An Unusual Case of Giant Arterio-Venous Malformation of Anterior Abdominal Wall
PS Aravinda1, Hirdaya Hulas Nag2, Vithal Kumar M. Betigeri3, Puja Sakhuja4, Ashok Sharma5
1 Senior Resident, Department of G.I Surgery, GB Pant Hospital, New Delhi, India.
2 Professor, Department of G.I Surgery, GB Pant Hospital, New Delhi, India.
3 Professor, Department of CTVS, GB Pant Hospital, New Delhi, India.
4 Professor, Department of Pathology, GB Pant Hospital, New Delhi, India.
5 Professor, Department of Radiology, GB Pant Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hirdaya Hulas Nag, Professor, Department of G.I Surgery, GB Pant Hospital, New Delhi-110002, India.
E-mail: hirdayanag@gmail.com
Arterio-Venous Malformations (AVMs) are high flow vascular anomalies, commonly seen in head, neck and extremities. AVMs represent a direct connection between the arterial and the venous systems. They are congenital, often asymptomatic and rarely manifest before adolescence. Depending on the site, size and symptoms, treatment options varies from conservative management to surgical resection. Here, we report a case of 20-year-old male patient with long standing lump in the anterior abdominal wall with no typical clinical features of vascular lesions. However, imaging findings were suggestive of vascular malformation, and final histopathological examination revealed arterio-venous malformation.
Atypical arterio-venous lesions, High flow vascular malformation, Vascular anomalies
CASE
A 20-year-old male patient presented with lump in the Left Upper Quadrant (LUQ) of the abdomen for the past 15 years. The lump was gradually incearsing in size, associated with dull aching pain. He had no bowel and bladder symptoms. He also underwent a session of injection sclerotherapy for the lump at another hospital, three years ago. However, the size of the lump didnot subside.
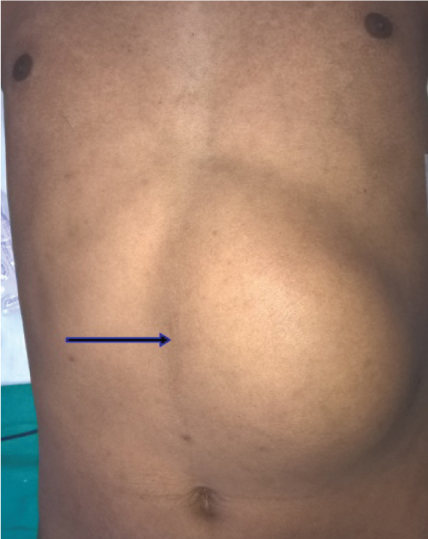
On clinical examination, a large, non tender, non pulsatile, non reducible, non compressible, firm lump with no local rise of temperture, normal overlying skin and not moving with respiration was palpable in LUQ of the abdomen, seemed to arising from the underlying muscles [Table/Fig-1]. Clinical diagnosis of soft tissue sarcoma was made and further evaluated with radiological investigations. Ultrasound was suggestive of a large hyperechoic mass in the left paramedian location extending from epigastrium to supraumbilical region involving subcutaneous fat and anterior abdominal wall muscles. Contrast Enhanced Computed Tomography (CECT) revealed a well defined abdominal wall mass involving left rectus abdominis muscle, measuring 12 x 10 x 7 cm with prominent intralesional vascularity and enhancing perilesional neovascularity [Table/Fig-2]. The mass was fed by left superior epigastric artery at the upper pole and left inferior epigastric artery at lower pole [Table/Fig-3].
CECT- Mass in the left rectus muscle with prominent intralesional vascularity (arrow).
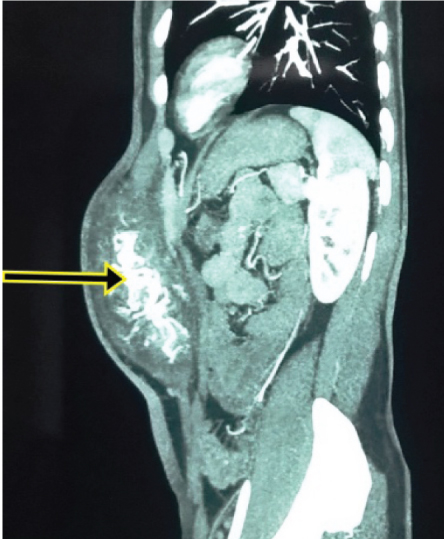
CT Angiography-Mass fed by superior (Yellow arrow) and inferior epigastric arteries (blue arrow).

He underwent surgical resection of the lump. Intraoperatively there was a giant, firm lump arising from the left rectus abdominis muscle [Table/Fig-4].
Mass arising from the rectus muscle (arrow).

On gross specimen examination, the mass was lobular, measuring 17 x 12 x 7 cm, without a well-defined capsule. The cut surface was grey-white to yellowish-brown, having a soft to fleshy to feel.
No necrotic area was identified. Histological examination revealed a lobular architecture comprising of admixture of small sized vessels predominantly capillaries, admixed with few larger arteries [Table/Fig-5] and venules.
A large artery with hemangiomatous component in the wall. (H&E 4X).
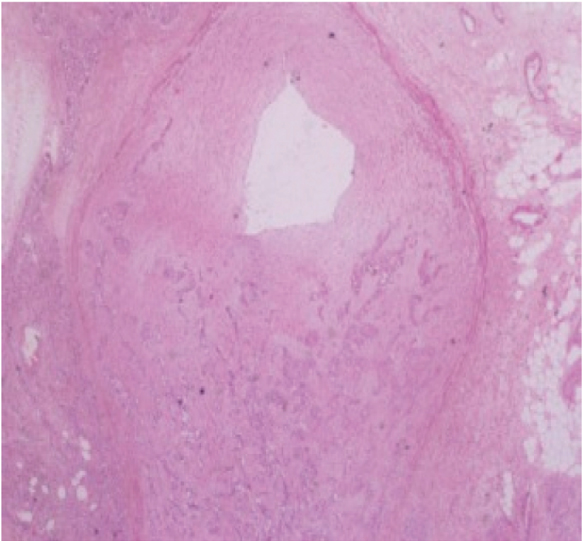
Numerous thin variably sized vessels show branching and intercommunicating complex network of vessels were also seen. Periphery of the lesion showed presence of lipomatous tissue and skeletal muscle. The mitotic count was low (<01/10 high power field). Verhoeff-Van Gieson (VVG) stain shows presence of interrupted and discontinuous elastic lamina in the vessels.
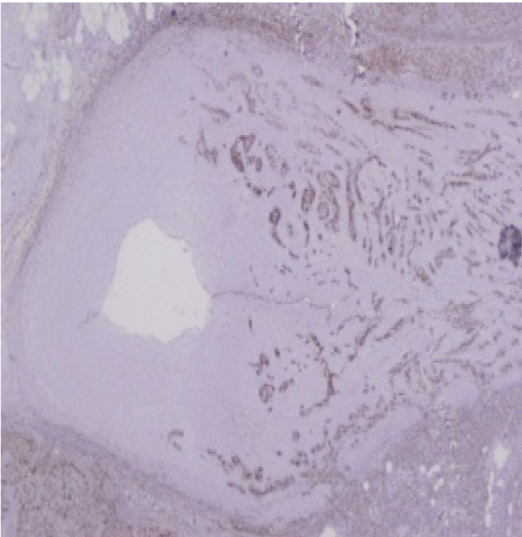
The cells were negative with HMB-45 and beta catenin, but showed intense positivity with CD34 [Table/Fig-6]. A histological diagnosis of AVM with hemangiomatous change was given. The patient is doing well at eight months’ follow up.
The same vessel showing CD34 positive staining of endothelial cells (Immunohistochemistry 4X).
Discussion
Vascular malformations are localized defects of vascular morphogenesis caused by dysfunction in embryogenesis and vasculogenesis [1]. They are classified into two large groups, hemangiomas and vascular malformations [2]. Vascular malformation are further classified into slow (low) flow (for example, capillary, venous and lymphatic malformations), high (fast) flow (for example, arterial malformation, arteriovenous fistula, AVM and complex combined vascular malformations [3].
Vascular malformations are commonly seen in head, neck and extremities and rarely affect the trunk [4]. They present as easily compressible blue masses. There are only few case reports regarding AVM of anterior abdominal wall, however, majority of patients had typical clinical features. In a case report by Alessandrino F et al., patient had vascular malformation of the abdominal wall, presenting as soft, bluish, compressible lesion [5]. In an another case report by Kumar A et al., in a patient with giant posterior abdominal wall AVM, there was a soft, compressible mass in the left flank with palpable thrill and audible bruit [6]. In our case, patient had firm, non compressible mass with normal overlying skin, leading to diagnostic dilemma. Although clinical features were not typical of AVM, imaging findings were suggestive of AVM, which was confirmed by histopathological examination.
Depending on the site, size, stage and symptoms, they can be treated conservatively, sclerotherapy or embolization with or without surgery or surgery alone. The most effective treatment for AVMs is transarterial embolization [7]. In our patient, transarterial embolization couldnot be done due to unavailability of technical expertise at that time and he was treated by surgical excision.
Conclusion
Giant AVM of anterior abdominal wall is very rare and imaging studies helps in the diagnosis, especially in patients with atypical clinical features. It should be kept as one of the differential diagnsosis in young patients with long standing abdominal wall lump.
[1]. Enjolras O, Wassef M, Chapot R, A review of: “Color atlas of vascular tumors and vascular malformations” 2007 Cambridge University Press:299 [Google Scholar]
[2]. Mulliken JB, Glowacki J, Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristicsPlastic and reconstructive surgery 1982 69(3):412-20. [Google Scholar]
[3]. Jackson IT, Carreño R, Potparic Z, Hussain K, Hemangiomas, vascular malformations, and lymphovenous malformations: classification and methods of treatmentPlastic and reconstructive surgery 1993 91(7):1216-30. [Google Scholar]
[4]. Ernemann U, Kramer U, Miller S, Bisdas S, Rebmann H, Breuninger H, Current concepts in the classification, diagnosis and treatment of vascular anomaliesEuropean Journal Of Radiology 2010 75(1):2-11. [Google Scholar]
[5]. Alessandrino F, Maira A, Tarantino CC, US and MRI features in venous vascular malformation of the abdominal wall. A case reportJournal of ultrasound 2012 15(3):171-73. [Google Scholar]
[6]. Kumar A, Singh M, Sankhwar S, Giant posterior abdominal wall arteriovenous malformation mimicking renal mass: rare imagesBMJ Case Reports 2014 2014:bcr2014204311 [Google Scholar]
[7]. Yakes WF, Rossi P, Odink H, Arteriovenous malformation managementCardiovascular and interventional radiology 1996 19(2):65-71. [Google Scholar]