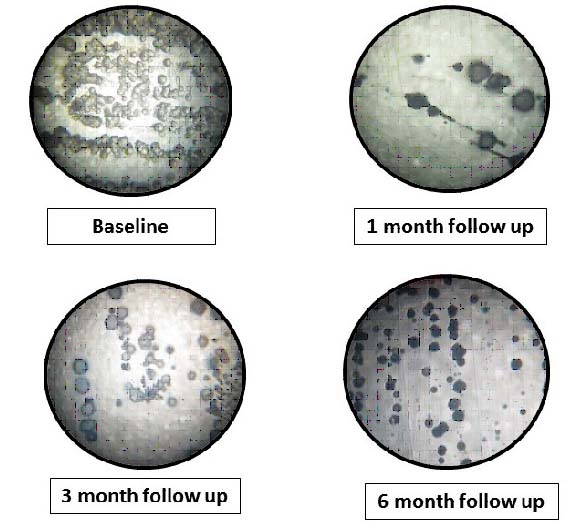
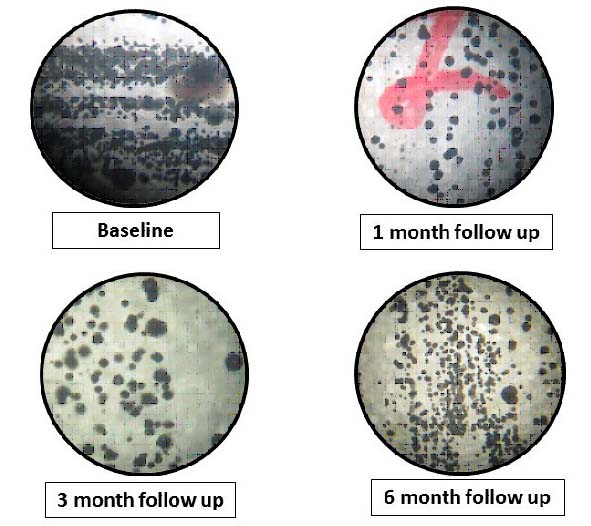
A total of 1ml of unstimulated saliva was collected and put into test tube containing 1ml Reduced Transport Fluid (RTF) and sent for further microbiological procedure and processed within 30 minutes. The saliva samples were diluted in 0.05 M phosphate buffer to the dilution of 1/10 and agitated for 30 seconds on vortex mixer. Almost, 100 μl of the dilution was inoculated each on the Mitis Salivarius Agar with potassium tellurite medium and bacitracin and incubated at 37°C in 5%-10% CO2 jar for 48 hours. After 48 hours, the S. mutans colony was identified using sorbitol fermentation test and Gram staining under light microscope following which the number of colony forming units was determined using stereomicroscope, Labomed SZ 790, (Labomed, Inc. Los Angeles, CA) [Table/Fig-5,6,7 and 8].
Shows microbial growth and colonization of S. mutans at various time intervals.
Showing stereomicroscopic photograph of microbial growth and colonization of S. mutans at various time intervals with respect to fluoride varnish group.
Showing stereomicroscopic photograph of microbial growth and colonization of S. mutans at various time intervals with respect to chlorhexidine varnish group.
Showing stereomicroscopic photograph of microbial growth and colonization of S. mutans at various time intervals with respect to fluoride with CPP-ACP varnish group.
Follow up
The patients were recalled for follow up and collection of saliva was carried out at 1 month, 3 months and 6 months. The dental caries was re-evaluated at the end of 6 months for the new caries lesion development using WHO-Initial Lesion (WHO-IL) Index [14].
Statistical Analysis
All data were subjected to statistical test using SPSS software 20.0 (SPSS Inc., Chicago, IL, USA). One-way ANOVA test for comparison of Streptococcus mutans colony count at baseline. Repeated measures of ANOVA for comparison of Streptococcus mutans colony count at various time intervals. Bonferroni multiple comparison test for inter group comparison of Streptococcus mutans colony count. Intra group comparison at various time points was made by using paired t-test.
Results
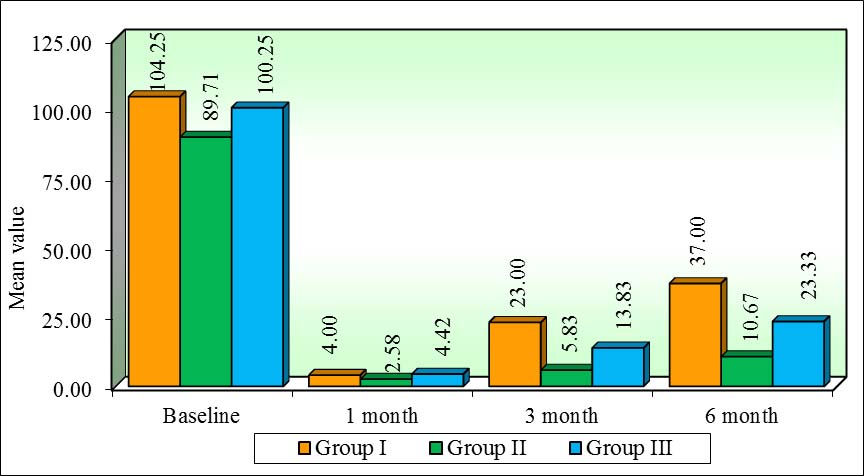
There was no statistically significant difference between the groups with respect to age and DMFT/ deft scores [Table/Fig-9]. One-way ANOVA revealed no statistically significant difference at baseline for all the three groups but at 1 month, 3 month and 6 month time interval there was a significant reduction seen with all the three groups in respect to S. mutans CFU/mL of saliva [Table/Fig-10]. Repeated measures of ANOVA revealed a statistically significant difference among the three group namely Fluoride varnish Group (Group I), Chlorhexidine varnish group (Group II), MI varnish group (Group III), different time points (baseline, 1 months, 3 months, 6 months) and their interactions with S. mutans count at 5% level of significance. Paired t-test was used for the intragroup comparison at different time intervals with respect to S. mutans CFU and it showed a statistically significant result at all the time intervals with maximum reduction in chlorhexidine varnish group at baseline to 1 month and maximum increase in fluoride varnish group at 1 month to 6 month. [Table/Fig-11]. Bonferroni post hoc test was used for the pair wise comparison between the three groups with respect to S. mutans CFU/mL of saliva. A statistically significant result between all the three groups was found with the mean changes were higher between Group I with Group II (14.86) as compared to Group I with Group III (6.60) and Group II with Group III (-8.26) [Table/Fig-12]. Newman-Keuls multiple post-hoc test revealed that a statistically significant result was found between Group II and Group III at 1 month time interval with respect to S. mutans colony count. At 3 month significant results were seen between Group II with Group I, Group III with Group II and Group II with Group III. Similar findings were observed at 6 months interval. [Table/Fig-13,14].
Comparison of mean age and mean DMFT/ deft values of different groups.
| Variable | Group I (24) | Group II (24) | Group III (24) | p-value |
|---|
| Age | 8.33 + 0.91 | 8.62 + 1.63 | 8.75 + 0.26 | 0.564 |
| DMFT/ deft | 4.45 + 1.06 | 4.125 + 0.79 | 4.02 + 0.75 | 0.116 |
Comparison of three groups with respect to salivary S. mutans count at baseline, 1 month, 3 month and 6 month by one-way ANOVA.
| Time points | Summary | Group I | Group II | Group III | F-value | p-value |
|---|
| Baseline | Mean | 104.25 | 89.71 | 100.25 | 2.3558 | 0.1024 |
| SD | 29.01 | 14.84 | 25.75 |
| SE | 5.92 | 3.03 | 5.26 |
| 1 month | Mean | 4.00 | 2.58 | 4.42 | 3.9454 | 0.0239* |
| SD | 2.50 | 2.32 | 2.28 |
| SE | 0.51 | 0.47 | 0.47 |
| 3 month | Mean | 23.00 | 5.83 | 13.83 | 38.2965 | <0.001* |
| SD | 9.67 | 3.38 | 5.81 |
| SE | 1.97 | 0.69 | 1.19 |
| 6 month | Mean | 37.00 | 10.67 | 23.33 | 61.1288 | <0.001* |
| SD | 10.45 | 4.89 | 8.44 |
| SE | 2.13 | 1.00 | 1.72 |
*denotes statistically significant (p<0.05)
Intragroup comparison at different time intervals by paired t-test.
| Groups | Time points | Mean | SD | Mean Diff. | SD Diff. | % of change | Paired t-test | p-value |
|---|
| Group I(FluorideVarnishGroup) | Baseline | 104.25 | 29.01 | | | | | |
| 1 month | 4.00 | 2.50 | 100.25 | 28.67 | 96.16 | 17.1296 | <0.001* |
| Baseline | 104.25 | 29.01 | | | | | |
| 3 month | 23.00 | 9.67 | 81.25 | 28.94 | 77.94 | 13.7542 | <0.001* |
| Baseline | 104.25 | 29.01 | | | | | |
| 6 month | 37.00 | 10.45 | 67.25 | 29.70 | 64.51 | 11.0932 | <0.001* |
| 1 month | 4.00 | 2.50 | | | | | |
| 3 month | 23.00 | 9.67 | -19.00 | 9.31 | -475.00 | -10.0018 | 0.0005* |
| 1 month | 4.00 | 2.50 | | | | | |
| 6 month | 37.00 | 10.45 | -33.00 | 11.03 | -825.00 | -14.6523 | <0.001* |
| 3 month | 23.00 | 9.67 | | | | | |
| 6 month | 37.00 | 10.45 | -14.00 | 10.55 | -60.87 | -6.5010 | <0.001* |
| Group II(CHX VarnishGroup) | Baseline | 89.71 | 14.84 | | | | | |
| 1 month | 2.58 | 2.32 | 87.13 | 14.42 | 97.12 | 29.5991 | <0.001* |
| Baseline | 89.71 | 14.84 | | | | | |
| 3 month | 5.83 | 3.38 | 83.88 | 14.36 | 93.50 | 28.6089 | <0.001* |
| Baseline | 89.71 | 14.84 | | | | | |
| 6 month | 10.67 | 4.89 | 79.04 | 15.41 | 88.11 | 25.1345 | <0.001* |
| 1 month | 2.58 | 2.32 | | | | | |
| 3 month | 5.83 | 3.38 | -3.25 | 3.95 | -125.81 | -4.0328 | 0.0005* |
| 1 month | 2.58 | 2.32 | | | | | |
| 6 month | 10.67 | 4.89 | -8.08 | 4.88 | -312.90 | -8.1140 | <0.001* |
| 3 month | 5.83 | 3.38 | | | | | |
| 6 month | 10.67 | 4.89 | -4.83 | 3.38 | -82.86 | -6.9978 | <0.001* |
| Group III(MI VarnishGroup) | Baseline | 100.25 | 25.75 | | | | | |
| 1 month | 4.42 | 2.28 | 95.83 | 26.29 | 95.59 | 17.8588 | <0.001* |
| Baseline | 100.25 | 25.75 | | | | | |
| 3 month | 13.83 | 5.81 | 86.42 | 25.90 | 86.20 | 16.3440 | <0.001* |
| Baseline | 100.25 | 25.75 | | | | | |
| 6 month | 23.33 | 8.44 | 76.92 | 26.64 | 76.72 | 14.1460 | <0.001* |
| 1 month | 4.42 | 2.28 | | | | | |
| 3 month | 13.83 | 5.81 | -9.42 | 5.26 | -213.21 | -8.7739 | <0.001* |
| 1 month | 4.42 | 2.28 | | | | | |
| 6 month | 23.33 | 8.44 | -18.92 | 8.34 | -428.30 | -11.1116 | <0.001* |
| 3 month | 13.83 | 5.81 | | | | | |
| 6 month | 23.33 | 8.44 | -9.50 | 8.11 | -68.67 | -5.7363 | <0.001* |
* denotes statistically significant (p< 0.05)
Pair wise comparison of three groups with respect to salivary S. mutans count at different time intervals.
| Groups | Mean Difference | Std. Error | p-value |
|---|
| Group I(Fluoride Varnish Group) | Group II | 14.865 | 2.3670 | <0.001* |
| Group III | 6.604 | 1.5570 | <0.001* |
| Group II(CHX Varnish Group) | Group I | -14.865 | 2.3670 | <0.001* |
| Group III | - 8.260 | 1.8550 | <0.001* |
| Group III(MI Varnish Group) | Group I | -6.604 | 1.5570 | <0.001* |
| Group II | 8.260 | 1.8550 | <0.001* |
* denotes statistically significant (p<0.05)
Pair wise comparison of three groups with respect to salivary S. mutans count at different time intervals.
| Time points | Groups | Group I | Group II | Group III |
|---|
| Baseline | Mean | 104.25 | 89.71 | 100.25p=0.8324- |
| Group I | - | p=0.0972 |
| Group II | | - |
| Group III | - | p=0.2866 |
| 1 month | Mean | 4.00 | 2.58 | 4.42p=0.8158- |
| Group I | - | p=0.1037 |
| Group II | | - |
| Group III | | p=0.0248* |
| 3 month | Mean | 23.00 | 5.83 | 13.83p≤0.001*- |
| Group I | - | p≤0.001* |
| Group II | | - |
| Group III | | p=0.0004* |
| 6 month | Mean | 37.00 | 10.67 | 23.33p≤0.001*- |
| Group I | - | p≤0.001* |
| Group II | | - |
| Group III | | p≤0.001* |
* denotes statistically significant (p<0.05)
Comparison of three groups (I, II, III) with respect to Streptococcus mutans count X 105 CFU/ml of saliva at baseline, 1 month, 3 month and 6 month.
Discussion
The present study compared the effect of fluoride varnish, chlorhexidine varnish and fluoride varnish containing CPP-ACP with intensive application regimen on S. mutans levels in saliva using microbiological methods under randomized controlled clinical trial settings.
Children between 6-12 years of age were included in the study because at this age they are highly susceptible to dental caries and undergoing multiple permanent tooth eruption. A second window of infectivity was seen between 6-12 years during the eruption of permanent dentition as suggested by Caufield PW et al., thus showing increased acquired SM and its correlation to an increase in dental hard-tissue surface when the permanent teeth start erupting [15]. Many researchers have found that the most frequent variable in caries risk assessment model is one that describes past caries experience. Thus in this trial, DMFT/deft 3-6 was considered as one of the inclusion criteria indicating child at moderate-to-high caries risk. This is in accordance with caries risk assessment tool given by American Academy of Paediatric Dentistry (AAPD) in 2011 [16].
Saliva a multi-constituent oral fluid regulates and maintains the integrity of the oral mucosa and therefore plays a very important role in maintaining the oral health. Saliva and plaque can be used for the estimation of S. mutans count. Due to the ease of sampling and processing, saliva was used in the study [17]. Unstimulated saliva was used as it has lower concentration of bicarbonate ions thus reducing the bias due to the buffering action of saliva. In our study, suction method was used for collection of saliva from the floor of mouth using sterile disposable syringe to avoid any contamination and its ease of use. Salivary flow rate shows a circadian rhythm so for standardization salivary samples were taken between 9 am-11 am in order to minimize the effect of circadian rhythm on the samples [11].
All the required restorative treatment was carried out before the application of varnishes for elimination of apparent retention sites (such as caries lesions and defective fillings) to reduce the level of Streptococcus mutans in plaque. A wash out period of 10 days was kept in our study to prevent any effect of restorative material on the result of the study [10].
Messer LB states, that the chlorhexidine varnish should be more frequently used in high risk children [18]. To accomplish a reservoir of chlorhexidine on the tooth surface, a single application of a highly concentrated varnish is sufficient even with reduced contact time. However, for varnishes with low concentration like Cervitec, repeated application and a longer retention time is required. Studies showed that fluoride varnish with four application in a month reduced and controlled the caries activity [19]. Thus, in our study an intensive regime was carried out which was in accordance to study done by Sandham HJ [13].
Fluoride varnish was first developed in 1960s and 1970s to prolong the contact time between fluoride and enamel. Fluoride exerts its cariostatic effect by its presence in the oral fluids bathing the dental hard tissues. The main action of fluoride is to retard demineralization and promote remineralization of enamel and dentin by the uptake of calcium and phosphates of saliva [20]. It also inhibits glucose transport, carbohydrate storage, and extracellular polysaccharide formation by interfering with enolase enzyme in microorganisms.
On the other hand, chlorhexidine has proved to be better antimicrobial agent against S. mutans. Chlorhexidine attaches to the glycoproteins by reversal electrostatic binding and thus gets retained on to the oral surfaces. In smaller concentrations, such as in Cervitec plus (1% Chlorhexidine) varnish, it has hydrophilic– hydrophobic properties and a bacteriostatic effect that interferes with membrane transport, allowing its light-weight molecules to infiltrate into the offending microorganism [21,22].
A novel material CPP-ACP is a product derived from milk, which strengthens and remineralizes the tooth structure and also has anticariogenic properties [23]. The CPP helps to stabilize Amorphous Calcium Phosphate (ACP) in the form of multiphosphoseryl sequences. CPP binds to ACP and thus prevents the dissolution of calcium and phosphate ions. The CPP-ACP helps in facilitating remineralization and maintaining it in supersaturated form by acting as a reservoir of bio-available calcium and phosphate [24]. CPP also has shown to decrease the count of S. mutans as it has got the ability to integrate in the salivary pellicle thus inhibiting its adherence [25]. The synergistic effect of CPP-ACP with fluoride present in MI varnish showed lower demineralisation and higher remineralization potential [26].
In the study when intragroup analysis was carried out at different time intervals it was found out that, in all the three groups, there were significant differences in S. mutans CFU values between the different time intervals with highest reduction observed in chlorhexidine group at baseline to 1 month [Table/Fig-11]. The results were in accordance to the study done by Twetman S and Peterson LG where drastic reduction of S. mutans CFU in saliva was seen at 1 month time interval followed by slight reduction at 3 months interval [27]. Similar results were seen in a clinical study by Sandham HJ, Paul S [28,29]. This short term effect is due to release of the active agent into the milieu within a relatively short period of time. The initial effect is due to the phenomenon called ‘burst effect’.
When intergroup comparison of S. mutans colony count at different time interval were seen it was observed that at baseline there were no statistically significant result between the three groups. At 1 month interval a statistically significant result was observed between the chlorhexidine varnish group and MI varnish but no significant result between the other groups stating the higher antimicrobial efficacy of chlorhexidine varnish in comparison to MI varnish.
At 3 and 6 month interval, significant result were seen between the three groups with chlorhexidine varnish showing the highest efficacy followed by MI varnish and least effective being the fluoride varnish group, this might be due to the property of substantivity showed by chlorhexidine group [Table/Fig-12,13]. Similar result was seen by Ekenbach SB et al., comparing the effect of chlorhexidine and fluoride varnishes on exposed sound root surfaces that found treatment with Cervitec varnish effective until 6 months as compared to fluoride varnish [30]. Similar findings were seen in a clinical study by Sandham HJ and Joharji RM [28,31].
Varnish containing fluoride with CPP-ACP was found to be effective in comparison to fluoride varnish group this could be due to the additive anticariogenic effect of CPP-ACP and fluoride attributable to localization of ACPF at the tooth surface by the CPP which in effect would co-localize calcium, phosphate and fluoride thus forming a reservoir and for slow and prolong release of ions for a longer period of time as seen in our study. Duraisamy V et al., stated that fluoride varnish with CPP-ACP was superior to fluoride or CPP-ACP applied alone [26]. This is in accordance with our study where similar results were found proving the synergistic effect of fluoride varnish with CPP-ACP.
At the end of 6 months, we found no new carious lesion in all the three study groups as per WHO-IL index proving that all the three varnishes were effective in caries prevention [14].
The limitations of our study are smaller sample size and short follow up period. A larger geographical area should be covered in order to substantiate the results of the present study.
Conclusion
All the three varnishes namely fluoride varnish, chlorhexidine varnish and MI varnish showed an antibacterial effectiveness against salivary S. mutans at all time intervals. Among the three varnishes, chlorhexidine varnish showed maximum reduction in salivary S. mutans as compared to MI varnish and fluoride varnish at 1 month, 3 months and 6 months intervals respectively.
*denotes statistically significant (p<0.05)
* denotes statistically significant (p< 0.05)
* denotes statistically significant (p<0.05)
* denotes statistically significant (p<0.05)