Unfolding of a Clinically Suspected Case of Pulmonary Tuberculosis
Savitha Thirouvengadame1, Swapna Muthusamy2, Vignesh Kanna Balaji3, Joshy Maducolil Easow4
1 Undergraduate Student, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India.
2 Assistant Professor, Department of Microbiology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India.
3 Postgraduate Student, Department of Microbiology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India.
4 Senior Consultant Microbiologist, Nirmal Laboratories, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swapna Muthusamy, Assistant Professor, Department of Microbiology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry-605102, India.
E-mail: swapnamuthuswamy@gmail.com
Pulmonary nocardiosis caused by Nocardia mimics pulmonary tuberculosis in many aspects. Here, we report a case of suspected pulmonary tuberculosis turning into pulmonary nocardiosis following microbiological evaluation. Sputum sample of the patient grew Nocardia otitidiscaviarum. Identification was done by conventional methods and matrix assisted laser desorption ionization-time of flight. He was given co-trimoxazole based on susceptibility reports. Even though Nocardia is a rare entity, pulmonary nocardiosis should be ruled out before starting antitubercular treatment to avoid unnecessary burden to the patient and community.
Modified Kinyoun’s technique, Nocardia otitidiscaviarum, Pulmonary nocardiosis
Case Report
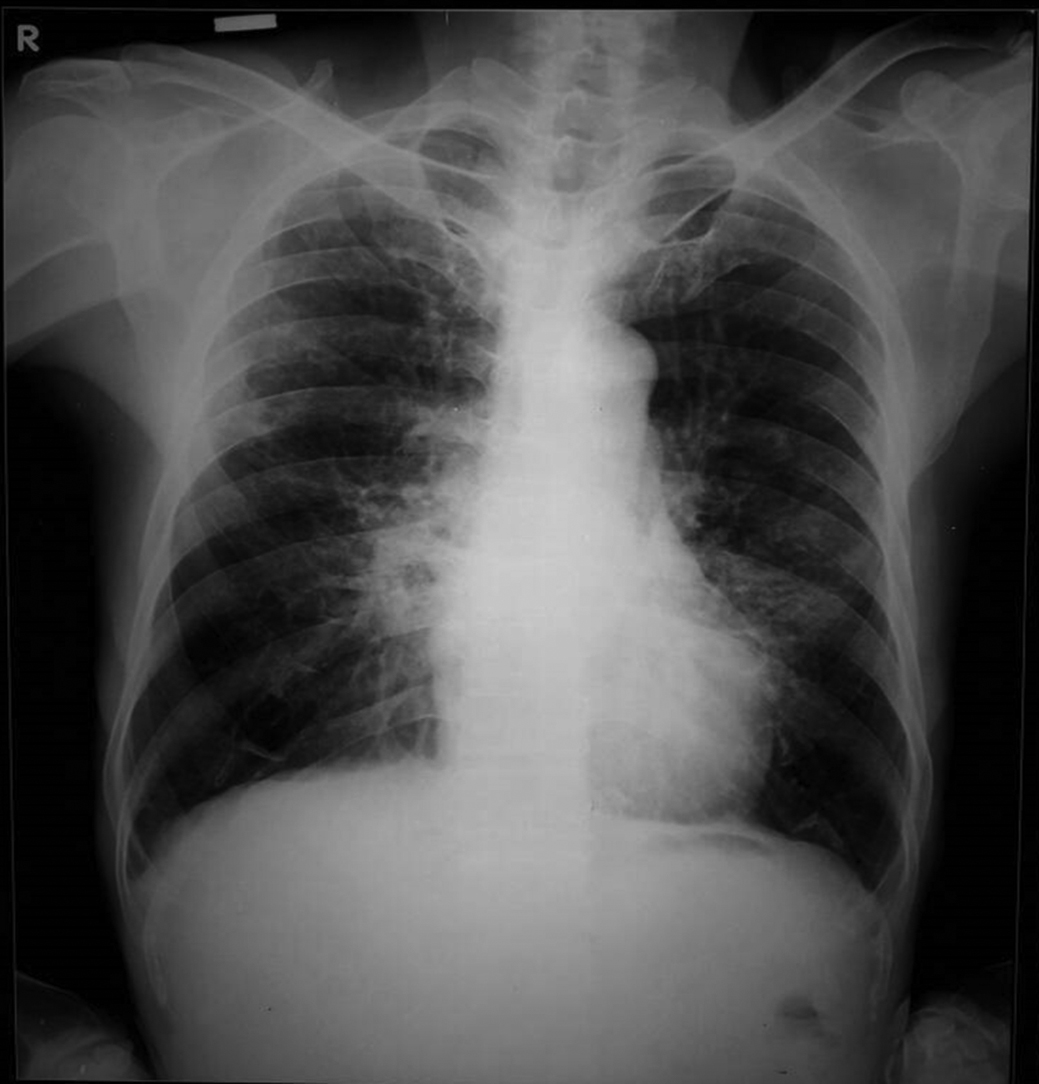
A 65-year-old male presented to our hospital with complaints of intermittent cough and breathlessness for the past three months. He also complained of loss of weight and appetite for the same duration. There was no significant history like exposure to known case of tuberculosis or treatment for pulmonary diseases. On examination, respiratory sounds were harsh with no added sounds. Sputum was sent for routine Acid Fast Bacilli (AFB) staining to look for Mycobacterium tuberculosis. Chest radiography showed infiltrative lesions in the middle zone of both lungs [Table/Fig-1]. Since sputum AFB smear was negative, he was clinically diagnosed as a case of smear-negative pulmonary tuberculosis and was planned to start on antitubercular treatment.
Chest radiography posteroanterior view.
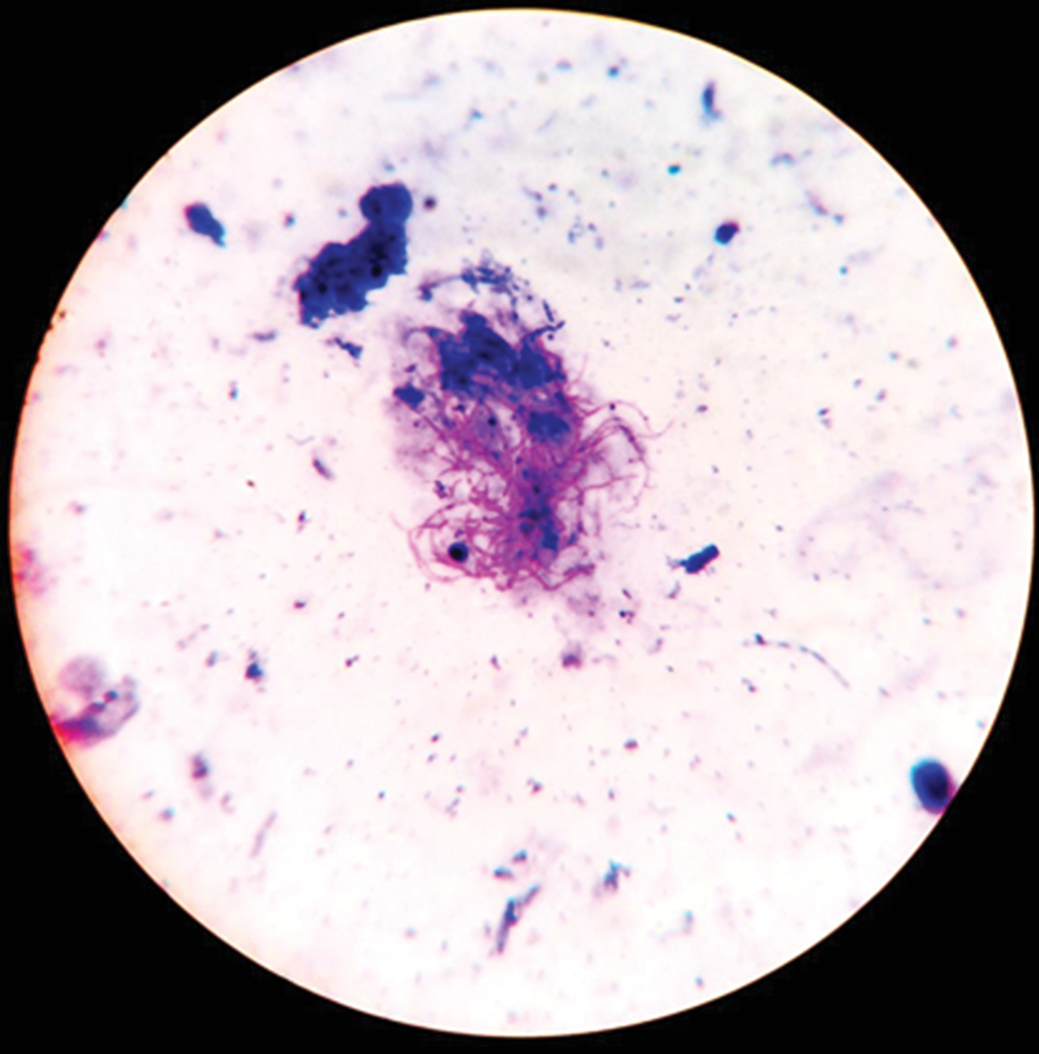
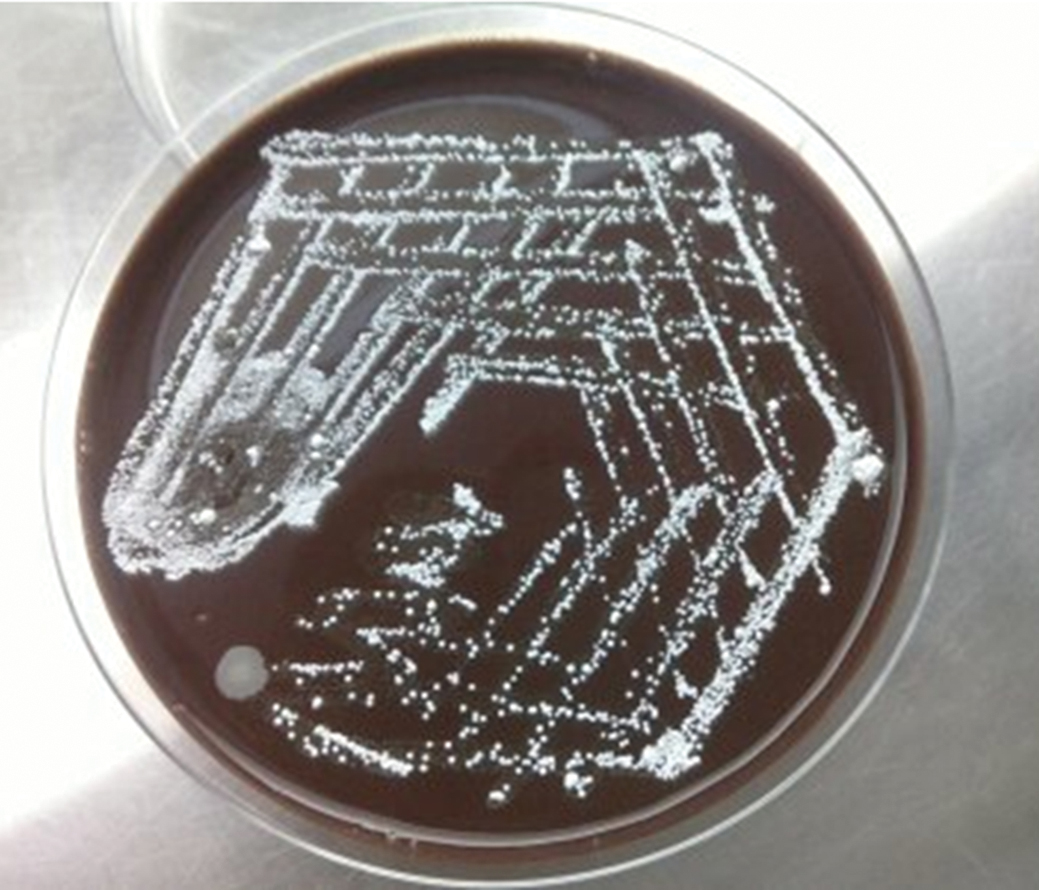
As a part of another study (screening of all sputum samples for Nocardia), this patient’s sample was also screened for Nocardia by Gram-staining and modified Kinyoun’s technique. Two smears were prepared from the purulent sputum. The first slide was stained by Gram-stain and second by modified Kinyoun’s technique using 1% sulfuric acid as decolorizer [Table/Fig-2]. For culture, the sample was inoculated on chocolate agar and incubated at 37°C for 4 days [Table/Fig-3]. Gram-staining showed Gram-positive filaments and modified Kinyoun’s technique showed pink colored acid-fast filamentous bacilli. Chocolate agar showed dry, chalky white colored colonies after 72 hours of incubation. Gram-staining and modified Kinyoun’s technique performed from culture was consistent with direct smear findings suggestive of Nocardia. Genus identification was done by characteristic colony morphology, microscopic appearance in Gram-staining, modified Kinyoun’s technique from culture and species identification was performed by Matrix-Assisted Laser Desorption/Ionization-Time Of Flight (MALDI-TOF) proteomic study (MALDI-TOF MS Biotyper version 2.02, Bruker Corporation). Antibiotic susceptibility test was performed by Vitek-2 system (Biomerieux) following manufacturer’s instructions and Clinical Laboratory Standards Institute guidelines for interpretation. As per the minimum inhibitory concentration values shown in [Table/Fig-4], the isolate was susceptible to amikacin, gentamicin, co-trimoxazole, ceftriaxone, imipenem, linezolid, and resistant to amoxicillin-clavulanic acid. Isolate was sent to Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, where molecular characterization using 16S ribosomal DNA sequencing also confirmed the identity as Nocardia otitidiscaviarum.
Nocardia spp. microscopic view with modified Kinyoun’s technique under ×400 magnification.
Nocardia spp. macroscopic view of culture on chocolate agar.
MIC values of Nocardia spp. by Vitek-2 system (Biomerieux).
| Antibiotic | MIC value (μg/ml) | Interpretation |
|---|
| Amikacin | 1 | Susceptible |
| Gentamicin | 0.125 | Susceptible |
| Imipenem | 0.25 | Susceptible |
| Amoxycillin-clavulanic acid | 256 | Resistant |
| Ceftriaxone | 2 | Susceptible |
| Linezolid | ≤4 | Susceptible |
| Cotrimoxazole | 1 | Susceptible |
MIC: Minimum inhibitory concentration
The patient was given oral cotrimoxazole (2 double-strength 160 mg trimethoprim/800 mg sulfamethoxazole twice daily) for 12 weeks with dose reduction after four weeks. He was advised to come for follow-up at the end of four weeks, during which the patient had improved clinically and repeat samples were negative for Nocardia.
Discussion
Nocardia is Gram-positive, weakly acid-fast, dichotomous branching bacilli [1]. The principle species giving rise to nocardiosis are Nocardia asteroides, Nocardia farcinica, and Nocardia nova. They have been implicated as a cause of cutaneous, ocular, pulmonary, and disseminated nocardiosis [2], of which pulmonary nocardiosis is the most common [3].
Clinical and radiological picture of pulmonary nocardiosis and tuberculosis are similar, and hence laboratory tests are required to distinguish the two. Identification and antibiotic susceptibility testing of Nocardia are essential to formulate empirical therapy, to understand their disease spectrum and geographical distribution [4]. In this case, microbiological evaluation clinched the diagnosis as pulmonary nocardiosis and contributed to the better management of the patient.
Based on the few studies documented on nocardiosis in India, there is a recent increase in the prevalence rate of nocardiosis [5]. A study on nocardiosis in a tertiary care center has shown that male-to-female ratio was 1.4:1, and the mean age was 54.6 years [6]. There exists a marked difference in the incidence of pulmonary nocardiosis between sexes, with a high predominance among men [7]. A study done in Yemen has revealed that 70% of their subjects had pulmonary tuberculosis and 30% had other pulmonary infections [8]. Another study showed that the most common comorbid condition associated with pulmonary nocardiosis was underlying pulmonary disease [9]. This is also evident from the case report on tuberculosis with pulmonary nocardiosis in a patient with HIV [10]. However, our patient did not have any associated comorbid conditions or pulmonary diseases.
Nocardia was identified in our patient’s sample by Gram-staining, modified Kinyoun’s technique and culture. Nocardia genus identification was done based on colony morphology, Gram-stain and modified Kinyoun’s technique. Genus confirmation and species identification as N. otitidiscaviarum were performed by MALDI-TOF. Molecular characterization using 16S ribosomal DNA sequencing also confirmed the identity. Antibiotic susceptibility test performed by Vitek-2 system showed that the isolate was susceptible to all the tested drugs except amoxicillin-clavulanic acid [Table/Fig-4]. The case report by Shahapur PR et al. has shown that N. otitidiscaviarum was resistant to co-trimoxazole, but our isolate was susceptible and the patient responded well to co-trimoxazole [11].
Nocardiosis is a low prevalence disease. There are studies that had reported zero prevalence. A study done in Yemen is one among them which included 500 study subjects and reported zero prevalence [8]. High incidence of 4.33% nocardiosis has been reported in Arak, Iran [12]. For isolation of Nocardia spp., paraffin bait technique is claimed to be more effective than the conventional culture for isolation of Nocardia [13]. Molecular methods are useful in identifying Nocardia to the species level which includes restriction endonuclease analysis of 16S rRNA gene, restriction fragment length polymorphism analysis of the amplified hsp 65 and sequencing of 16S rRNA or DNA [14]. Unfortunately, such molecular studies are often limited to research-oriented laboratories and are rarely performed in routine clinical laboratories. According to Brown-Elliott et al., possible reasons for reduced isolation of Nocardia were readily responsive nature of Nocardia to the empirical antimicrobial treatment given for other common infections and slow growing nature compared to commensal flora of the respiratory tract [15].
In our case, nocardiosis was neither suspected, nor specific investigations were ordered, and diagnosis was established purely by chance.
Conclusion
Every patient suspected of pulmonary tuberculosis should be investigated for nocardiosis to avoid unnecessary burden to the patient and society. Microbiologists must be informed in such cases, to perform specific laboratory investigation like modified Kinyoun’s technique to detect Nocardia.
MIC: Minimum inhibitory concentration
[1]. D’Cruz S, Bhadada S, Chander J, Agarwal V, Singh R, Sachdev A, Isolated nocardial subcapsular and perinephric abscessIndian J Pathol Microbiol 2004 47(1):24-6. [Google Scholar]
[2]. Srifuengfung S, Poonwan N, Tribuddharat C, Chokephaibulkit K, Prevalence of Nocardia species isolated from patients with respiratory tract infections at Siriraj Hospital, ThailandJ Infect Dis Antimicrob Agent 2007 24(1):1-6. [Google Scholar]
[3]. Wilson JW, Nocardiosis: Updates and clinical overviewMayo Clin Proc 2012 87(4):403-7. [Google Scholar]
[4]. Aravantagi A, Patra KP, Broussard M, Jones K, A case of Nocardia transvalensis pneumonia in a 19-year-old cystic fibrosis patientLung India 2012 29(3):283-85. [Google Scholar]
[5]. Taruna S, Sanju P, Sharma BP, Pulmonary nocardiosis in immunocompromised patients of BikanerInt J Basic Appl Med Sci 2013 3:362-66. [Google Scholar]
[6]. Wang HK, Sheng WH, Hung CC, Chen YC, Lee MH, Lin WS, Clinical characteristics, microbiology, and outcomes for patients with lung and disseminated nocardiosis in a tertiary hospitalJ Formos Med Assoc 2015 114(8):742-49. [Google Scholar]
[7]. Garcia-Bellmunt L, Sibila O, Solanes I, Sanchez-Reus F, Plaza V, Pulmonary nocardiosis in patients with COPD: Characteristics and prognostic factorsArch Bronconeumol 2012 48(8):280-85. [Google Scholar]
[8]. Al-Robasi AA, Al-Madhagi A, Association of nocardiosis with pulmonary tuberculosis in YemenFac Sci Bull 2009 22:1-5. [Google Scholar]
[9]. Alavi Darazam I, Shamaei M, Mobarhan M, Ghasemi S, Tabarsi P, Motavasseli M, Nocardiosis: Risk factors, clinical characteristics and outcomeIran Red Crescent Med J 2013 15(5):436-39. [Google Scholar]
[10]. Kumar A, Mehta A, Kavathia G, Madan M, Pulmonary and extra pulmonary tuberculosis along with pulmonary nocardiosis in a patient with human immune deficiency virus infectionJ Clin Diagn Res 2011 5(1):109-11. [Google Scholar]
[11]. Shahapur PR, Peerapur BV, Shahapur RP, Honnutagi RM, Biradar MS, Lymphocutaneous nocardiosis caused by Nocardia otitidiscaviarum: A case report and review of literatureJ Nat Sci Biol Med 2014 5(5):197-201. [Google Scholar]
[12]. Abtahi H, Saffari M, Jourabchi A, Rafiei M, Pulmonary nocardiosis and its related factors in patients with pulmonary infection in ArakJ Kashan Univ Med Sci Spring 2003 7:87-91. [Google Scholar]
[13]. Bareja R, Jindal RC, Vohra P, Grover PS, Evaluation of various techniques for the detection of Nocardia species in clinically evident cases of pulmonary and extrapulmonary tuberculosisIOSR J Dent Med Sci 2014 13(1):65-70. [Google Scholar]
[14]. Rudramurthy SM, Honnavar P, Kaur H, Samanta P, Ray P, Ghosh A, Molecular identification of clinical Nocardia isolates from IndiaJ Med Microbiol 2015 64(10):1216-25. [Google Scholar]
[15]. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ, Clinical and laboratory features of the Nocardia spp. Based on current molecular taxonomyClin Microbiol Rev 2006 19(2):259-82. [Google Scholar]