Gastroduodenal Intussusception due to Gastrointestinal Stromal Tumour (GIST)
Abdul Rehman Abdul Jameel1, Durairaj Segamalai2, Gnanasekaran Murugaiyan3, Rajendran Shanmugasundaram4, Naganath Babu Obla5
1 Postgraduate, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
2 Postgraduate, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
3 Assistant Professor, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
4 Professor, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
5 Director and Professor, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Naganath Babu Obla, WD-243, Tower 2, Rajiv Gandhi Government General Hospital, Madras Medical College, Chennai-600003, Tamil Nadu, India.
E-mail: naganathbabu@gmail.com
Gastroduodenal intussusception is the rarest forms of adult intussusception. We present a case of gastroduodenal intussusception due to a gastric Gastrointestinal Stromal Tumour (GIST). The patient was a 65-year-old female who clinically presented as acute gastric outlet obstruction. The patient was managed by gentle reduction of the intussusception, followed by wedge resection of the tumour. She was relieved of her symptoms and recurrence free for past one year.
Adult intussusception, Endoscopy, Gastric outlet obstruction, Gastric tumour
Case Report
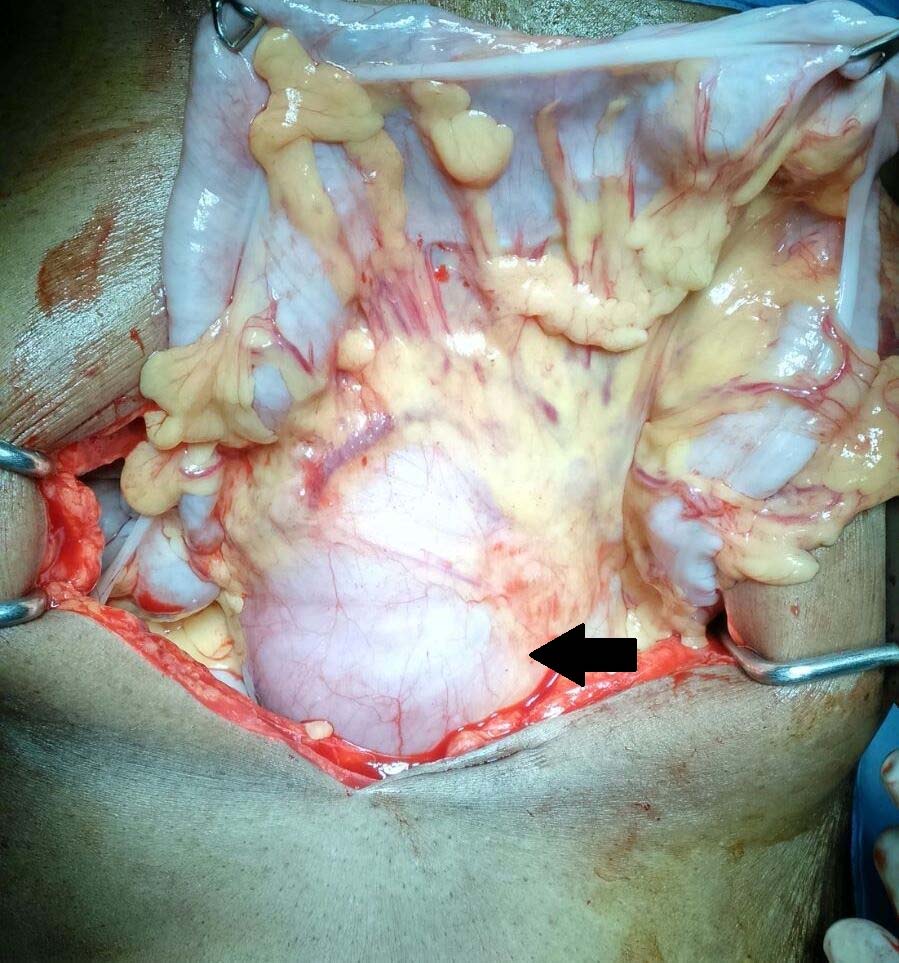
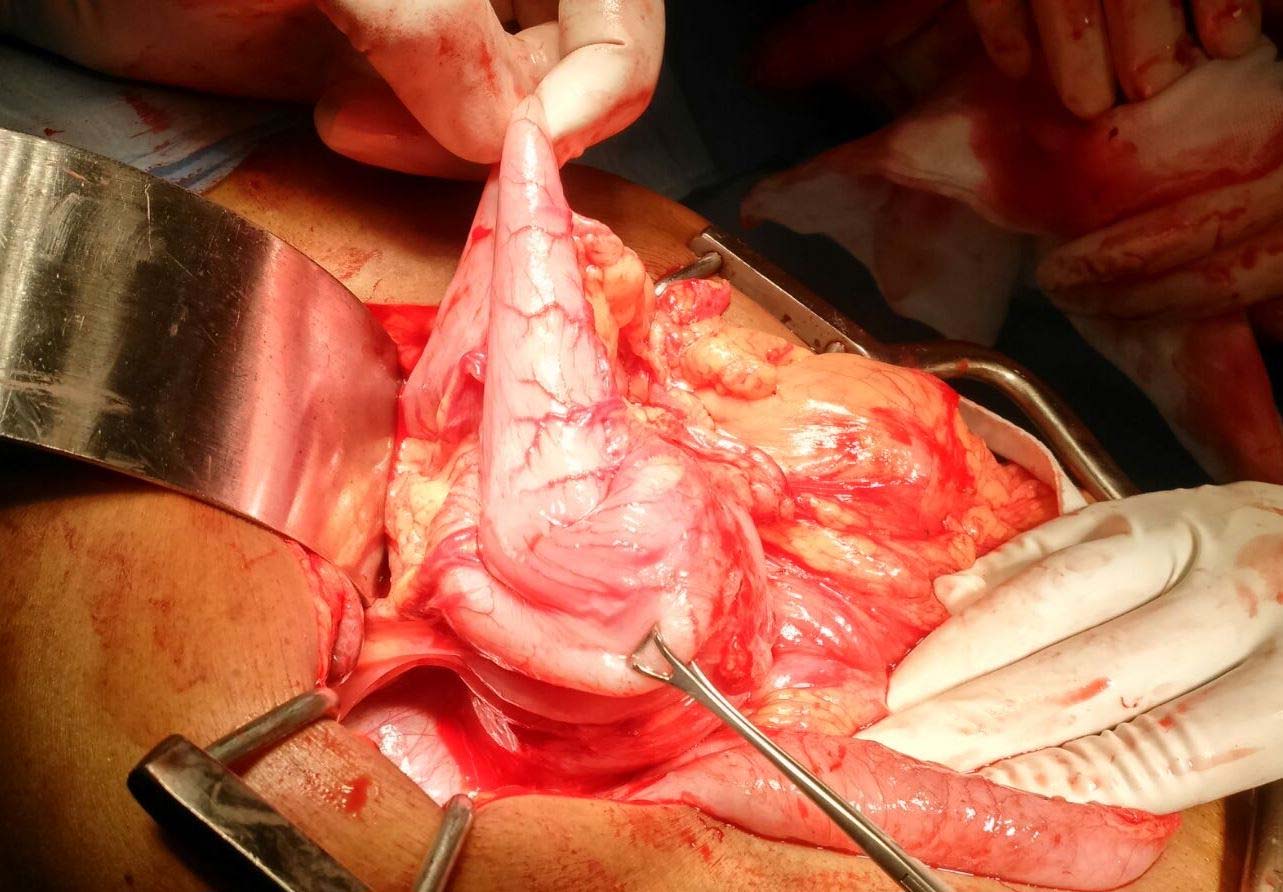
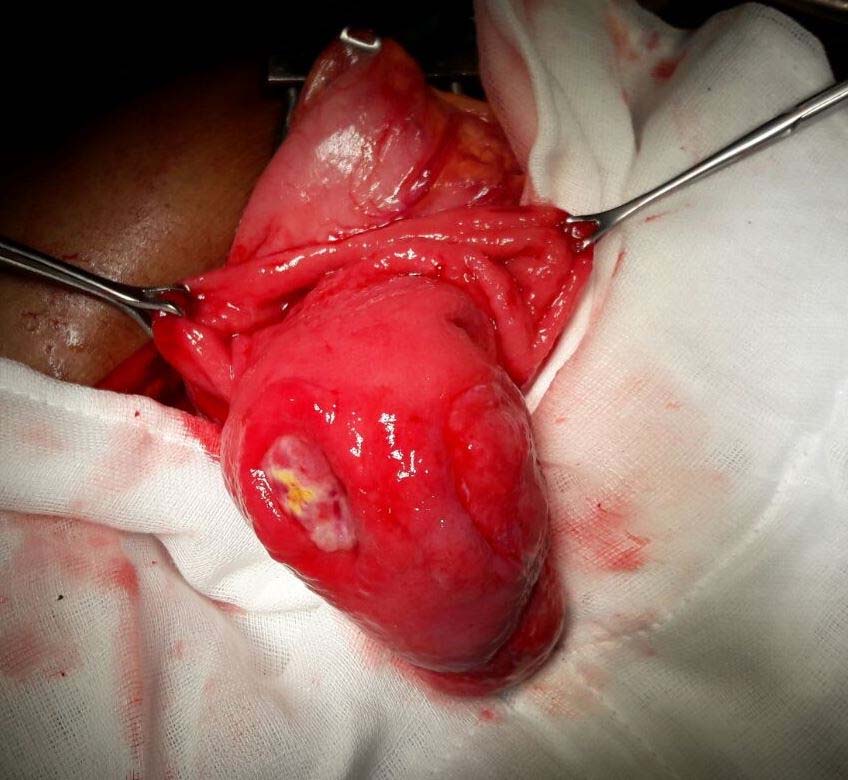
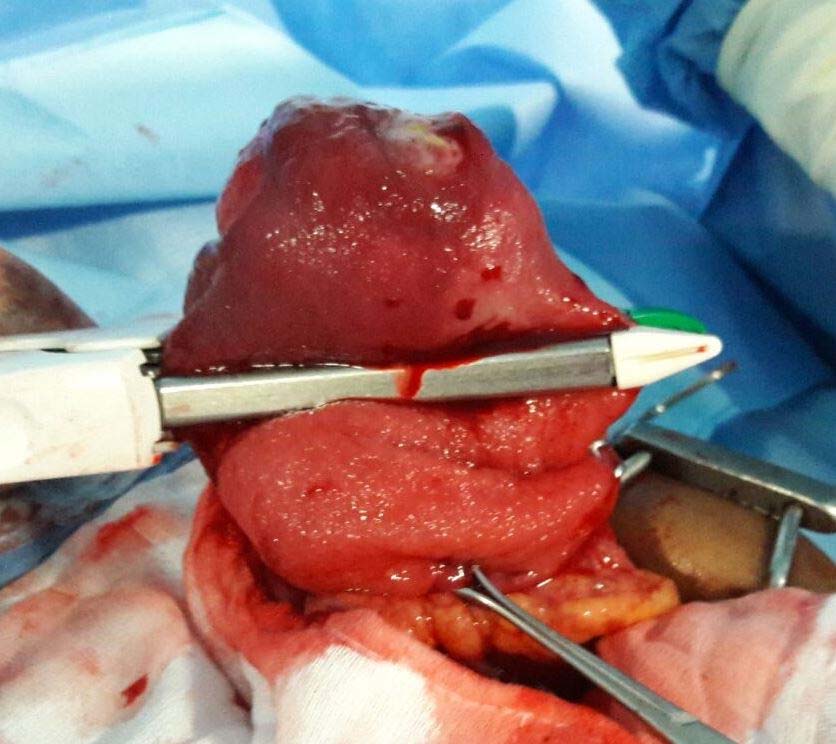
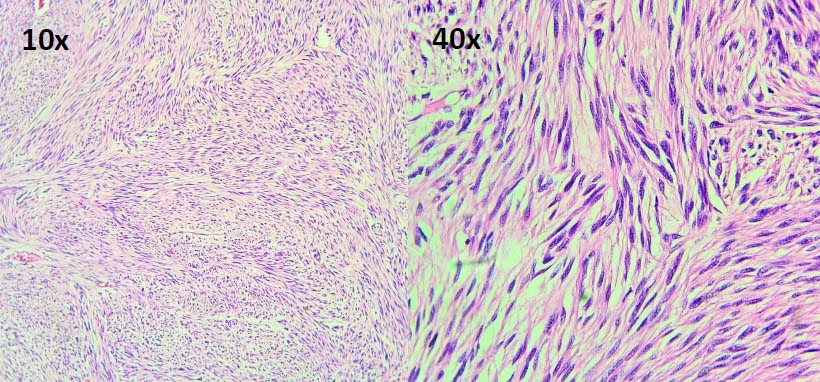
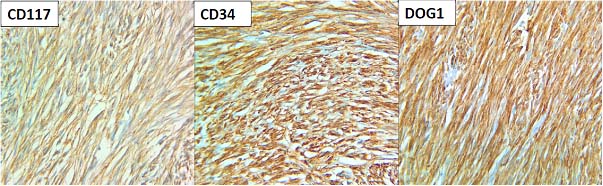
A 65-year-old female presented with symptoms of upper abdominal pain, intermittent vomiting 30 minutes after meals for the past six months and she did not have any significant past history. She had a mass, palpable in the right upper quadrant with clinical features of gastric outlet obstruction. Blood investigations showed mild anaemia. Endoscopy showed a submucosal tumour from the posterior wall of stomach with central ulceration prolapsing into the duodenum [Table/Fig-1]. CT scan demonstrated gastroduodenal intussusception due to 6 x 6 x 4 cm sized heterogeneously enhancing pedunculated polypoid mass attached to the antropyloric region, lying within the duodenum extending till its third part [Table/Fig-2,3]. During laparotomy, the gastroduodenal intussusception was noticed to have extended upto the duodeno-jejunal junction as evidenced by the intussusception complex being seen in the infracolic compartment [Table/Fig-4]. The intussusception was reduced gradually with traction [Table/Fig-5] and the tumour replaced back into the antrum. Anterior gastrotomy was made, the tumour was resected with a cuff of posterior wall of stomach with GIA stapler [Table/Fig-6,7]. The anterior gastrotomy was closed with single layer continuous 2’0 vicryl sutures. Postoperative period was uneventful, Nasogastric tube was removed on second Post Operative Day (POD) and orals gradually started from third POD and discharged on eighth POD. Histopathology of the resected specimen showed spindle cell neoplasm with 0-1/50 (high-power field) mitotic activity [Table/Fig-8]. There was focal ulceration of mucosa and no necrosis was evident. All around gastric wall margin was free of tumour. Immunohistochemistry showed positivity for CD 117, CD 34 and DOG1 [Table/Fig-9]. Smooth Muscle Actin (SMA) was focally positive with S100 negative. The patient is doing well, without recurrence for the past one year.
Endoscopy showing submucosal tumour in the antrum with mucosal ulceration.

CT scan showing gastroduodenal intussusception (white arrow head).

CT scan showing gastroduodenal intussusception extending to third part of duodenum (white arrow head).

Gastroduodenal intussusception complex seen at duodenojejunal junction in the infracolic compartment.
Reduction of the intussusception by gentle traction.
After anterior gastrotomy, tumour seen arising from the posterior wall of stomach.
Wedge resection of the tumour done with GIA staplers.
H and E section showing spindle cell neoplasm. (10X and 40X).
Immunohistochemistry staining showing positivity for CD117, CD34 and DOG1.
Discussion
Adult intussusception is different in its entity than in children as it is caused by a definable structural lesion [1]. Gastroduodenal intussusception is among the rarest forms of adult intussusception, around 10% [2]. Gastroduodenal intussusception results from the invagination of a part of the stomach through the pylorus and into the duodenum. It can be caused by benign or malignant conditions. This rare presentation has been documented to be caused by polyps, Menetrier’s disease, brunner gland hamartoma, GIST and gastric carcinoma [3-7]. Our case of gastroduodenal intussusception is due to a pedunculated gastric GIST.
GIST is the most common mesenchymal tumours of the gastrointestinal tract, and is pathologically defined by positive immunostaining for c-kit proto-oncogene - CD117 (overexpressed in 95%) and CD34 (positive in 60% to 70%) [8]. Gastrointestinal stromal tumours are relatively common tumour of the stomach, majority of which are asymptomatic. Ulceration of the apical mucosa may occur resulting in abdominal pain or bleeding as reported in 50% of cases [9]. Rarely patients present with symptoms of weight loss, early satiety, dysphagia and vomiting. Our patient presented with similar symptoms along with acute gastric outlet obstruction due to gastroduodenal intussusception. Only a handful of cases of gastroduodenal intussusception due to a gastric GIST have been reported in literature so far [6,10-12]. Endoscopy and CT scan are helpful in making a diagnosis, as in our case.
The treatment of choice for localised GIST is complete surgical resection. Gastric GIST <5 cm can be managed by wedge resection of stomach with generous margin, although some may require formal types of gastrectomy [13]. Tumours located close to gastroesophageal junction or pylorus may not be amenable to straight forward wedge resections. Laparoscopic management of gastric GIST has been reported in centres with such expertise [11,12].
Tumour size and mitotic index are the main variables used in risk stratification systems, which was first developed by the National Institute of Health (NIH), also called as Fletcher’s criteria [14]. Modified NIH criteria include additional prognostic factors, such as non-radical resection (R1) and tumour rupture [15]. Based on Fletcher’s criteria our case belonged to the low risk category.
Conclusion
Gastroduodenal intussusception is the rarest form of adult intussusception. It can be caused by benign or malignant gastric tumours. Although gastric GIST is not uncommon, presentation in the form of gastroduodenal intussusception is very rare. This diagnosis should be entertained in a patient with acute gastric outlet obstruction. After reduction of the intussusception, GIST requires conventional surgical resection.
[1]. Choi S, Han J, Kim S, Lee J, Lee K, Kim Y, Intussusception in adults: from stomach to rectumAmerican Journal of Roentgenology 2004 183(3):691-98. [Google Scholar]
[2]. Stubenbord W, Thorbjarnarson B, Intussusception in AdultsAnnals of Surgery 1970 172(2):306-10. [Google Scholar]
[3]. Kim DJ, Lee JH, Kim W, Gastroduodenal Intussusception Resulting from Large Hyperplastic PolypJournal of Gastric Cancer 2012 12(3):201-04. [Google Scholar]
[4]. Juglard R, Rimbot A, Stéphant E, Paoletti H, Talarmin B, Arteaga C, Gastroduodenal intussusception complicating Menetrier’s diseaseJ Radiol 2006 87:69-71. [Google Scholar]
[5]. Petersen JM, Felger TS, Goldstein JD, Gastroduodenal intussusception secondary to a giant brunner gland hamartomaGastroenterol Hepatol (N Y) 2008 4:471-73. [Google Scholar]
[6]. Gyedu A, Reich SB, Hoyte-Williams PE, Gastrointestinal stromal tumour presenting acutely as gastroduodenal intussusceptionActa Chir Belg 2011 111:327-28. [Google Scholar]
[7]. Asai S, Kijima H, Yamamoto S, Shiraishi S, Suzuki T, Maeda Y, Gastroduodenal intussusception secondary to pedunculated gastric carcinomaJ Ultrasound Med 2008 27:673-76. [Google Scholar]
[8]. Bucher P, Villiger P, Egger JF, Buhler LH, Morel P, Management of gastrointestinal stromal tumours: from diagnosis to treatmentSwiss Med Wkly 2004 134:145-53. [Google Scholar]
[9]. Nakagawara M, Kajimura M, Hanai H, Shimizu S, Kobayashi H, Gastroduodenal intussusception secondary to a giant solitary gastric heterotopia: A case reportGastrointestinal Endoscopy 2000 52(4):568-70. [Google Scholar]
[10]. PBB M.S., Reddy CK, Augustine AJ, Sagari SG, Gastroduodenal Intussusception Due to Pedunculated Polypoid Gastrointestinal Stromal Tumour (Gist): A Rare CaseJournal of Clinical and Diagnostic Research: JCDR 2015 9(1):PD05-PD06. [Google Scholar]
[11]. Palanivelu C, Rangarajan M, Annapoorni S, Laparoscopic distal gastrectomy for gastroduodenal intussusception due to a benign gastric tumourHellenic Journal of Surgery 2016 88(2):135-38. [Google Scholar]
[12]. Adjepong S, Parameswaran R, Perry A, Mathews R, Jones R, Butterworth J, Gastroduodenal Intussusception due to Gastrointestinal Stromal Tumour (GIST) treated by laparoscopic billroth II distal gastrectomySurgical Laparoscopy, Endoscopy & Percutaneous Techniques 2006 16(4):245-47. [Google Scholar]
[13]. Pidhorecky I, Cheney R, Kraybill W, Gibbs J, Gastrointestinal Stromal Tumours: Current Diagnosis, Biologic Behavior, and ManagementAnnals of Surgical Oncology 2000 7(9):705-12. [Google Scholar]
[14]. Demetri GD, Von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumoursJournal of the National Comprehensive Cancer Network 2010 8(Suppl 2):S-1. [Google Scholar]
[15]. Agaimy A, Gastrointestinal stromal tumors (GIST) from risk stratification systems to the new TNM proposal: more questions than answers? A review emphasizing the need for a standardized GIST reportingInternational Journal of Clinical and Experimental Pathology 2010 3(5):461-471. [Google Scholar]