Simultaneous Bilateral Anterior and Posterior Lenticonus in Alport Syndrome
Ravi Kant Bamotra1, Meenakshi2, Prem Chandra Kesarwani3, Shazia Qayum4
1 Senior Resident, Department of Ophthalmology, GMCH, Chandigarh, India.
2 Senior Resident, Department of Ophthalmology, AIIMS, Rishikesh, Uttrakhand, India.
3 Senior Resident, Department of Ophthalmology, AIIMS, Delhi, India.
4 Senior Resident, Department of Ophthalmology, MMIMSR, Ambala, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravi Kant Bamotra, Senior Resident, Department of Ophthalmology, D block, 3rd floor, GMCH Sector-32, Chandigarh-160030, India.
E-mail: dr.ravibamotra@gmail.com
Alport syndrome is an inherited disease characterized by progressive renal failure, hearing loss, and ocular abnormalities like anterior lenticonus, corneal opacities, cataract, central perimacular and peripheral coalescing fleck retinopathies, and temporal retinal thinning. Although anterior lenticonus is common in Alport syndrome, simultaneous anterior and posterior lenticonus is a rare presentation. We report a case of a 22-year-old female with simultaneous anterior and posterior lenticonus presentation in which ocular examination lead to the detection of Alport syndrome. The patient had sensorineural deafness as well as microscopic haematuria. Clear lens extraction was performed in both eyes to eliminate lenticular irregular astigmatism for visual rehabilitation.
Astigmatism, Renal disease, Sensorineural deafness
Case Report
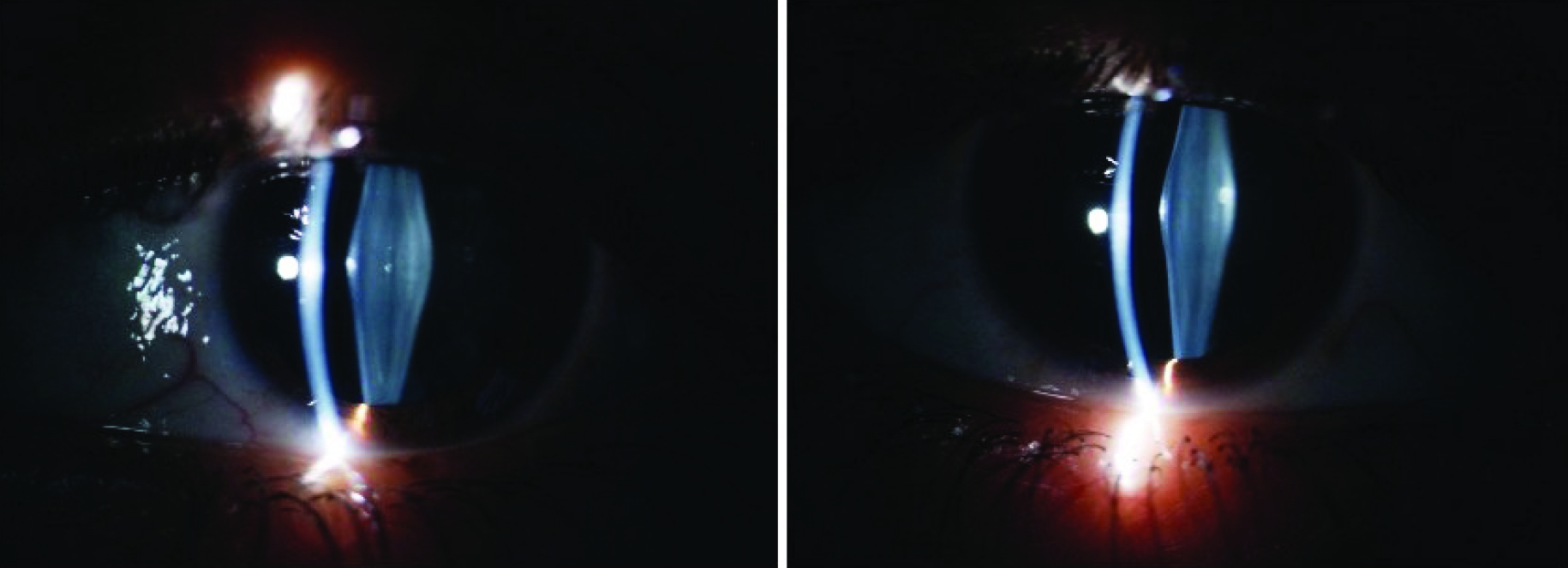
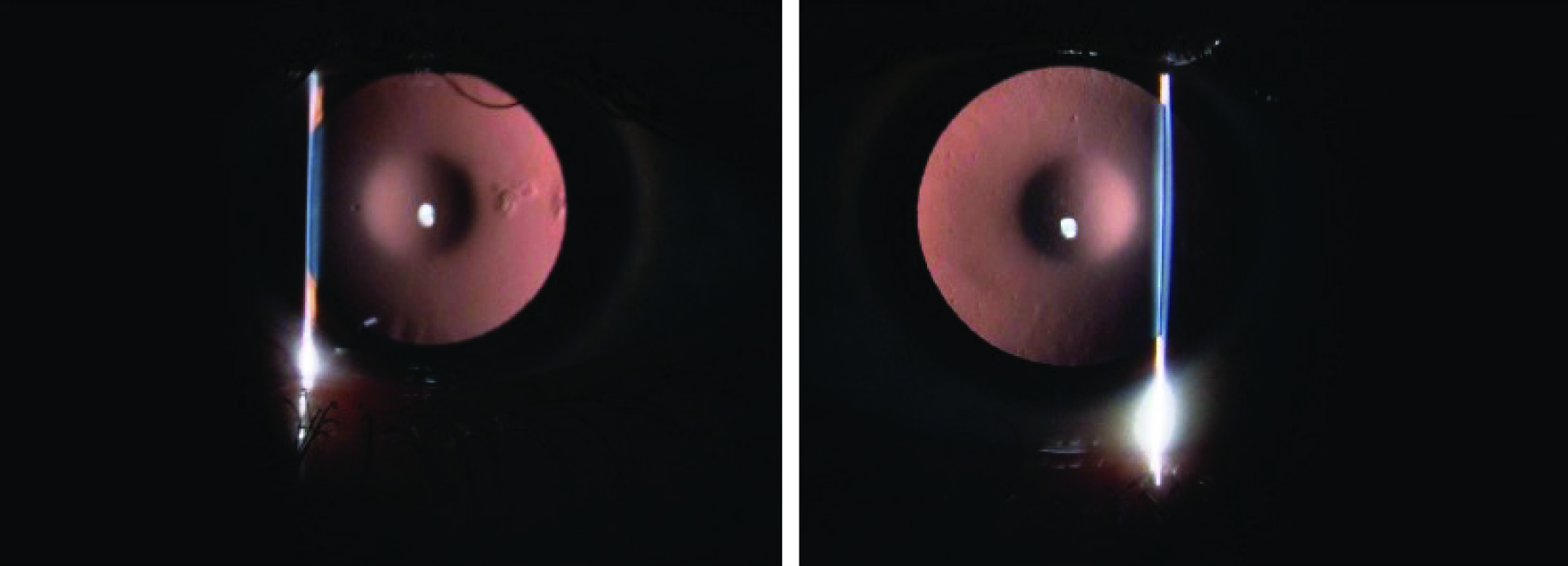
A 22-year-old female presented with diminution of both distant and near vision for last seven years. On ocular examination, the Best Corrected Visual Acuity (BCVA) was 6/24 in both eyes. Streak retinoscopy revealed irregular astigmatism in both eyes. On slit lamp examination, both corneas were clear, pupillary reactions were normal and Intraocular Pressure (IOP) was 14 in RE (Right Eye) and 16 in LE (Left Eye). Lens showed anterior and posterior lenticonus in both eyes [Table/Fig-1]. On distant direct ophthalmoscopy, oil droplet reflex was seen although fundus examination revealed no abnormalities [Table/Fig-2]. Electroretinography was normal in both the eyes.
Slit lamp picture showing anterior and posterior lenticonus in both eyes.
Slit lamp picture showing ‘oil droplet sign’ in both eyes on retro-illumination.
Based on the clinical features, suspicion of Alport syndrome was made. Patient was asked about the history of haematuria and deafness. History revealed decreased hearing since childhood but no macroscopic haematuria.
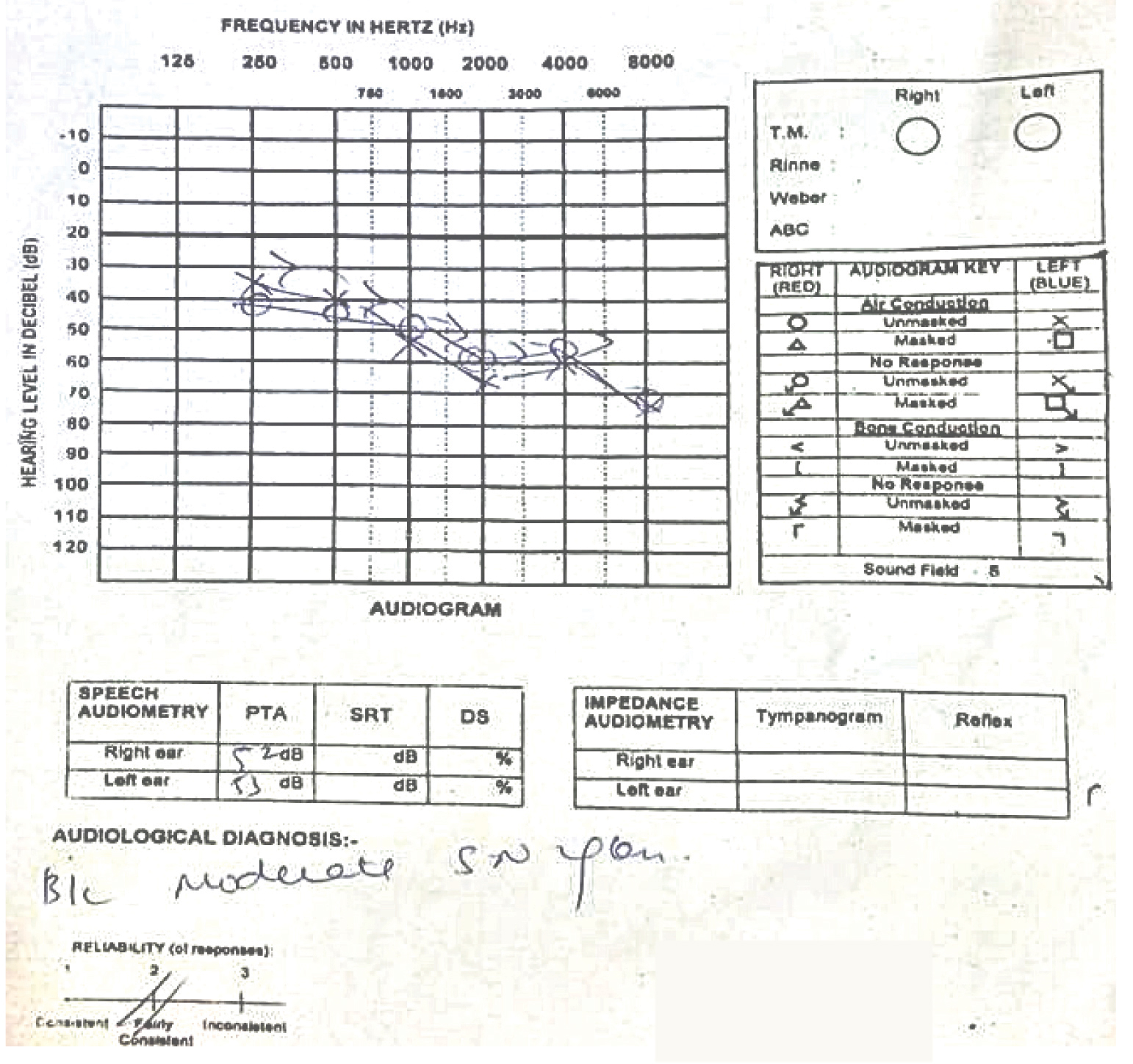
Patient was investigated accordingly, audiometry showed moderate sensorineural hearing defects both sides [Table/Fig-3]. Urine examination showed microscopic haematuria, hence, a diagnosis of Alport syndrome was made. Patient had no family history of similar complaints or haematuria. The presentation, with progressive simultaneous anterior and posterior lenticonus without any renal complaints is rare. In such cases, the lenticonus on ocular examination can help in early diagnosis of renal pathology, thus preventing complication like renal failure.
Audiometry of both ears showing moderate sensorineural hearing loss.
A clear lens extraction with intraocular lens was done in both eyes one after the other to eliminate the lenticular irregular astigmatism taking precautions during capsulorhexis. The follow-up at four weeks was uneventful with patient regaining best corrected visual acuity 6/6 in both eyes.
Discussion
Lenticonus is a cone-shaped protrusion of the anterior or posterior lens surface of the crystalline lens. Posterior lenticonus is more common than anterior lenticonus and is usually unilateral and associated with Lowe’s syndrome, whereas anterior lenticonus, which is often bilateral, may be associated with Alport syndrome. The types of ocular defects described mostly involve the lens, the retina and more rarely the cornea. The most common changes are anterior lenticonus and perimacular retinal flecks [1]. The classical Alport’s syndrome is an X linked disorder characterized by a triad of progressive haematuric, nephritis, progressive hearing loss, and ocular signs [2]. It affects at least one in 10,000 individuals. The diagnosis is imperative because of the risk of disease in other family members; also, early diagnosis and treatment delays the onset of end stage renal failure. Anterior lenticonus is present in 50% of men with X-linked transmission. In women, however X-linked transmission is not common. In contrast, with autosomal recessive inheritance, lenticonus is common in both men and women [3].
The usual presentation of lenticonus is in early middle age when the renal failure has already set in [3]. Patients have gradually progressive diminution of vision due to induced lenticular astigmatism which cannot be corrected by refraction. The diagnosis is based on ‘oil droplet sign’ on distant direct ophthalmoscopy or slit-lamp examination [4]. Other ocular features include corneal opacities; cataract; central, perimacular and peripheral coalescing fleck retinopathies, and temporal retinal thinning [5]. Rarely, posterior polymorphous corneal dystrophy, macular hole, or a maculopathy impairs vision [6].
The patients with Alport syndrome usually presents with anterior lenticonus and renal disease. Cases with both anterior and posterior lenticonus are rare presentation. Also, the presentation of visual symptoms before the onset of renal failure is very uncommon [7].
Inheritance is mainly X linked or autosomal recessive with homozygous or compound heterozygous mutations [8].
On slit lamp biomicroscopy, lenticonus is seen as protrusion of lens anteriorly towards anterior chamber or posteriorly towards vitreous. The initial symptoms are blurring of vision which cannot be corrected by refraction. Later on cataract develops near anterior and posterior poles in areas of weakness due to tiny microscopic capsular ruptures [3]. The pathogenesis of Alport syndrome is explained by loss of collagen IV α3α4α5 network in basement membranes of the eye [9].
Apart from lenticonus and haematuria associated with renal dysfunction, other ocular features like central and peripheral retinopathy also occur in Alport syndrome which aids in the confirmation of diagnosis [10]. Ocular features are less sensitive but more specific than hearing loss in Alport syndrome. In certain other inherited renal diseases and in dialysis patients, haematuria is associated with hearing loss [3].
Vedantham V et al., have reported similar case of bilateral anterior and posterior lenticonus in classical Alport’s syndrome [7]; Sukhija J et al., have also reported such a finding in the autosomal recessive variant [11]. Our case serves to illustrate the fact that both anterior and posterior lenticonus may be present simultaneously in classical Alport’s syndrome, even in the absence of corneal and retinal findings.
A careful capsulorrhexis is required during cataract surgery due to weakness of capsule as described by Sukhija J and John ME et al., [11,12].
Authors have suggested that a planned clear lens extracted is advisable in such cases before the anterior capsule ruptures spontaneously as seen in these cases [13,14]. In our case, surgery was planned because of the induced astigmatism caused by lenticonus. Careful capsulotomy was performed in both eyes and fortunately in both eyes, posterior capsule was intact and thus both surgeries went uneventful.
Conclusion
An early diagnosis of Alport syndrome can be life saving to the patient as it decreases the risk of early renal failure. Cataract surgery in such patients can be planned in clear lens to rehabilitate the patient but caution should be taken in capsulorrhexis and a pre-existing posterior capsular defect.
[1]. Govan JA, Ocular manifestations of Alport’s syndrome. A hereditary disorder of basement membranes?Br J Ophthalmol 1983 67(8):493-503. [Google Scholar]
[2]. Feingold J, Bois E, Chompret A, Broyer M, Gubler MC, Grunfeld JP, Genetic heterogeneity of Alport syndromeKidney Int 1985 27(4):672-77. [Google Scholar]
[3]. Savige J, Sheth S, Leys A, Nicholson A, Mack HG, Colville D, Ocular Features in Alport Syndrome. Pathogenesis and Clinical SignificanceClin J Am Soc Nephrol 2015 10(4):703-09. [Google Scholar]
[4]. Savige J, Colville D, Opinion: Ocular features aid the diagnosis of Alport syndromeNat Rev Nephrol 2009 5(6):356-60. [Google Scholar]
[5]. Sabates R, Krachmer JH, Weingeist TA, Ocular findings in Alport’s syndromeOphthalmologica 1983 186(4):204-10. [Google Scholar]
[6]. Grupcheva CN, Chew GS, Edwards M, Craig JP, McGhee CN, Imaging posterior polymorphous corneal dystrophy by in vivo confocal microscopyClin Experiment Ophthalmol 2001 29(4):256-59. [Google Scholar]
[7]. Vedantham V, Rajagopal J, Ratnagiri PK, Bilateral simultaneous anterior and posterior lenticonus in Alport’s syndromeIndian J Ophthalmol 2005 53(3):212-13. [Google Scholar]
[8]. Jais JP, Knebelmann B, Giatras I, De Marchi M, Rizzoni G, Renieri A, X-linked Alport syndrome: Natural history in 195 families and genotype- phenotype correlations in malesJ Am Soc Nephrol 2000 11(4):649-57. [Google Scholar]
[9]. Barker DF, Hostikka SL, Zhou J, Chow LT, Oliphant AR, Gerken SC, Identification of mutations in the COL4A5 collagen gene in Alport syndromeScience 1990 248(4960):1224-27. [Google Scholar]
[10]. Bhatnagar R, Kumar A, Pakrasi S, Alport’s syndrome-ocular manifestations and unusual featuresActa Ophthalmol (Copenh) 1990 68(3):347-49. [Google Scholar]
[11]. Sukhija J, Saini JS, Jain AK, Phacoemulsification and intraocular lens implantation in an Alport’s syndrome patient with bilateral anterior and posterior lenticonusJ Cataract Refract Surg 2003 29(9):1834-36. [Google Scholar]
[12]. John ME, Noblitt RL, Coots SD, Boleyn KL, Ballew C, Clear lens extraction and intraocular lens implantation in a patient with bilateral anterior lenticonus secondary to Alports syndromeJ Cataract Refract Surg 1994 20(6):652-55. [Google Scholar]
[13]. Gupta A, Ramesh Babi K, Sriniwasan R, Mohanty D, Clear lens extraction in Alport syndrome with combined anterior and posterior lenticonus or ruptured anterior lens capsuleJ Cataract Refract Surg 2011 37(11):2075-78. [Google Scholar]
[14]. Mohan S, Gupta P, Sahai K, Sachan SK, Phacoemulsification in rare case of Alport syndromeSemin ophthalmol 2014 24(4):196-98. [Google Scholar]