Introduction
Femoral shaft fractures are one of the common injuries that is treated by open reduction, with internal fixation by plate and screws or intramedullary nailing, which can achieve a high union rate.
Aim
To evaluate the outcome of using closed external fixation to augment a failing plate; with signs of screw loosening and increasing bone/plate gap; a failed plate; broken plate; screws completely out of bone with redisplacement of fracture.
Materials and Methods
A retrospective study on 18 patients, aged between 17-42 years, who presented between 6-18 weeks after initial surgical fixation, with pain, difficulty in limb function, deformity and abnormal movement at fracture site, was done. X-Rays showed plating failure with acceptable amount of callus, which unfortunately had refractured. Cases associated with infection and no radiological evidence of callus formation were excluded from this study. Closed reduction was done by manipulation, then fracture fixation by AO external fixator. The patients were encouraged for full weight bearing as early as possible with dynamization later on.
Results
Of the 18 patients who underwent external fixation after close reduction, 15 cases showed bone healing in a period between 11-18 weeks (mean of 14.27 weeks) with good alignment (Radiologically). Removal of external fixator was done followed by physical therapy thereafter.
Conclusion
Closed external fixation for treatment of failing or failed femoral plating, achieves good success rate and has less complications, is a short time procedure, especially in a hospital with limited resources.
Introduction
Femoral shaft fractures are one of the common injuries, that occur mostly in young males after high energy, trauma and in old females after a low energy fall. Open reduction with internal fixation by plate and screws or intramedullary nailing can achieve a high union rate [1,2].
There has been an advance in the AO/Association for the femoral shaft plating technique during the past few years, that includes the use of long plates and less plate screws, fewer one cortex screws at the ends of plate and less number of lag screws outside the plate. These changes indicate an evolving technique of plate osteosynthesis that improves the close reduction techniques, biologic internal fixation and improved biomechanics. Outcome data suggest that there has been an improvement in time for bone healing, a decrease in the percentage of implant failures, delayed unions, non union, malunion, number of surgical revision and in overall rate of failure [3].
The management of femoral shaft fracture non union is still a challenge in orthopaedic operations. It represents a serious postoperative problem for the patient [4,5], including implant failures such as broken plate and/or screw, screws loosening or extrusion, refracture after removal of plate, non union, and infection [6].
There are several other operative methods for treating femoral shaft delayed union and non union, including nail dynamization [7,8] nail exchange [9], plate osteosynthesis [10,11] and monolateral external fixation [12].
The management of implant failure in femoral shaft fracture especially if associated with some element of delayed union/non union is a dilemma for an orthopaedic surgeon. It represents a serious postoperative complication for the patient, associated with longer time of restricted mobility, shortening, deformity, knee joint stiffness and the need for second major surgery, providing osteosynthesis plus bone graft after failed plate removal [4].
In our regional hospitals, most cases of closed femoral shaft fractures are fixed by classical AO plates and screws because of shortage of locked IM nail or other methods of fixation (because of limitation of resources). For this reason, cases of broken or loosening of plates and/or screws are frequently seen, other reasons probably include: early unguarded weight bearing, use of shorter plate, second fall or trauma, concealed infection and some form of delayed/non union.
In this study, we tried to evaluate the outcome of using closed external fixation to augment a failing plate, with signs of screw loosening and increasing bone/plate gap or failed plate, broken plate or screws completely out of bone with redisplacement of fracture.
Materials and Methods
A retrospective study was done at Al-Hilla Teaching Hospital on 18 patients who presented with implant failure (plate and screw fixation for femoral shaft fracture) between September 2008 to November 2015. The Institutional Review Board approved this study. Informed consent was obtained from each patient for surgical procedure.
Fifteen cases were male, three were female, age between 17 years and 42 years, all of them were otherwise healthy, 14 cases had fracture femur as a result of Road Traffic Accident (RTA) and four cases due to Fall From Height (FFH), all were treated initially (elsewhere, by other orthopaedic surgeons) by open reduction and internal fixation using AO plate and screws.
All the patients presented between 6-18 weeks after surgical fixation with pain, difficulty in limb function, deformity and abnormal movement at fracture site. X-Rays showed plating failure (broken plate/or screws, extruded screws or increasing bone to plate space) with significant callus formation and deformity. Cases associated with infection and no evidence of callus formation were excluded from this study.
Surgical technique: Patients were prepared for the procedure, under general or regional anaesthesia and X-Ray control (C-arm fluoroscopy), closed reduction by manipulation (most cases were easy even the slipped screws might find their way back to original bone tracks), then fracture fixation was done with AO external fixator, three pins proximal and three pins distal to the site of plate. At the same time, we did manipulation for the knee as most cases had variable degrees of stiffness.
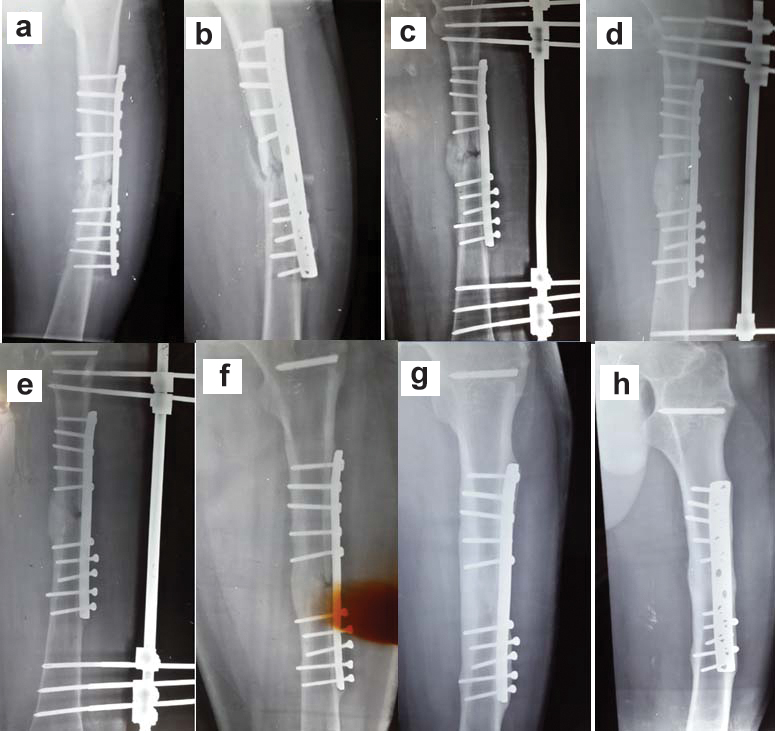
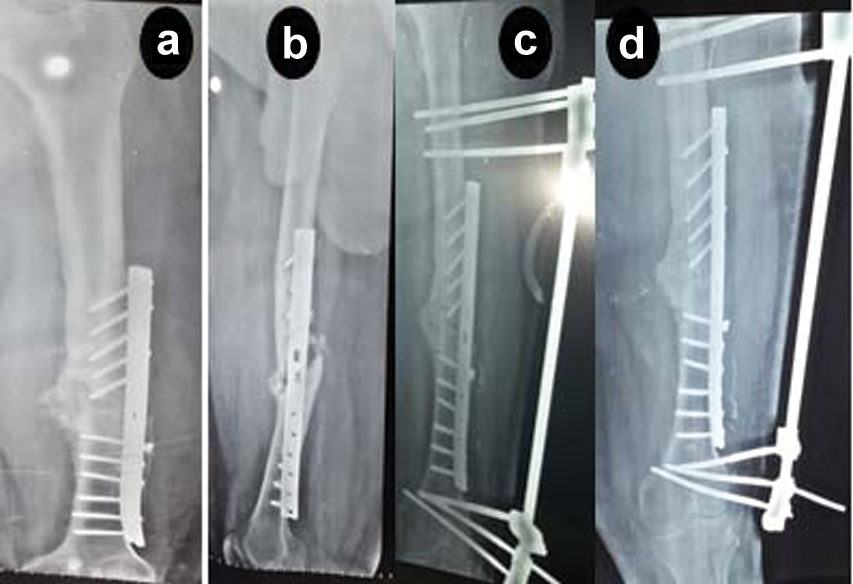
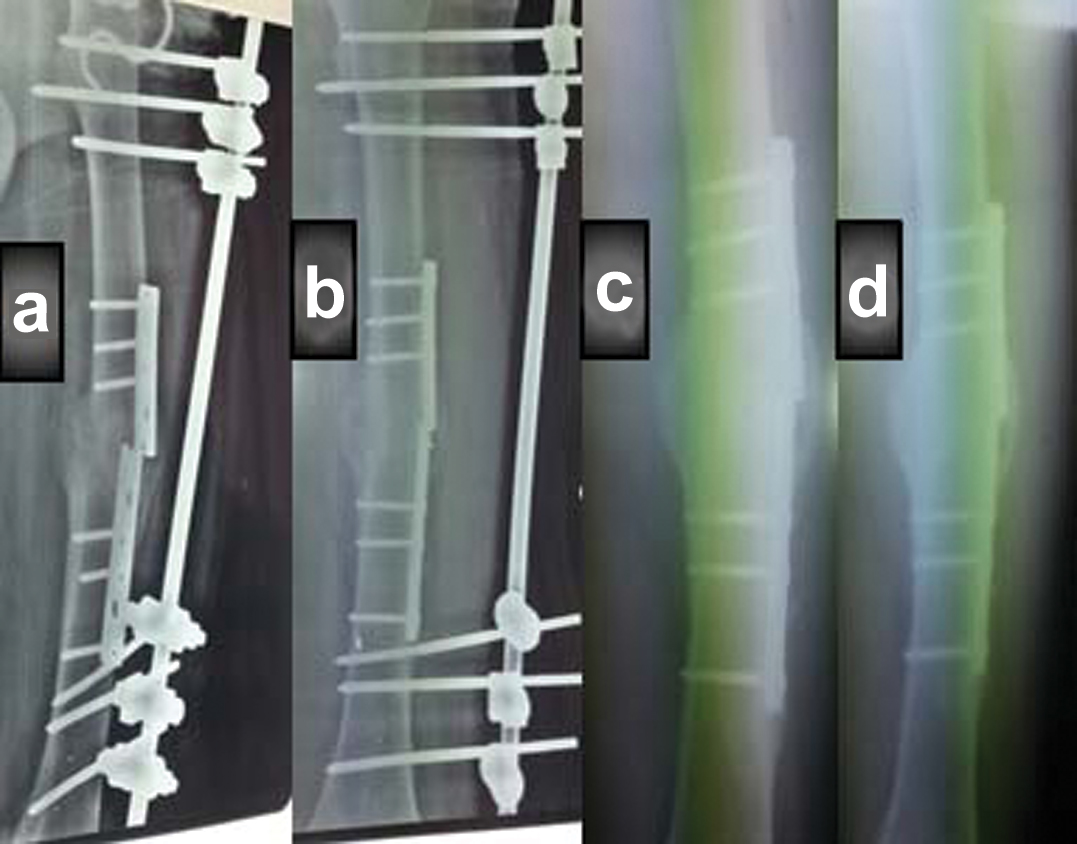
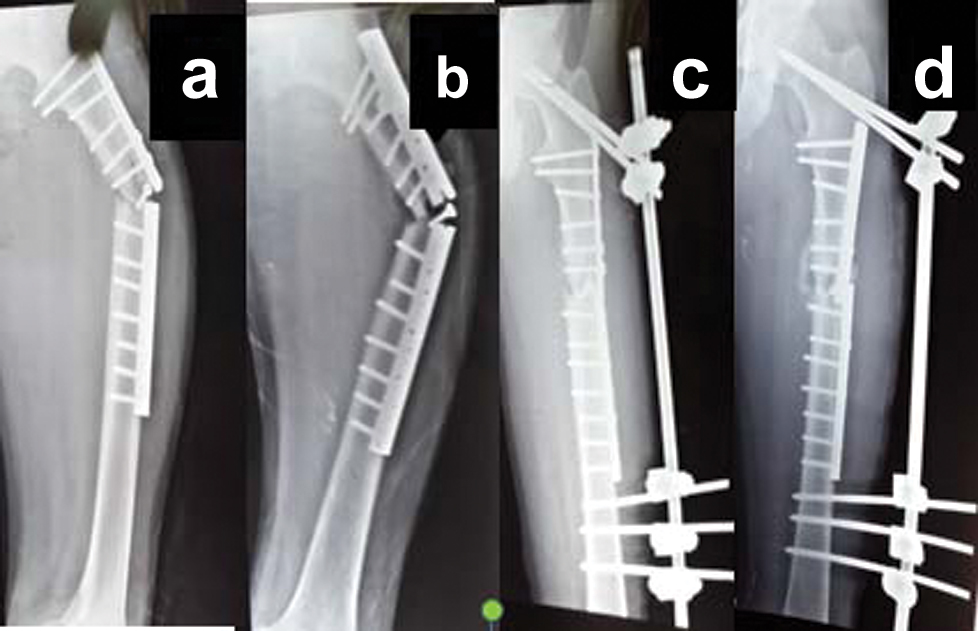
Postoperative care and follow up: The patients were encouraged full weight bearing as early as possible (even on the same day of operation) though most of them preferred use of crutches for 1-2 weeks. The patients were advised atleast 4-5 hours/day full weight bearing until solid union. Dynamization, by untightening the proximal or distal pins or both later on, was done at follow up visits when X-Ray showed obliteration of fracture line (in the last four weeks before the removal of external fixator [Table/Fig-1,2,3 and 4].
X-Ray series of patient; a,b) Extruded screws of distal segment; c) external fixation after reduction; d) Broken proximal pin, and removed; e,f) External fixation removed; g,h) Complete healing.
a,b) Extruded screws (AP and Lat. veiw); c,d) Refixation by closed external fixation.
(a,b) Broken plate, fixed by external fixation; (c,d) Healed fracture and external fixation was removed.
(a,b) Broken plate with deformity; (c,d) Close reduction and external fixation.
Removal of external fixator was done in the outpatient clinic under local anaesthesia. The retained implant (internal fixator) was removed in the following weeks.
Results
Eighteen patients underwent closed reduction and external fixation. [Table/Fig-5] shows data related to the patients regarding the types of fracture, site of fracture, the type of initial fracture, fixation and the time of complication and the time needed for healing after external fixator application.
Clinical data for 18 patients who were treated by external fixation.
| No | Type of fracture | Site of fracture | Failing/failed plating | Time of complication | Time for healing |
|---|
| 1 | Oblique | Upper third | Broken plate | 10 wks | 12 wks |
| 2 | Comminuted | Shaft | Broken plate | 14 wks | 16 wks |
| 3 | Comminuted | Upper third | Loosened screws | 13 wks | 13 wks |
| 4 | Comminuted | Lower third | Broken screws | 11 wks | 12 wks |
| 5 | Oblique | Lower third | Broken plate | 12 wks | Not healed |
| 6 | Comminuted | Shaft | Broken plate | 8 wks | 18 wks |
| 7 | Comminuted | Lower third | Loosened screws | 16 wks | 13 wks |
| 8 | Oblique | Upper third | Broken plate | 10 wks | 12 wks |
| 9 | Comminuted | Lower third | Broken plate | 13 wks | 13 wks |
| 10 | Oblique | Shaft | Broken screws | 6 wks | Not healed |
| 11 | Comminuted | Shaft | Loosened screws | 8 wks | 16 wks |
| 12 | Comminuted | Lower third | Broken screws | 10 wks | 15 wks |
| 13 | Oblique | Lower third | Loosened screws | 9 wks | 11 wks |
| 14 | Transverse | Shaft | Broken plate | 13 wks | 16 wks |
| 15 | Comminuted | Upper third | Broken screws | 12 wks | 15 wks |
| 16 | Oblique | Lower third | Broken plate | 18 wks | Not healed |
| 17 | Comminuted | Lower third | Loosened screws | 10 wks | 16 wks |
| 18 | Oblique | Lower third | Loosened screws | 14 wks | 17 wks |
As seen in [Table/Fig-5], the site of femoral fractures, 9 (50%) cases were in the lower third, 4 (22%) in the upper third and 5 (28%) were in the shaft.
Eight cases (45%) presented with broken plate with angulations and limping, while other 10 (55%) cases presented with broken or loosened screws above or below the fracture site. Of the total, 11 (61%) cases presented after re-trauma on the fixed fracture, and 7 (39%) patients due to early weight bearing after initial fixation by plate and screws, had re-fracture.
The time of presentation with complication in these patients ranged between 6-18 weeks after initial internal fixation (mean of 11.5 weeks).
Fifteen patients achieved good bone healing in a period between 11-18 weeks (mean of 14.27 weeks) with good alignment and removal of external fixator was done followed by physical therapy, three cases did not achieve healing by this method (after 27 weeks from external fixation) and were treated by removal of external and internal fixator. In these patients plate and screws with bone graft were used, due to which bone healing was delayed upto seven months and later.
The main problems of this type of management are:
Pin tract infection: It occurred in six cases, mostly affecting the uppermost or lowermost pin, this could be related to the mechanical factor, as the skin is rubbed around pins during hip and knee flexion. Five of them responded well to conservative treatment and in the sixth patients, the infected loose pin (uppermost one) was removed.
Broken pin: This happened in one case, in which the upper most pin was broken. The external segment was removed and the internal part was left inside, that did not cause any problem.
Knee stiffness: It occured in seven cases, all of them did well after physical therapy.
Discussion
Implant failure with respect to femoral bone fractures, is still a challenge to orthopaedic surgeons, in our practice, the best method of treatment is evolving and in most cases is individualized.
In hospitals of our region, because of limitation of resources, use of plate and screws for fixation of femoral shaft fractures, is still preferred. However, the problem of broken internal fixator, and/or loosening of screws does occur at times.
Many factors are related to such complications, one of them is rigidity of internal fixator, others are early unrestricted weight bearing, second trauma before complete healing of the fracture, concealed infection slowing healing process and poor technique of fixation (too short plate, screws in the fracture site or screws purchasing near cortex only).
Most of the references suggest treatment of such problem by removal of failed plate and application of another one plus bone graft or interlocked IM nail and grafting, both are demanding surgeries requiring relatively long time of anaesthesia with blood transfusion and restricted mobility for variable periods of time. If concealed infection is discovered, the problem is doubled [1,2,4,5].
Simple method of fixation after closed reduction using C-arm fluoroscopy achieves good alignment, a procedure requiring relatively short time, without removal of the failed plate or application of another plate on the other side as some prefer, or adding bone graft [2-4,7,10]. Another advantage is that, the time of restricted mobility is very short as the patient must and should start full weight bearing as soon as possible.
Dynamization principle used by untightening the distal and/or proximal pins with partial weight bearing to enhance callus formation and shorten the time of bone healing, agrees with what was mentioned by Checketts RG et al., [13]. The procedure used did not interfere with already formed callus at the fracture site which resulted in a shorter time required for solid union.
Regarding the wide range of time needed to achieve healing after application of external fixator, it may depend on many factors such as the age of the patient, site and type of fracture in addition to the broken metal causes. That is why the results show wide range of time to achieve bone healing.
Regarding the complications related to our study, we did not face any major complication, which may affect the results, there was pin tract infection in six patients and all of them were cured. Joint stiffness occurred in seven cases but all of them regained good range of movements after physical therapy.
Limitation
The limitations of current study were that there were less number of the patients. As such complication (broken internal fixator) was limited and there is no similar study to compare with it.
Conclusion
The use of closed external fixation for treatment of failing or failed femoral plating, if not associated with signs of non union, is a good choice (in the hospitals with limited resources, lack of more recent techniques of fixations), with short time procedure, no surgical exploration, less risk of complications, shorter healing time and good success rate.
[1]. Kanellopoulos AD, Soucacos PN, Management of nonunion with distraction osteogenesisInjury 2006 37S:S51-55. [Google Scholar]
[2]. Gelalis ID, Politis AN, Arnaoutoglou CM, Korompilias AV, Pakos EE, Vekris MD, Diagnostic and treatment modalities in nonunions of the femoral shaft. A reviewInjury 2012 43:980-88. [Google Scholar]
[3]. Rozbruch SR, Müller U, Gautier E, Ganz R, The evolution of femoral shaft plating techniqueClin Orthop Relat Res 1998 (354):195-208. [Google Scholar]
[4]. Maimaitiyiming A, Amat A, Rehei A, Tusongjiang M, Li C, Treatment of the femoral shaft nonunion with double plate fixation and bone grafting: A case series of 14 patientsInjury 2015 46:1102-07. [Google Scholar]
[5]. Ma YG, Hu GL, Hu W, Liang F, Surgical factors contributing to nonunion in femoral shaft fracture following intramedullary nailingChinese Journal of Traumatology 2016 19:109-12. [Google Scholar]
[6]. Wu CC, The effect of dynamization on slowing the healing of femur shaft fractures after interlocking nailingJ Trauma 1997 43:263-67. [Google Scholar]
[7]. Furlong AJ, Giannoudis PV, DeBoer P, Matthews SJ, MacDonald DA, Smith RM, Exchange nailing for femoral shaft aseptic non unionInjury 1999 30:245-49. [Google Scholar]
[8]. Abdel-Aa AM, Farouk OA, Elsaved A, Said HG, The use of a locked plate in the treatment of ununited femoral shaft fracturesJ Trauma 2004 57:832-36. [Google Scholar]
[9]. Bellabarba C, Ricci WM, Bolhofner BR, Results of indirect reduction and plating of femoral shaft nonunions after intramedullary nailingJ Orthop Trauma 2001 15:254-63. [Google Scholar]
[10]. Choi YS, Kim KS, Plate augmentation leaving the nail in situ and bone grafting for non union of femoral shaft fracturesInt Orthop 2005 29:287-90. [Google Scholar]
[11]. Abeed RI, Naseer M, Abel EW, Capacitively coupled electrical stimulation treatment: Results from patients with failed long bone fracture unionsJ Orthop Trauma 1998 12:510-13. [Google Scholar]
[12]. Kim SJ, Shin SJ, Yang KH, Moon SH, Lee SC, Endoscopic bone graft for delayed union and nonunionYonsei Med J 2000 41:107-11. [Google Scholar]
[13]. Checketts RG, Moran CG, Jennings AG, 134 tibial shaft fractures managed with the dynamic axial fixatorActa Orthop Scand 1995 66(3):271-74. [Google Scholar]