A Case Series on Superior Mesenteric Artery Syndrome Surgical Management, Single Institution Experience
Gopakumar Valiathan1, Majid Wani2, Juneed Lanker3, Prasanna Kumar Reddy4
1 Registrar, Department of Surgical Gastroenterology, Apollo Main Hospitals, Chennai, Tamil Nadu, India.
2 Registrar, Department of Surgical Gastroenterology, Minimal Access Surgery, Apollo Main Hospitals, Chennai, Tamil Nadu, India.
3 Registrar, Department of Surgical Gastroenterology, Minimal Access Surgery, Apollo Main Hospitals, Chennai, Tamil Nadu, India.
4 Senior Consultant, Surgical Gastroenterologist and Laparoscopic Surgeon, Department of Surgical Gastroenterology, Apollo Hospitals, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gopakumar Valiathan, Sreenilayam, Thonnalloor, Pandalam-698501, Kerala, India.
E-mail: gopancv@gmail.com
Compression of duodenum by Superior Mesenteric Artery (SMA) causing proximal intestinal obstruction is an uncommon condition. Treatment of this condition involves conservative management initially followed by surgical management in those patients who have persistent symptoms. This case series evaluates surgical management and outcome of six patients after one year, who presented with SMA syndrome and describes a brief review of literature. Three patients underwent open duodenojejunostomy and the rest three underwent laparoscopic duodenojejunostomy. All patients had uneventful postoperative recovery. Postoperative requirement of analgesics was less in laparoscopic group versus open group. All the three patients in laparoscopic group could be mobilised out of bed on the day of the surgery itself. Mean duration of hospital stay was seven days for open surgery group and three days for the laparoscopy group. Outcome in terms of resolution of abdomen pain and vomiting was similar in both the groups. Four patients were asymptomatic after one year of follow up. A high index of clinical suspicion is needed for the diagnosis of SMA syndrome. Laparoscopic approach is feasible, safe, less morbid and effective as compared to open surgery. In the presence of facilities and surgical expertise, laparoscopic duodenojejunostomy should be considered the procedure of choice for SMA syndrome. Majority of patients remain symptom free at one year follow up.
Aortomesenteric angle, Duodenojejunostomy, Laparoscopic approach
SMA syndrome, caused by compression of duodenum by SMA causing proximal intestinal obstruction is an uncommon condition. It should be treated by conservative management initially followed by surgical management in those patients who have persistent symptoms.
Case Series
From the hospital case record, a total of six cases were identified during duration of five years from January 2010 to May 2015 [Table/Fig-1]. The mean age of patients was 20 years (17-31 years). The male to female ratio was 2:1. Postprandial vomiting associated with upper abdominal discomfort was the most common presentation. A history of significant weight loss was present in two patients. Associated predisposing factors could be identified in three patients. Two patients had restricted their diet due to concern of their body image resulting in weight loss. One patient had a scoliosis correction surgery six months before the onset of SMA syndrome. In our series patients were operated after a mean period of two months if symptomatic on conservative management.
Clinical profile of patients.
| Cases | Age | Sex | Symptoms | Aortomesenteric angle | Management | Follow up at 1 year |
|---|
| Case 1 | 17 years | Male | Upper abdominal pain, vomiting | 7 degrees | Open duodenojejunostomy | Pain resolved, occasional vomiting |
| Case 2 | 17 years | Male | Postprandial bilious vomiting | 12 degrees | Laparoscopic duodenojejunostomy | Continues to have vomiting once in a month |
| Case 3 | 31 years | Male | Postprandial upper abdominal pain | 10 degrees | Open duodenojejunostomy | Asymptomatic |
| Case 4 | 20 years | Female | Postprandial non bilious vomiting | 11 degrees | Open duodenojejunostomy | Asymptomatic |
| Case 5 | 22 years | Male | Postprandial bloating, upper abdominal pain | 10 degrees | Laparoscopic duodenojejunostomy | Asymptomatic |
| Case 6 | 17 years | Female | Upper abdominal pain, vomiting | 12.5 Degrees | Laparoscopic duodenojejunostomy | Asymptomatic. |
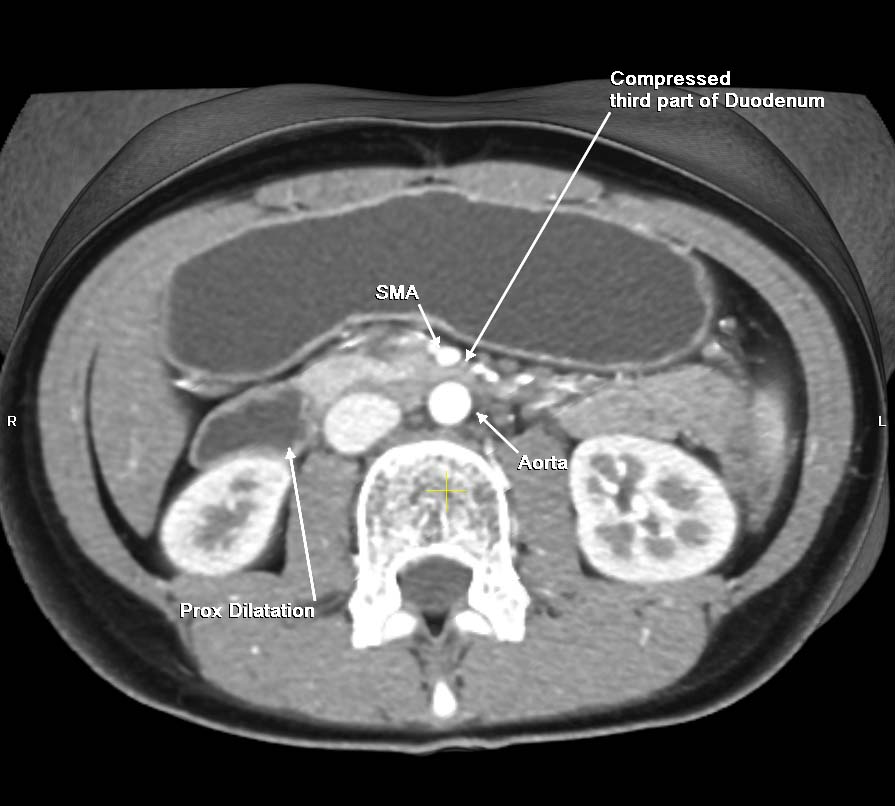
Evaluation of patients: All patients underwent an upper gastrointestinal endoscopy and 320 slice CECT abdomen evaluation [Table/Fig-2,3]. Upper gastrointestinal endoscopy was normal in four patients; two patients had mid dilatation of second part of duodenum. The aortomesenteric angle was assessed on reconstructed arterial images on CT scan [Table/Fig-4]. The mean aortomesenteric angle was 10.5 degrees in six patients (range 7-12.5 degrees).
A 320 slice CECT abdomen axial section showing compressed distal third part of duodenum between SMA and aorta and proximal dilatation.
Sagittal reconstruction image showing grossly dilated second and third part of duodenum and stomach.

CT angiogram showing narrowing of aortomesenteric angle.

All the six patients eventually underwent surgical intervention because of persisting symptoms, three each by open and laparoscopy approach.
Operative Technique
a) Open approach: Approach was by upper midline incision. The side to side anastomosis was done between second part of duodenum and a loop of jejunum, about 30 cm distal to duodenojejunal flexure. The anastomosis was performed in two layers in all patients. Wound was closed en masse.
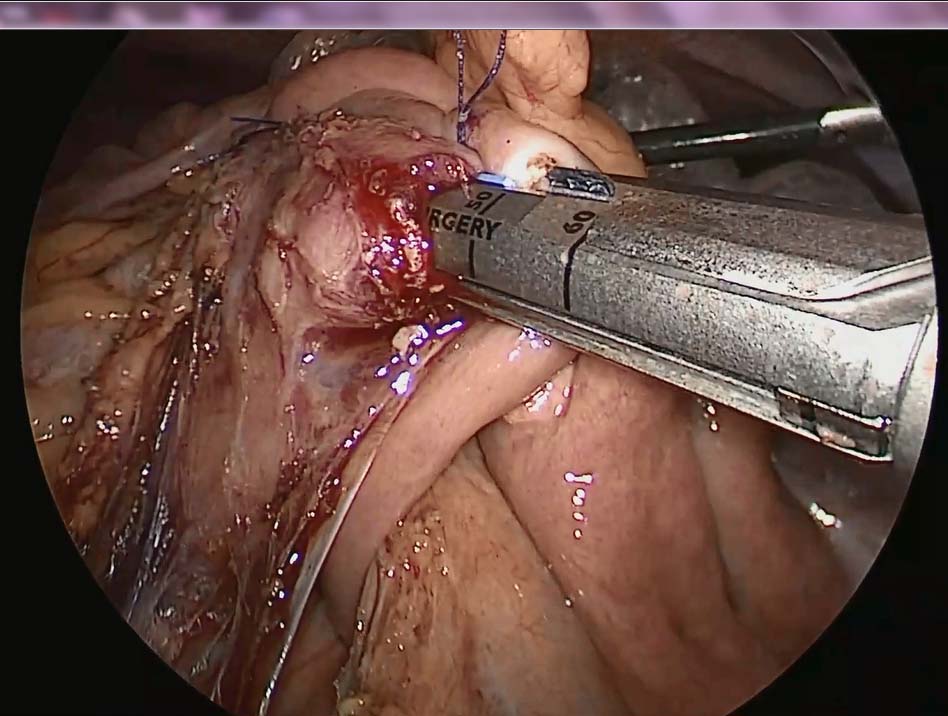
b) Laparoscopic approach: The patient was placed in a 20° head-up supine-split leg position. Operating surgeon stood in between the legs of patient, camera assistant on the right side of patient, scrub nurse and second assistant on the left side of the patient. Pneumoperitoneum was established using Veress needle technique. Port position was: 10-mm port at the umbilicus for a 30° telescope, a 5-mm port in the epigastrium for liver retraction, a 10-mm working port in the right subcostal region and a 5-mm working port in the left subcostal region. The transverse colon was lifted up. Dilated duodenum was seen in the infra-colic compartment. SMA pulsations could be seen to the right side of the dilated third part of duodenum. The visceral peritoneum overlying second and third part of duodenum was divided using harmonic scalpel and this part of the duodenum was freely mobilized. A loop of jejunum about 30 cm from the duodenojejunal flexure was brought up to the duodenum. Stay sutures were applied intracorporeally with 2-0 silk to keep both segments in approximation. A small opening was made in both the duodenum and jejunum with harmonic scalpel. One of the jaws of a 45-mm EndoGIA echelon stapler was introduced into the lumen of the jejunum, and the other jaw was introduced into the lumen of the duodenum and stapler was fired [Table/Fig-5]. The common opening thus created was closed intracorporeally using 2-0 Vicryl continuous sutures in a single layer. The duodenojejunal anastomosis was side-to-side, and the size of the lumen was about 4.5 cm. Methylene blue leak test was performed to ascertain the integrity of anastomosis. A 28 Fr tube drain was kept adjacent to the site of anastomosis. 10 mm port sites were closed in layers and 5 mm port sites with steristrips.
Laparoscopic view of duodenojejunostomy anastomosis being performed with Echelon 45 EndoGIA staplers.
Patients were kept nil by mouth for two days and started on liquid diet on the third day. Drain was removed on postoperative day three. The mean operating time was 105 minutes in the open versus 130 minutes in the laparoscopy group. Postoperative analgesic requirement was significantly low in laparoscopic group compared to open group. All the three patients in laparoscopic group could be mobilised out of bed on the day of the surgery itself while as patients in open group could be mobilised out of bed on the next day of the surgery. Mean duration of hospital stay was four days less in the laparoscopic group compared to the open group. All patients except one had resolution of upper abdominal pain and vomiting at one year follow up [Table/Fig-1].
Discussion
SMA syndrome is an uncommon cause of duodenal obstruction. It was first described by the Austrian professor C Von Freiherr Rokitansky in 1861 as an autopsy finding, later described in detail by Wilkie in a case series of 64 patients [1,2]. The reported incidence in some studies is about 0.1% to 0.3% [3]. Even though about 400 cases are described in English literature, many had expressed doubt about the true existence of such condition. It often poses a diagnostic dilemma, often diagnosed after excluding other conditions. The SMA usually forms an angle of about 45 degrees (38- 56 degrees) with the aorta. SMA syndrome is presumed to be present if the aortomesenteric angle is less than 25 degrees in adults [4]. The aortomesenteric distance in SMA syndrome is decreased to 2-8 mm (normal is 10-20 mm). Other anatomical causative factors implicated includes the high insertion of duodenum at the ligament of Treitz, low origin of SMA, compression of duodenum due to peritoneal adhesions [5]. Acquired predisposing factors include scoliosis surgery, spinal trauma, total proctocolectomy with ileal J pouch, application of abdominal casts, body image disorder such as anorexia nervosa, paraduodenal hernias, and abdominal aortic aneurysm [6]. Young females (18-35 years) are frequently affected by this condition. This age and sex distribution is likely related to the over concern with body image and eating disorders [7]. As many as 40% of patients have no apparent explainable cause.
Symptomatology of this condition is often non-specific. Clinical presentation include an acute onset or a more gradual onset of postprandial abdominal fullness and early satiety. Abdominal symptoms are aggravated by supine position and relieved by lateral decubitus or prone position. Patients with significant obstruction of duodenum may present with bilious emesis, weight loss and electrolyte abnormalities [8]. Physical examination findings are often unrevealing, including a patient with thin body habitus, abdominal distention or intestinal obstruction.
Patients with clinical suspicion should undergo further evaluation. Hypotonic duodenography has been described in literature. Findings such as: i) dilatation of the first and second portions of the duodenum, with or without gastric dilatation; (ii) abrupt vertical and oblique compression of the mucosal folds; (iii) antiperistaltic flow of barium proximal to the obstruction; (iv) delay of 4–6 hour in transit through the gastroduodenal region; and (v) relief of obstruction in a prone, knee–chest, or left lateral decubitus position are suggestive [9]. MDCT with three dimensional reconstruction helps to assess the duodenal compression and the aortomesenteric angle and distance more objectively when compared to conventional imaging techniques [10]. In this series the mean aortomesenteric angle was 10.5 degrees in six patients. Upper gastrointestinal endoscopy is useful to rule out other causes of mechanical obstruction. In our series only two patients had duodenal dilatation.
Management of this condition initially involves conservative measures like nasogastric decompression, intravenous rehydration, correction of electrolyte abnormalities and aggressive nutritional support. Nutritional support may be in the form of parenteral nutrition and/or postpyloric feeding when possible, followed by oral diet as tolerated. Medical treatment may be successful in patients with a short history, moderate symptoms and incomplete duodenal obstruction. Left lateral decubitus, knee chest, or prone positioning decreases the mesenteric pressure on the duodenum and allows temporary alleviation of the duodenal obstruction [11]. No definite time limit has been described for conservative management.
The surgical options include duodenojejunostomy, section of the ligament of Treitz and relocation of the duodenojejunal junction, gastrojejunostomy, duodenal anterior replacement. Gastrojejunostomy does not relieve the proximal duodenal obstruction and patients can continue to have postoperative vomiting [12]. Because SMA syndrome is a rare condition, no randomised trials have compared the various surgical techniques. Duodenojejunostomy was introduced by Starley in 1910 and it is has become the most frequent treatment with success rate of 90% [13]. With the advent of laparoscopic era, many of the open procedures could be performed with minimal invasive methods producing similar or better outcome. In 1995, Massoud has described laparoscopic severing of the ligament of Treitz. In 1998 the first laparoscopic duodenojejunostomy was performed by, Gersin KS and Heniford BT [14]. Surgical options should be considered whenever the conservative approach fails or if patient prefers surgical management [15]. A number of case reports and small case series have been published emphasising that laparoscopic duodenojejunostomy is a viable option in the treatment of SMA syndrome, combining the benefits of minimally invasive surgery as well as excellent results [15-17]. Even though it requires expertise, overall the mean duration of hospital stay, requirement of postoperative analgesia and the expenditure are less in the laparoscopic technique while achieving results similar to the open technique. Patient can resume his normal activities at an early date. A list of few similar studies on laparoscopic duodenojejunostomy is provided in [Table/Fig-6] [12,16,18,19].
Studies on laparoscopic treatment of SMA syndrome [16,18,19].
| Author | Type of study | Number of cases | Surgery | Mean Operating time | Mean hospital stay | Outcome |
|---|
| Pottorf BJ et al., [12] | Retros-pective | 12 | Laparo-scopic duodenoj-ejunostomy | 72.4 min | 4.2 days | 92% symptomatic improvement. |
| Munene G et al., [16] | Review | 13 | Laparo-scopic duodeno-jejunostomy | 84 min | 4.5 days | More than 95%symptomaticimprovement |
| Richardson WS et al., [18] | Case series | 2 | Laparo-scopic duodeno-jejunostomy | 113 min | 3 days | Both patients symptom free. |
| Sun Z et al., [19] | Retros-pective | 14 | Lapar-oscopic duodeno-jejunostomy | 119 min | 5.5 days | 79 % symptomatic improvement at 20 months. |
Conclusion
SMA syndrome is an uncommon entity. Many cases are misdiagnosed. Majority of affected patients are young females. A definite precipitating factor can be identified in majority. A high index of clinical suspicion is needed for diagnosis of this condition. Assessment of aortomesenteric angle and aortomesenteric distance by high resolution CECT imaging gives clue to the diagnosis. Management involves conservative measures aimed at improving bodyweight initially. Surgical intervention is reserved for patients who fail on medical management. Laparoscopic duodenojejunostomy is rapidly becoming the standard procedure of this condition producing excellent outcome comparable with open surgery. Majority of patients will be relieved of symptoms after surgical management.
Abbreviations used in this literature
SMA – Superior Mesenteric Artery.
CECT – Contrast Enhanced Computerised Tomogram.
MDCT – Multi Dimensional Computerised Tomogram.
[1]. Von Rokitansky C, Superior mesenteric artery syndromeIn: Lehrbuch der pathologischen Anatomie 1861 3rd edViennaBraumüller:87 [Google Scholar]
[2]. Wilkie DPD, Chronic Duodenal IleusThe American Journal of the Medical Sciences 1927 173(5):643-48. [Google Scholar]
[3]. Shiu JR, Chao HC, Luo CC, Lai MW, Kong MS, Chen SY, Clinical and nutritional outcomes in children with idiopathic superior mesenteric artery syndromeJ Pediatr Gastroenterol Nutr 2010 51(2):177-82. [Google Scholar]
[4]. Merrett ND, Wilson RB, Cosman P, Biankin AV, Superior mesenteric artery syndrome: diagnosis and treatment strategiesJournal of Gastrointestinal Surgery 2008 13(2):287-92. [Google Scholar]
[5]. Kyslan K, Barla J, Stanislayova M, Superior mesenteric artery (SMAS/AMS) syndrome and its managementRozhl Chir 2008 87(5):255-58. [Google Scholar]
[6]. Zaraket V, Deeb L, Wilkies Syndrome or Superior Mesenteric Artery Syndrome: Fact or FantasyCase Reports in Gastroenterology 2015 9(2):194-99. [Google Scholar]
[7]. Smith BM, Zyromski NJ, Purtill M-A, Superior mesenteric artery syndrome: an underrecognized entity in the trauma populationThe Journal of Trauma: Injury, Infection, and Critical Care 2007 PAP:827-30. [Google Scholar]
[8]. Cohen LB, Field SP, Sachar DB, The superior mesenteric artery syndrome. The disease that isnt, or is itJournal of Clinical Gastroenterology 1985 7(2):113-16. [Google Scholar]
[9]. Yakan S, Calıskan C, Kaplan H, Deneclı AG, Coker A, superior mesenteric artery syndrome: a rare cause of intestinal obstruction. Diagnosis and Surgical ManagementIndian J Surg 2013 75(2):106-10. [Google Scholar]
[10]. Agrawal GA, Johnson PT, Fishman EK, Multidetector row CT of superior mesenteric artery syndromeJournal of Clinical Gastroenterology 2007 41(1):62-65. [Google Scholar]
[11]. Welsch T, Büchler MW, Kienle P, Recalling superior mesenteric artery syndromeDigestive surgery 2007 24(3):149-56. [Google Scholar]
[12]. Pottorf BJ, Husain FA, Hollis HW. Jr, Lin E, Laparoscopic management of duodenal obstruction resulting from superior mesenteric artery syndromeJAMA Surg 2014 149(12):1319-22. [Google Scholar]
[13]. Ha CD, Alvear DT, Leber DC, Duodenal derotation as an effective treatment of superior mesenteric artery syndrome: a thirty-three year experienceThe American Surgeon 2008 74(7):644-53. [Google Scholar]
[14]. Gersin KS, Heniford BT, Laparoscopic duodenojejunostomy for treatment of superior mesenteric artery syndromeJSLS 1998 2:281-84. [Google Scholar]
[15]. Bohanon FJ, Lopez ON, Graham BM, Griffin LW, Radhakrishnan RS, A case series of laparoscopic duodenojejunostomy for the treatment of pediatric superior mesenteric artery syndromeInternational Journal of Surgery and Research 2016 2016(Suppl 1):1 [Google Scholar]
[16]. Munene G, Knab M, Parag B, Laparoscopic duodenojejunostomy for superior mesenteric artery syndromeAm Surg 2010 76(3):321-24. [Google Scholar]
[17]. Wyten R, Kelty CJ, Falk GL, Laparoscopic duodenojejunostomy for the treatment of superior mesenteric artery (SMA) Syndrome: case seriesJ Laparoendosc Adv Surg Tech A 2010 20(2):173-76. [Google Scholar]
[18]. Richardson WS, Surowiec WJ, Laparoscopic repair of superior mesenteric artery syndromeAm J Surg 2001 181(4):377-78. [Google Scholar]
[19]. Sun Z, Rodriguez J, McMichael J, Walsh RM, Chalikonda S, Rosenthal RJ, Minimally invasive duodenojejunostomy for superior mesenteric artery syndrome: a case series and review of the literatureSurg Endosc 2015 29(5):1137-44. [Google Scholar]