Sarcoidosis is a multisystem granulomatous disease which frequently affects young adults. Because of its rarity, the exact incidence and prevalence of childhood sarcoidosis is not known. It mostly affects children of older age group i.e., 13–15 years. Early onset sarcoidosis (<5 years) is characterized by a triad of arthritis, uveitis and rash. Late onset sarcoidosis present with a multisystem disease similar to adults, with frequent pulmonary infiltrations and lymphadenopathy. Herein, we report a case of early-onset childhood sarcoidosis in a four-year-old female along with uncommon clinical features like cutaneous ulceration, onycholysis and geographical tongue and its rarity in the literature.
Case Report
A four-year-old female presented with multiple asymptomatic tiny red colored elevated skin lesions involving the face, chest, bilateral hands and legs since two years. The patient also had history of painless swelling of knee joint and finger tips with destruction of nail plate since one year. It was not associated with trauma. In addition to this, parents gave history of ulceration on both legs and tip of nose since six months. She also had history of pain and redness in both the eyes along with blurring of vision. There was no history of fever, malaise, weight loss, dyspnoea and cough with sputum or any other systemic complaints. There was no significant family history of tuberculosis or any other chronic disease. Vaccination history was complete including BCG vaccination.
General physical and systemic examinations were normal. On cutaneous examination, patient has multiple, well to ill-defined erythematous to skin coloured papules of size varying from 0.3×0.5 cm distributed symmetrically on extensor aspect of bilateral arms, forearms and chest [Table/Fig-1a,b]. Some of these papules were coalescing to form plaques on bilateral cheeks and chest with ulceration present on the lateral aspect of right leg and tip of nose [Table/Fig-1a-c]. On diascopy of these papules, apple jelly colour was present. She also had red to purple periungual discoloration associated with onycholysis of right ring finger. Several other fingers also showed nail dystrophy and longitudinal ridging [Table/Fig-1d]. On oral examination, there was a well-defined erythematous, depapillated areas bounded by whitish elevated borders on the dorsum of tongue resembling geographical tongue [Table/Fig-1a]. Bilateral cervical, inguinal and femoral significant lymphadenopathy was noted [Table/Fig-1e]. The largest of them was about 10 × 8 cm present in the right inguinal region. On palpation, lymph nodes were firm, mobile and non-tender. Ophthalmological examination also revealed bilateral uveitis on slit lamp examination.
(a) Multiple erythematous papules coalescing to form plaque on bilateral cheek with punched out ulcer on tip of nose and geographical tongue; (b) Multiple erythematous papules with mild central scaling on anterior aspect of chest; (c) An ulcer of 4×3 cm on lateral aspect of right leg and some of them healing with atrophic scar (red colour arrow showing ulcer and black colour arrow showing atrophic scar); (d) Periungual discoloration with onycholysis in right ring finger (arrow showing onycholysis); (e): Massive right inguinal lymphadenopathy of 10×8 cm size.

Laboratory findings showed: raised Erythrocyte Sedimentation Rate (ESR): 30 mm/h with decreased haemoglobin: 8.4 g/dl and white blood cell count: 3.4×109/l. Other routine biochemical tests, including random blood sugar, renal and liver function tests were within normal limits. Urine routine examination and urine calcium were also found to be normal. There was a marked increase in the Angiotensin Converting Enzyme (ACE) levels (258 U/L) (normal levels: 13–100 U/L). Other haematological test including serum calcium, alkaline phosphatase, Venereal Disease Research Laboratory test (VDRL) in dilution, vitamin B12 and folic acid blood levels were also normal.
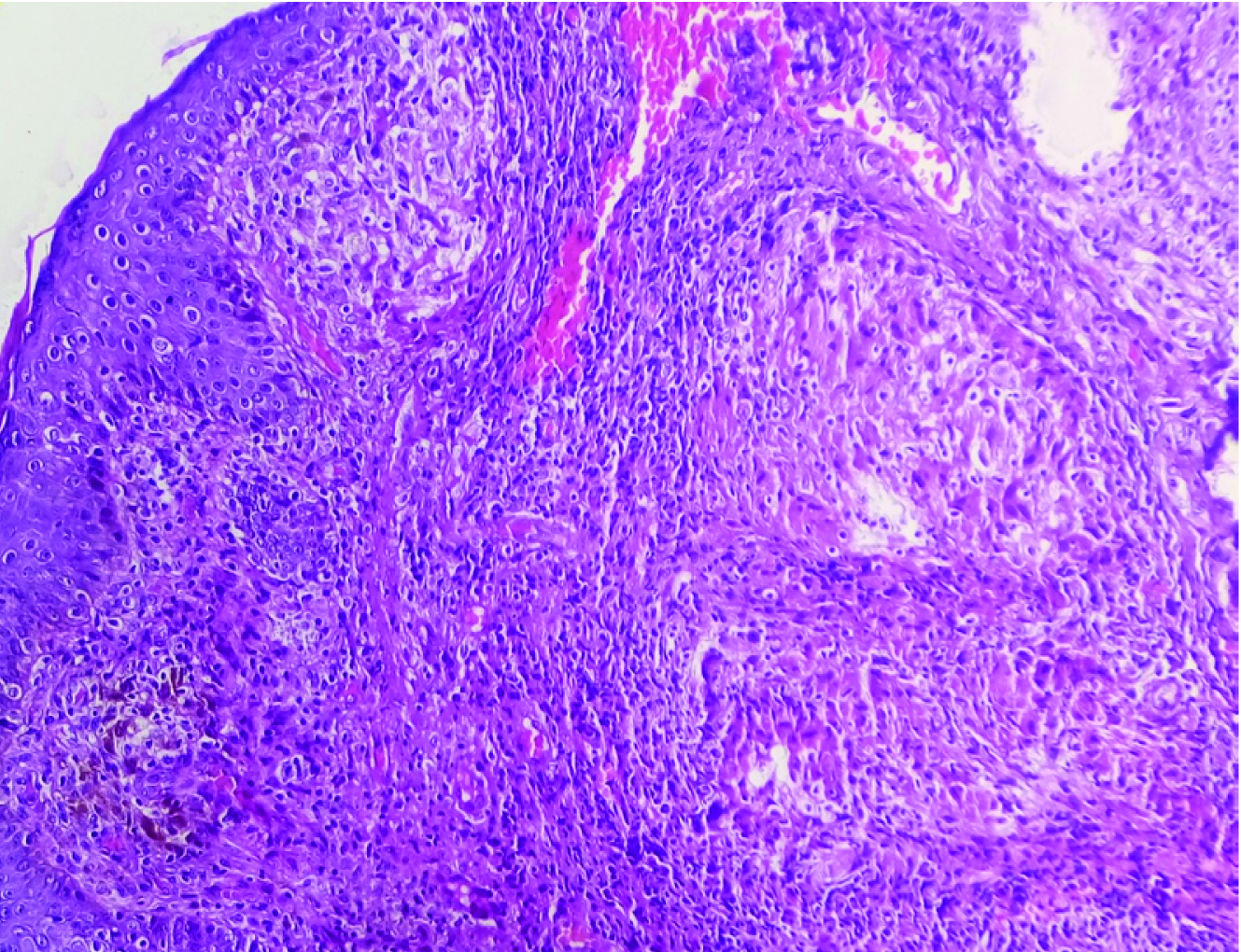
Tuberculin skin test as well as sputum for acid fast bacilli stain was negative. KOH mount from the dorsum of tongue was found to be negative. The x-ray chest, bilateral knee and hands were normal. No abnormalities were found in electrocardiogram and ultrasonography abdomen. The biopsy was done from a papular lesion over chest with the differential diagnosis of sarcoidosis, papulonecrotic tuberculosis and reticulohistiocytosis. Histopathological examination revealed an aggregate of epithelioid cells forming numerous non-caseating granulomas with some Multinucleated Giant Cells (MNGC), located in dermis suggesting a diagnosis of sarcoidosis [Table/Fig-2]. Special stains for mycobacteria and fungi were also negative. However, patient did not give consent for biopsy from other sites like tongue, nail bed and ulcer margins. Fine Needle Aspiration Cytology (FNAC) from right inguinal lymph node showed a collection of non-caseating epithelioid granulomas with few histiocytes that was compatible with sarcoidal granuloma. Based on these clinical features, raised ACE level, histopathological and FNAC findings a final diagnosis of sarcoidosis was made.
Photomicrograph showing non caseating granuloma with multinucleated giant cells, located in dermis. (H&E stain, ×10).
Patient was not taking any treatment since two years due to dilemma in diagnosis and familial constrains. Thus, she was started with high dose of prednisolone i.e., 2 mg/kg/day for one month along with injection methotrexate 0.5 mg/kg/week. This produced a marked improvement in cutaneous lesion and ulceration within three weeks. Steroid was tapered and stopped after three months. Patient was continued on weekly injection methotrexate for next six months.
Discussion
Childhood sarcoidosis is an uncommon granulomatous disease and difficult to diagnose because of its diverse presentations. Its diagnosis is based on clinical features and histolopathological examination. Childhood sarcoidosis may be divided into two distinct forms [1]. Older children (> 5 years) usually present with frequent hilar lymphadenopathy and pulmonary involvement, similar to that of adult sarcoidosis. In contrast, early-onset sarcoidosis (<5 years) is characterized by the triad of rash, uveitis, and arthritis. Thus, early onset sarcoidosis is a rare and appears to be different from sarcoidosis in older children and adolescents [2].
The proposed immunopathogenesis of sarcoidosis requires at least three major events: (1) antigenic exposure; (2) acquired cellular immunity against the antigen which is mediated through antigen presenting cells and antigen specific T lymphocytes; and (3) the appearance of immune effector cells which promote a nonspecific inflammatory response. Genetic also play an important role in determining its susceptibility as it is more common in relatives of an affected person. Thus, the interplay of antigenic and genetic factors plays a putative role in the pathophysiology of sarcoidosis [3].
As reliable epidemiological data are not available in the literature, the true incidence and prevalence of sarcoidosis in India is not yet assessed. According to an estimation in a respiratory unit at Kolkata, sarcoidosis constituted 10 to 12 cases per 1,000 new registrations in a respiratory unit and 61.2/100,000 new cases at a center in New Delhi in a report published in 2002 [4]. According to a study by Hoffman AL et al., in Denmark showed that the disease is uncommon in paediatric age group with an estimated incidence of 0.22–0.27 per 1, 00,000 children per year [5].
Cutaneous lesions are most common presentation occurring in 77% of early onset childhood sarcoidosis [2,6]. It usually presents with asymptomatic, discrete, maculopapular rash, which initially appears on face and extremities. Though, cutaneous sarcoidosis is a common, ulcerative atrophic lesions are quite rare. According to a study of 147 adults with cutaneous sarcoidosis, only 4.8% patients demonstrated an ulcerative-atrophic sarcoidosis [7]. Clinically, ulcerative sarcoidosis presents as punched out lesion with necrotic bases and heals with atrophic scar. It usually develops on the lower extremities, especially on the pretibial areas [8]. To our knowledge, there is no case report of childhood sarcoidosis with ulceration. Probably ours was the first case report of early onset sarcoidosis with ulceration.
Cutaneous tuberculosis such as Papulo Necrotic Tuberculid (PNT) and Tuberculosis Cutis Miliaris Disseminate (TCMD) can be kept as a potential differential diagnosis of sarcoidosis. PNT results from the immunological expression of an internal focus of TB in a patient with moderate to high degree of immunity. Tuberculin test is positive and Ziehl-Neelsen (ZN) staining is often negative [3]. Whereas in case of TCMD, tuberculin test may be negative but staining with ZN method is positive. On the hispathological examination of both the cases shows tubercular granuloma with caseous necrosis [1]. Thus in our case the diagnosis of cutaneous TB was ruled out on the basis of negative tuberculin test and absence of typical histopathological features. Another differential diagnosis of Multicentric Reticulo Histiocytosis (MRH) can be kept in our case due to the presence of papulonodular skin lesions with arthritis. In the literature, there are rare case reports of MRH occurring in children. In case of MRH biopsy specimen shows histiocytes. Thus, histopathological absence of histiocytes rules out its possibility [3].
Arthritis has been reported in 15-58% of childhood sarcoidosis [2]. It is usually presents with painless boggy effusions of synovium with good range of movement involving multiple joints [2]. Similarly, our patient also presents with painless swelling of bilateral knee joint and finger tips without limitation of movement. Ocular involvement is also common in childhood sarcoidosis. It may involve anterior or posterior segment of eye. Among anterior segment disease, uveitis andiritis are the most common manifestation, occurring in 24-58% of childhood sarcoidosis [2]. Our patient also presents with bilateral uveitis.
Peripheral lymphadenopathy is noted in 40-70% of cases, which is more common in late onset as compared to early-onset sarcoidosis [2]. In contrast to this, our patient presents with multiple inguinal and femoral lymadenopathy. Nail changes are quite rare in sarcoidosis. These are due to micro-compressive effects of sarcoidal granuloma between phalanx and nail plate [9]. In our case onycholysis was seen, although it is a very rare presentation in childhood sarcoidosis. Similarly, oral involvement is also an uncommon presentation of sarcoidosis [2]. In fact, there is only a hand full of cases exhibiting sarcoidosis-associated tongue impairment [10]. In our case, we observed geographical tongue in childhood sarcoidosis, which has not been reported previously.
In comparison to late onset sarcoidosis, early onset sarcoidosis usually lacks such varied presentations. The presence of onycholysis, geographical tongue and ulcerative atrophic lesions with generalized lymphadenopathy had puzzled the diagnosis. These unusual presentations might be a co-incidence or an association that is yet to be reported. If it is an association then it might be due the long duration of disease that had favoured the exaggerated immune response to produce such varied clinical presentation in this patient.
Currently, the treatment of choice for childhood sarcoidosis is topical or systemic corticosteroid. Methotrexate and azathioprine can be used in case of severe, non-responsive cases [11]. Combination of oral steroids in tapering dosage with methotrexate found to be safe and effective, as in our case. As it is a rare disease, the prognosis in children is not yet clear. However, a good prognosis has been reported in children which is as good as adults and most children experience significant improvement in clinical manifestations with treatment [2]. In a study by Hofffman AL et al., on Danish children, majority of patients had a favourable prognosis and most of them recovered in less than six years after onset of disease. However, long term multicentric studies are required to determine its exact prognosis in children [5].
Conclusion
This case showed that childhood sarcoidosis may unusually present with cutaneous ulceration, onycholysis and geographical tongue. So, any patient of less than five years presenting with these features with or without the characteristic triad of arthritis, uveitis and rash, sarcoidosis must be considered as differential for early diagnosis and prevention of serious complication.
[1]. Marcoval J, Mana J, Griffiths CEM, Barker J, Bleiker T, Chalmers R, Creamer D, SarcoidosisRook’s Textbook of Dermatology 2016 39th ednOxfordWiley Blackwell Science:98.1-17. [Google Scholar]
[2]. Shetty AK, Gedalia A, Childhood sarcoidosis. A rare but fascinating disorderPediatr Rheumatol Online J 2008 6:16 [Google Scholar]
[3]. Marchell RM, Thiers B, Judson MA, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, SarcoidosisFitzpatrick’s Dermatology in General Medicine 2012 18thednNew YorkMcGraw Hill:1869-78. [Google Scholar]
[4]. Sharma SK, Mohan A, Sarcoidosis in India: not so rareJ Indian Acad Clin Med 2004 5:12-21. [Google Scholar]
[5]. Hoffman AL, Milman N, Byg KE, Childhood sarcoidosis in Denmark 1979–1994: incidence, clinical features and laboratory results at presentation in 48 childrenActa Paediatr 2004 93:30-36. [Google Scholar]
[6]. Wong L, Ho J, Yen Y, Early-onset childhood sarcoidosis: a case reportDermat ologicasinica 2011 29:125-28. [Google Scholar]
[7]. Yoo SS, Mimouni D, Nikolskaia OV, Kouba DJ, Sauder DN, Nousari CH, Clinicopathologic features of ulcerative-atrophic sarcoidosisInt J Dermatol 2004 43:108-12. [Google Scholar]
[8]. Albertini JG, Tyler W, Miller OF, IIIUlcerative sarcoidosis. Case report and review of the literatureArch Dermatol 1997 133:215-19. [Google Scholar]
[9]. Losada-Campa A, De la Torre-Fraga C, de Gomez Lian˜o A, Cruces-Prado MJ, Histopathology of nail sarcoidosisActaDerm Venereol 1995 75:404-05. [Google Scholar]
[10]. Bouaziz A, Le Scanff J, Chapelon-Abric C, Varron L, Khenifer S, Gleizal A, Oral involvement in sarcoidosis: report of 12 casesQJM 2012 105:755-67. [Google Scholar]
[11]. Doherty CB, Rosen T, Evidence-based therapy for cutaneous sarcoidosisDrugs 2008 68:1361-83. [Google Scholar]