Unusual Branching Pattern of the Portal Vein: Its Importance
Sreedhara B Cheluvashetty1, Vamsidhar Rachapalli2
1Consultant, Department of Radiology, BGS Global Hospital, Bengaluru, Karnataka, India.
2Consultant, Department of Radiology, BGS Global Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vamsidhar Rachapalli, 19-4-3H/15, STV Nagar, Tirupathi-517501, Andhra Pradesh, India.
E-mail: r_vamsidhar@yahoo.com
Portal vein anatomy and its branching pattern are of utmost importance for surgical planning of complex liver resections, living donor liver transplant and radiological procedures. The division of the vein at the porta hepatis, into the right and left branches is the most common branching pattern. Various branching variations have been described. We report a previously undescribed branching pattern of the right portal vein, where the segment VII vein arises directly from the left portal vein.
Anatomy, Liver transplantation, Portal vein embolization, Variations
Case Report
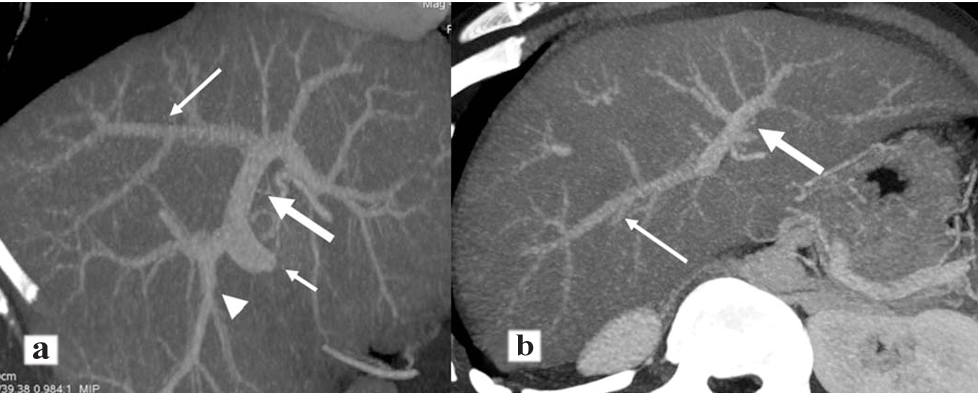
A 23-year-old male voluntary liver donor underwent triphasic computerized tomography of the abdomen as a part of transplant work up. Portal vein was noted to be formed by the union of superior mesenteric vein and splenic vein posterior to the neck of the pancreas. At the porta hepatis, the main portal vein bifurcated into right and left branches. The first branch from the right portal vein traversed inferiorly to supply segments V/VI [Table/Fig-1a]. Subsequently, it coursed cranially terminating as two major branches, supplying segments V and VIII. The left portal vein coursed horizontally towards ligamentum teres. There was a long branch arising from the left portal vein, which coursed across the Cantlie’s line, segment IVA and VIII and supplied predominately segment VII, with tiny branches to segment VIII along the course [Table/Fig-1a,b]. Segments II, III, IVA and IVB were supplied by left portal vein branches. The hepatic artery and veins demonstrated normal anatomy.
Reconstructed coronal (a) and axial (b) computed tomographic images. The short narrow arrow (a) corresponds to the main portal vein. The long narrow arrows (a and b) correspond to the portal vein branch to segment VII arising from the left portal vein. The thick arrow (a and b) corresponds to the left main portal vein. The arrow head (a) corresponds to branches supplying segments V and VI.
Discussion
Embryologically portal vein is derived from two vitelline veins and left umbilical vein. The intrahepatic branching pattern occurs due to selective involution and fragmentation of vitelline veins within the proliferating endodermal liver cords starting from the third to sixth week and is completed by the 12th week of intrauterine life [1,2]. Whilst hepatic parenchyma and hepatic vasculature develop independently, by 35th day of gestation the developing vasculature has to adapt to the fast growing hepatic parenchymal growth [1]. Variant anatomy arises as a consequence of abnormal obliteration of the connections that exist between the vitelline and umbilical veins in utero [2].
On computerized tomographic assessment, the normal portal vein anatomy is noted in 65-80% of cases [3]. The most common branching pattern is where the portal vein divides into right and left portal veins branches at the porta hepatis. As it courses cranially, the right portal vein first gives off branches to the caudate lobe and then divides into anterior and posterior branches, each of which subdivides into a superior and inferior segmental branch to supply the right lobe of the liver. Hence, the right portal vein supplies Couinaud segments V, VI, VII and VIII [2]. The left portal vein has an initial horizontal course prior to turning medially at the ligamentum teres. It provides branches to segments II and III, before undertaking a sharp angulation and terminating as branches to the superior and inferior segments of segment IV. Hence, the left portal vein supplies Couinaud segments II, III and IV [2,4]. Given its location, segment I is supplied by both the left and right portal vein branches [3].
Variant portal vein anatomy is not uncommon. It occurs in 0.09%-29.1% of the general population, with the commonest variation being the trifurcation of portal vein (7.8%-10.8%) [5]. Other more commonly reported variations are the right posterior segmental branch arising from the main portal vein (4.7%-5.8%) and right anterior segmental branch arising from the left portal vein (2.9%-4.3%) [4]. Unclassified, rare branching variations have also been described. These occur in less than 2% of the cases [3]. Some of these include the right posterior division arising from the left portal vein, right posterior division and segment V vein arising from the left portal vein, division of the portal vein into four branches (left portal branch and three separate right portal venous branches), congenitally absent portal vein and absent bifurcation of the portal vein [1,3,6-8]. Yasaka K et al., describes the right portal vein arising from the left portal vein [8]. However, in our case only segment VII vein arose from the left portal veins, whereas the remainder of the right lobe branches arise from the right portal vein itself. In their study of 1,384 patient, anomalous segmental portal venous origin traversing the midline was noted in 4% and involved only segments IV, V, VIII [9]. Sureka B et al., found segmental portal vein variations in approximately 1% of their study population with involvement of segments II, IV, V, VI only [10].
In our case, the right portal vein had an unusual branching pattern with no discernible anterior and posterior divisions. The first branch from the right portal vein coursed inferiorly to supply both segments V and VI. Subsequently, the right portal vein terminated by diving into two branches supplying segments V and VIII. Branch to segment VII was arising directly from the left portal vein, coursing across the Cantlie’s line and through segments IV and VIII. To the best of our knowledge, this variation has never been described previously in the literature.
The Cantlie’s line is the main portal fissure or scissura. This extends from the middle of the gall bladder fossa to the left side of the inferior vena cava, thereby dividing the liver into two functional halves; right and left livers. Each of these functional halves has their own portal and arterial supply and biliary drainage [11]. This forms the basis of surgical resection of the liver. Thus, a thorough understanding of the portal venous anatomy is important in guiding patient selection and planning of treatment, particularly when the patient is being considered for donor liver resection or segmental hepatectomy. During partial hepatectomy, all portal vein branches of the lobe to be resected, should be ligated to prevent bleeding and conversely, all portal vein branches of the remnant lobe must be patent to promote liver hypertrophy. Occlusion of a portal vein branch can cause portal hypertension and impair remnant lobe hypertrophy [3]. In addition, knowledge of the anatomy plays an important role for interventional radiologists who undertake portal vein embolization, particularly when segmental portal vein branch embolization is being considered. It guides the interventionist not only to decide the approach but also which branches need to be embolized. Inadvertent ligation or embolization can significantly contribute to the patient’s morbidity and mortality.
Conclusion
Prior to surgical or interventional procedures a thorough review of the cross-sectional imaging should be undertaken to ensure that variant anatomy can be identified and appropriate changes planned.
[1]. Kouadio EK, Bessayah A, Valette PJ, Glehen O, Nloga J, Diabatӑ AS, Anatomic variation: absence of portal vein bifurcationSurg Radiol Anat 2011 33(5):459-63. [Google Scholar]
[2]. Lee WK, Chang SD, Duddalwar VA, Comin JM, Perera W, Lau WF, Imaging assessment of congenital and acquired abnormalities of the portal venous systemRadiographics 2011 31(4):905-26. [Google Scholar]
[3]. Schmidt S, Demartines N, Soler L, Schnyder P, Denys A, Portal vein normal anatomy and variants: implication for liver surgery and portal vein embolizationSemin Intervent Radiol 2008 25(2):86-91. [Google Scholar]
[4]. Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A, Congenital and acquired anomalies of the portal venous systemRadiographics 2002 22(1):141-59. [Google Scholar]
[5]. Akgul E, Inal M, Soyupak S, Binokay F, Aksungur E, Oguz M, Portal venous variations. Prevalence with contrast-enhanced helical CTActa Radiol 2002 43(3):315-19. [Google Scholar]
[6]. Barchetti F, Pellegrino L, Al-Ansari N, De Marco V, Scarpato P, Ialongo P, Congenital absence of the portal vein in a middle-aged manSurg Radiol Anat 2011 33(4):369-72. [Google Scholar]
[7]. Takeishi K, Shirabe K, Yoshida Y, Tsutsui Y, Kurihara T, Kimura K, Correlation between portal vein anatomy and bile duct variation in 407 living liver donorsAm J Transplant 2015 15:155-60. [Google Scholar]
[8]. Yasaka K, Akai H, Kiryu S, Anomalous branching pattern of the portal vein: Right posterior portal vein originating from the left portal veinSurg Radiol Anat 2006 39(5):573-76. [Google Scholar]
[9]. Koç Z, Oguzkurt L, Ulusan S, Portal vein variations: clinical implications and frequencies in routine abdominal multidetector CTDiagn Interv Radiol 2007 13(2):75-80. [Google Scholar]
[10]. Sureka B, Patidar Y, Bansal K, Rajesh S, Agrawal N, Arora A, Portal vein variations in 1000 patients: surgical and radiological importanceBr J Radiol 2015 88(1055):20150326 [Google Scholar]
[11]. Bismuth H, Surgical anatomy and anatomical surgery of the liverWorld J Surg 1982 6:03-09. [Google Scholar]