Some techniques have been recommended to prevent and decrease the complications of nasotracheal intubation, including heating the nasotracheal tube, lubricating the distal one-third of the tube and the nasal mucosa before intubation, local use of vasoconstrictors and local anaesthetic agents (phenylephrine and lidocaine) and use of intranasal antibiotic ointments, etc., [8,9].
In addition, several studies have shown that prophylactic use of mupirocin ointment within the nasal cavity in S. aureus carriers decreases the risk of infection of the surgical site, alleviate problems in ICU patients, who undergo intubation for a long duration [3,4,10-12]. However, except for the study by Takahashi S et al., no comprehensive study has been carried out to evaluate the efficacy of this ointment. In that study, only the antibacterial properties of mupirocin were evaluated and other complications of nasotracheal intubation were not evaluated [2]. However, it is expected that use of this ointment will be useful for decreasing other complications of nasotracheal inhibition, in addition to its antibacterial effect, because it has a lubricating effect, too. Therefore, the present study was designed to evaluate the effect of nasal mupirocin ointment before and after nasotracheal intubation on decreasing the complications of intubation during oral and maxillofacial surgeries. Thus, in case of favourable effects this ointment can be used in all the surgeries that are associated with nasal intubation to decrease the complications of the procedure, especially in compromised patients. It should be pointed out that no studies to date have reported any major side effects associated with the use of mupirocin ointment and the complications have been confined to minor irritation of the nasal mucosa that is resolved after discontinuation of the use of the ointment [4,10].
Materials and Methods
This single blinded randomized controlled trial was carried out from April 2016 to February 2017 at Imam Reza Educational/Treatment Center, Tabriz, Iran. Based on a study by Takahashi S et al., and by considering α=0.05, β=0.2, power=80%, P1=0.66 and P2=0.23 and a difference of 10%, the sample size was estimated at 44 [2].
At the beginning of the study, an informed consent form was prepared and explained to all the patients so that those who were unable to read or write became aware of it.
The inclusion criteria consisted of subjects of age between 20 to 60 years in the ASA1 category (American Society of Anaesthesiologist’s physical status) [13] undergoing nasotracheal intubation; who signed informed consent were included in the study. The exclusion criteria consisted of a history of difficult intubation, clinical signs and symptoms associated with difficult intubation, contraindications for nasotracheal intubation, frequent epistaxis, nasal polyps, chronic sinusitis, use of anti-inflammatory medications (especially Aspirin in recent weeks), upper respiratory tract infections, active allergic reactions, nasal occlusion (septal deviation, enlarged pharyngeal adenoid, enlarged palatine tonsils), allergy to mupirocin, nasal fracture and haemorrhagic traumas of the nose, retropharyngeal or postnasal haemorrhage before surgery, pregnancy, breastfeeding and patients with more than two times of attempts for nasal intubation.
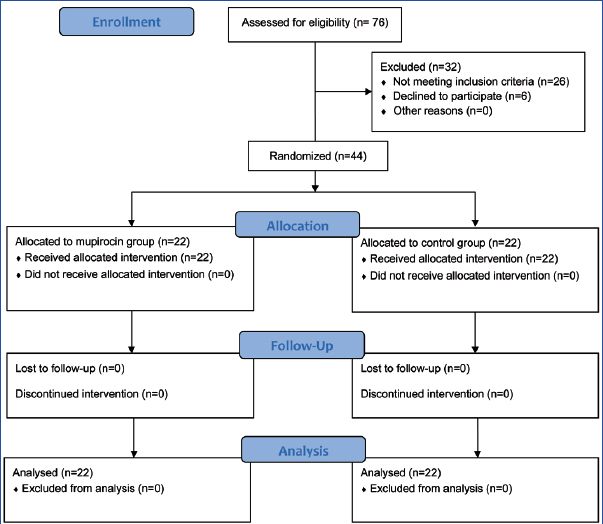
A purposive sampling technique was used for randomization of subjects. The subjects were randomly assigned to two equal groups (n=22) by one operator blinded to the aims of the study, using the Randlist software program, and the two groups were matched in terms of age and gender. Group 1 was the test group on which effects of 2% mupirocin were assessed whereas, in group 2 no intervention was carried out. Before the study, all the subjects were briefed on the study procedures and steps and the scoring technique was explained to them. All the subjects completed the study and none was excluded [Table/Fig-1].
Flow diagram of study patients.
Clinical examinations were carried out by an oral and maxillofacial surgeon and for pulmonary health, by an anaesthesiologist. Based on the clinical symptoms and signs including easy respiration from both nostrils; the deviation of nasal septum was evaluated with the use of a nasal speculum.
Study Groups
A sterile swab was used, eight to 10 hours before nasotracheal intubation, to take a sample for culturing from the vestibule of nostrils and the anterior septum of the patients. In Group 1, 2% nasal mupirocin ointment (Mupirocin 2%, Sina Daru Co., Tehran, Iran) was applied to the vestibules of both nostrils and the anterior septum. In Group 2, no intervention was carried out.
The patients were transferred into the operating room and underwent premedication; three to five minutes before induction, three drops of 0.25% phenylephrine (Nasophrin 0.25%, Sina Daru Co., Tehran, Iran) were applied into each nostril and the patients carried out a deep and rapid inspiration so that the phenylephrine drops covered the whole nasal mucosa like a spray. Induction was carried out and each patient underwent general anaesthesia. The nasotracheal tube, measuring 6-6.5 mm in internal diameter, was placed in water (60°C) for three minutes for softening to prevent mucosal trauma [8]. Before intubation, the nostril used for intubation was covered with 2% lidocaine gel (Xylogel 2%, Sina Daru Co., Tehran, Iran). In addition, the distal tip of the nasotracheal tube and its cuff were lubricated with 2% lidocaine gel. Intubation was carried out under clean conditions. The nasotracheal tube, with a suitable size, was inserted into the nostril and guided towards the pharynx with mild pressure. When the tip of the tube entered the pharynx, there was a sudden decrease in the pressure of the nasotracheal tube, upon which in Group 1 the part of the tube which was outside of the nostril was lubricated with 2% mupirocin ointment. In addition, inside of the nostrils were also lubricated with 2% mupirocin ointment. Then, a laryngoscope was used to place the distal end of the tube within the trachea under direct visualization. It should be noted that the segment of the tube which had been lubricated with mupirocin ointment was never placed within the larynx and the trachea, and was only placed in the nasopharynx. Therefore, the effect of the ointment was evaluated only in the nasal area. After surgery and before extubation, four to five drops of 0.25% phenylephrine drops were applied to the periphery of the tube. Each patient was extubated after three to four minutes. The distal end of the tube, measuring 4 mm in length, was transferred to the Microbiology Laboratory for microbial culturing and antibiogram test for the presence of S. aureus and other bacterial species [8].
The prepared samples were stored in broth and sent to the laboratory using the Amies transport medium. The initial culturing was carried out on MacConkey blood agar and chocolate agar media. Then conventional biochemical methods and Microgen identification kit (Microgen GN-A and GN-B, Gamberley, United Kingdom) were used for identification of microbial species. In addition, Muller-Hinton agar medium (Merck, Germany) was used for antibiogram test and for evaluation of resistance in microbial isolates, Kirby Bauer disc diffusion test was employed using 8 MAST antibiotic discs (MAST Diagnosis group, United Kingdom) [14]. The microbial suspensions were used at 0.5 McFarland standards and the evaluations were carried out using CLSI (Clinical Laboratory Standard Institute) guidelines [14].
In addition, the patients were compared in relation to the severity of nose bleeding during intubation and after extubation in the two groups. The severity of nose bleeding during intubation was scored as follows by an anaesthesiologist:
No bleeding;
Mild bleeding with some blood visible on the tracheal tube with the use of a laryngoscope; however, no bleeding upon suction from the oropharynx;
Moderate bleeding with some blood being suctioned from the oropharynx, which stops after some irrigation;
Severe bleeding, with profuse blood suctioned from the oropharynx, which does not stop after irrigation and epistaxis is observed, too.
The severity of nose bleeding after extubation was scored by the anaesthesiologist as follows:
No blood on the distal end of the tube (no bleeding);
Some blood on the distal end of the tube (mild bleeding);
Blood on the distal end of the tube + suction of blood from the nasopharynx or oropharynx (moderate bleeding);
Apart from the case 3 above, epistaxis is observed (severe bleeding).
In addition, the ease of extubation in the two study groups was scored by the anaesthesiologist as follows:
Easy (extubation without the application of any force);
Moderate (extubation with the application of force with no trauma);
Difficult (extubation with the application of force in association with trauma).
The ease of breathing through the nose and the severity of nasal congestion in the study groups were scored at three, six and 12 hour intervals after extubation by the oral and maxillofacial surgeon as follows:
Easy breathing without nasal congestion.
Mild difficulty in breathing (with nasal congestion).
Difficult breathing (severe nasal congestion), necessitating prescription of phenylephrine drops.
A microbiologist blinded to the objectives of the study and patient’s group allocations carried out all the microbial culture procedures. The operator carrying out data analysis, too, was blinded to the patient’s group allocations. Clinical examinations in relation to the complications of nasal intubation consisted of nasal bleeding during intubation and after intubation and ease of intubation by an anaesthesiologist. However, it was not possible to blind the anaesthesiologist because mupirocin was used in one group during intubation and not used in the other group. Clinical examination in relation to the ease of breathing was carried out by an oral and maxillofacial surgeon who was not aware of the objectives and patient grouping. However, since no placebo was used, it was not possible to blind the patients.
In the present study, all the patients went through the routine procedures of diagnosis and treatment planning and none of the patients was deprived of the routine treatment. The protocol of the study was approved by the Ethical Committee of Tabriz University of Medical Sciences under the code IR.TBZMED.REC.1394.20.
Statistical Analysis
Data were analysed with descriptive statistical methods (means, standard deviations, frequencies and percentages), repeated-measures ANOVA, Fisher’s-exact test and Chi-square test, using SPSS 18. Statistical significance was set at p-value<0.05.
Results
In the present study, 44 patients who were candidates for surgery under nasal intubation, with a mean age of 32.5±12.8 years, were evaluated. All the subjects completed the study and none was excluded from the study [Table/Fig-1].
The results of microbial cultures from the nasal mucosa and the distal end of the nasotracheal tube in each study group are represented in [Table/Fig-2].
The frequencies (percentages) of microorganisms that were cultured, separately in each study group.
| Result of culture | Mupirocin group | Fisher’s-exact test | Control group | Fisher’s-exact test |
|---|
| Nasal Cavity (Before intubation) | Intubation tube (After extubation) | p-value | nasal Cavity (Before intubation) | intubation tube (after extubation) | p-value |
|---|
| S. epidermidis | 15 subjects (68.1%) | 3 subjects (13.6%) | 0.05* | 18 subjects (81.8%) | 18 subjects (81.8%) | 1.0 |
| S. aureus | 6 subjects (27.2%) | 0 | 0.02* | 4 subjects (18.2%) | 4 subjects (18.2%) | 1.0 |
| Other Coagulase negative staphylococci | 1 subject (4.5%) | 0 | 1.0 | 0 | 0 | - |
| Yeast | 3 subjects (13.6%) | 0 | 0.2 | 1 subject (4.5%) | 1 subject (4.5%) | 1.0 |
| K. pneumoniae | 0 | 3 subjects (13.6%) | 0.2 | 0 | 0 | - |
| P. aeruginosa | 0 | 3 subjects (13.6%) | 0.2 | 0 | 9 subjects (40.9%) | 0.001* |
| E. agglomerans | 0 | 0 | - | 0 | 1 subject (4.5%) | 1.0 |
| C. freundii | 0 | 0 | - | 0 | 1 subject (4.5%) | 1.0 |
| K. oxytoca | 0 | 0 | - | 0 | 1 subject (4.5%) | 1.0 |
| Culture negative | 0 | 13 subjects (59.1%) | 0.001* | 0 | 0 | - |
Statistically significant (p-value<0.05).
Before surgery, a total of 27.2% (6) of the subjects in the mupirocin group were carriers of S. aureus in the nasal cavity and 50% of isolated S. aureus were resistant to methicillin.
After extubation, no S. aureus was detected at the distal end of nasotracheal tube (p-value=0.02); however, in 27.2% of these patients (six subjects) there was colonization of Gram-negative bacteria, in 13.6% (three subjects) of which P. aeruginosa was detected at the end of the distal end of nasotracheal tube.
A total of 18.2% (4) of the patients in the control group were carriers of S. aureus in the nasal cavity before surgery, but there was no change in the number of S. aureus counts at the distal end of nasotracheal tube, 50% of which were resistant to methicillin. These patients were exactly those from whom Methicillin-Resistant S. aureus (MRSA) had been isolated from their nasal cavity (p-value=1). An interesting finding was the fact been 54.4% (12) of the subjects in the control group exhibited colonization of different Gram-negative bacteria and the results of microbial culture tests showed that there were P. aeruginosa in 40.9% (9) of the cases and only one case was resistant to carbapenem.
In the mupirocin group, no microorganisms were cultured from the distal end of the nasotracheal tube in 59.1% of the cases (13 subjects); however, in the control group there were no cases of negative culture results (p-value=0.001).
[Table/Fig-3] represents the results of the severity of haemorrhage from the nose during intubation and after extubation.
The frequencies (percentages) of the severity of haemorrhage from the nose during intubation and after extubation in the study groups.
| Severity of bleeding | During intubation | after extubation |
|---|
| Mupirocin group | Control group | Mupirocin group | Control group |
|---|
| No bleeding | 20 subjects (90.9%) | 19 subjects (86.4%) | 14 subjects (63.6%) | 2 subjects (9.1%) |
| Mild bleeding | 2 subjects (9.1%) | 3 subjects (13.6%) | 3 subjects (13.6%) | 13 subjects (59.1%) |
| Moderate bleeding | 0 | 0 | 1 subject (4.5%) | 2 subjects (9.1%) |
| Severe bleeding | 0 | 0 | 4 subjects (18.2%) | 5 subjects (22.7%) |
| Chi-Square Test | p-value=0.5 | p-value=0.001* |
Statistically significant (p-value<0.05)
The results showed that the frequencies of haemorrhage during nasal intubation in the mupirocin and control groups were 9.1% and 13.6%, respectively. However, there was no significant difference between the two groups (p-value=0.5). The results after extubation showed that the differences in the severity of haemorrhage between the two groups were significant, with higher frequencies in the control group (p-value=0.001).
[Table/Fig-4] represents the results of the ease of extubation in the two study groups. The results showed that the difference between the two groups was significant, with a higher rate of easy extubation in the mupirocin group (p-value=0.044).
The frequencies (percentages) of ease of extubation in the study groups.
| Ease of extubation | Mupirocin group | Control group |
|---|
| Easy | 19 subjects (86.4%) | 13 subjects (59.1%) |
| Moderate | 3 subjects (13.6%) | 9 subjects (40.9%) |
| Difficult | 0 | 0 |
| Chi-Square Test | p-value=0.044* |
Statistically significant (p-value<0.05)
In relation to the ease of breathing after surgery, in the mupirocin and control groups 9.1% and 63.7% of the patients, respectively, reported mild difficulty in breathing after extubation. Three hours after extubation, these percentages were 9.1% and 54.6%, respectively. Chi-square test showed that immediately after gaining consciousness (p-value=0.001) and three hours after extubation (p-value=0.001) the rate of easy breathing was significantly higher in the mupirocin group. In contrast, at six and 12 hour intervals after extubation the results were similar in both groups, with no significant differences (p-value=0.75) [Table/Fig-5].
The frequencies (percentages) of ease of breathing in the study groups at different postoperative intervals.
| Ease of breathing | Immediately after regaining consciousness | After 3 hours | After 6 hours | After 12 hours |
|---|
| Mupirocin | Control | Mupirocin | Control | Mupirocin | Control | Mupirocin | Control |
|---|
| Easy breathing | 20 subjects (90.9%) | 8 subjects (36.3%) | 20 subjects (90.9%) | 10 subjects (45.4%) | 21 subjects (95.4%) | 21 subjects (95.4%) | 21 subjects (95.4%) | 21 subjects (95.4%) |
| Rather difficult breathing | 2 subjects (9.1%) | 14 subjects (63.7%) | 2 subjects (9.1%) | 12 subjects (54.6%) | 1 subject (4.6%) | 1 subject (4.6%) | 1 subject (4.6%) | 1 subject (4.6%) |
| Difficult breathing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Chi-Square Test | p-value=0.001* | p-value=0.001* | p-value=0.75 | p-value=0.75 |
Statistically significant (p-value<0.05)
Discussion
In the present study, 44 patients who were candidates for surgery under nasal intubation were evaluated.
The most prevalent bacteria cultured from the anterior vestibule of the nose of patients before intubation were S. epidermidis (75%) and S. aureus (22%). S. aureus nasal carriage rate were reported 23% to 38% in recent studies [15,16]. In the present study, nasal carriage rate of MRSA was 11.36%, similar to which reported in Takahashi S et al., (11.6%) study [2].
Although P. aeruginosa bacterial species was not cultured from the nasal cavity of any of the patients before intubation, it was cultured from the distal end of the nasotracheal tube in both groups after extubation; but, the amount of bacteria cultured in the control group (40.9%) was three folds that in the mupirocin group (13.6%). In fact, use of mupirocin not only resulted in a decrease in the risk of colonization of S. aureus, even the cases resistant to methicillin, but also it decreases the risk of colonization of Gram-negative bacteria.
The number of S. epidermidis bacterial species (68.1%) cultured from the distal end of the nasotracheal tube in patients receiving mupirocin decreased approximately 50% compared to the bacterial culture results (13.6%) from the nasal cavity before intubation and the counts of S. aureus bacterial species (27.2%) decreased to zero. In the control group, the same amount of bacteria cultured before intubation from the nasal vestibule was cultured from the distal end of the nasotracheal tube after extubation (18.2%). In a similar study by Takahashi S et al., a total of 46.1% and 7.7% of the patients in the mupirocin group were carriers of general bacteria and MRSA in the nasal cavity before surgery. After nasal intubation, general bacteria were isolated from the nasotracheal tube tip in 23.1% of the patients in the mupirocin group, and no MRSA was detected. A total of 66.7% and 16.7% of the patients in the control group were carriers of general bacteria and MRSA in the nasal cavity before surgery, but there was no change in the number of general bacteria and MRSA counts at the distal end of nasotracheal tube after surgery. They concluded that nasotracheal intubation, compared to orotracheal intubation, resulted in the transportation of more bacteria into the trachea and use of nasal mupirocin ointment before surgery might decrease the number of bacteria transported [2].
In 2008, van Rijen MM et al., carried out a review and meta-analysis, in which 686 patients who were candidates for surgery and were carriers of S. aureus in the nasal area, were evaluated. They concluded that contamination with S. aureus in the control subjects was twice that in patients receiving mupirocin [3].
Bode LG et al., evaluated 808 patients who were undergoing surgery in 2010 and showed that contamination with S. aureus in patients receiving mupirocin was approximately 3.4%, with 7.7% in the control group. They concluded that prophylactic use of mupirocin ointment within the nose in carriers of S. aureus resulted in a decrease in staphylococcal infections after surgery [4].
Hill RL et al., used nasal mupirocin ointment to eliminate methicillin-resistant S. aureus from the nasal cavities of hospital employees and patients and showed that use of mupirocin resulted in the management of the incidence of infection [11].
In rhinosinusitis cases resistant to surgical treatment, use of mupirocin sinonasal irritants has been reported as a short-term anti-staphylococcal treatment [12].
In some studies, local anaesthetic agents and vasoconstrictors have been used for disinfecting the nasal cavity and decreasing the complications of nasal intubation. However, subsequent evaluations showed that use of these agents does not have significant effects on preventing bacteraemia and decreasing bacterial counts in the nasal cavity [2].
Therefore, it might be concluded that nasotracheal intubation results in the transportation of microorganisms into the trachea and use of mupirocin before intubation results in a decrease in the bacterial counts in the nasal area, decreasing the bacterial counts in the distal end of the nasotracheal tube and decreasing transportation of bacteria into the trachea, consistent with the results of other studies [4,11,12].
In relation to the comparison of the complications of nasal intubation in the study groups, the results showed that the severity of bleeding during intubation was similar in both groups. However, in the mupirocin group, bleeding in the nose region was less severe after extubation and extubation was easier. Breathing was easier in patients in the mupirocin group immediately after regaining consciousness and three hours after extubation; however, six and 12 hours after extubation it was the same in both groups. Use of mupirocin during nasal intubation and its lubricating effect might result in a decrease in trauma to the nasal region, decrease in the severity of bleeding, increase in the ease of extubation and finally easy breathing of the patients.
Recent investigations reported that nasotracheal intubation is associated with some complications, including trauma to mucous membranes of the nasal passages, epistaxis and postoperative nasal congestion [2,5-7]; which is in agreement with the results of the present study. So, in addition to some techniques that has been suggested to prevent and decrease the complications of nasotracheal intubation, including heating the nasotracheal tube, lubrication of the distal third of the tube, etc., [8,9]; the use of mupirocin ointment before nasotracheal intubation can be considered.
Limitation
Some of the limitations were the lack of the use of placebo, the difference in the surgical procedure type, the use of various other lubricants prior to application of mupirocin and the duration of the patient’s general anaesthesia, which might have affected the results of the study. In addition, the microbial culture samples were taken from the distal end of the nasotracheal tube, while the presence or absence of bacteria in the distal end of the nasotracheal tube does not mean definitive transportation or absence of transportation of bacteria into the trachea and the respiratory system. Therefore, it is suggested that future studies must be carried out by considering the limitations above and comparison of the suggested techniques to decrease the complications of nasal intubation.
Conclusion
Before nasotracheal intubation, use of mupirocin decreased the complications of nasal intubation after extubation and also decreased the colonization of S aureus and other Gram-negative bacteria.
*Statistically significant (p-value<0.05).
*Statistically significant (p-value<0.05)
*Statistically significant (p-value<0.05)
*Statistically significant (p-value<0.05)