Case Report
During routine dissection for undergraduates in Melmaruvathur Adiparasakthi Institute of Medical Sciences and Research, Tamil Nadu, India, variation in the VA and Basilar Artery (BA) was identified in a 72-year-old male cadaver [Table/Fig-1].
Image showing duplicated and Hypoplastic V4 segments of Vertebral Artery (VA) and Duplicated Anterior Inferior Cerebellar Artery (AICA) on the right side.
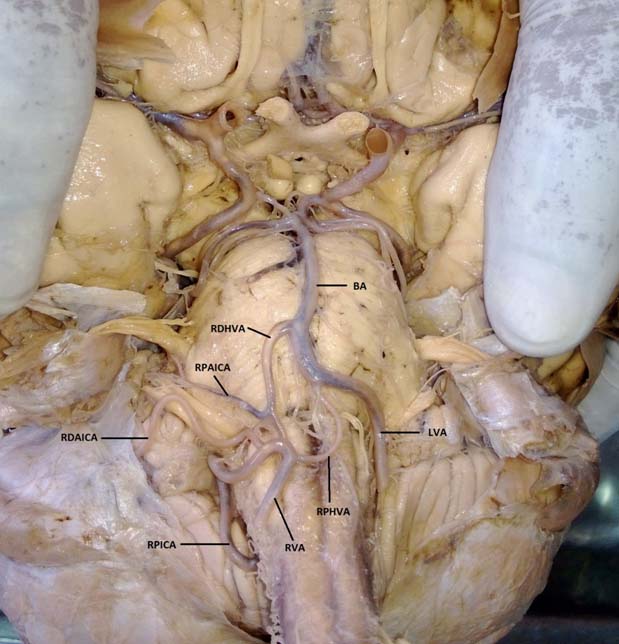
RVA: Right Vertebral Artery, RPHVA: Right Proximal Hypoplastic Vertebral Artery, RDHVA: Right Distal Hypoplastic Vertebral Artery, RPAICA: Right Proximal Anterior Inferior Cerebellar Artery, RDAICA: Right Distal Anterior Inferior Cerebellar Artery, RPICA: Right Posterior Inferior Cerebellar artery, LVA: Left Vertebral Artery, BA: Basilar Artery.
Right Vertebral Artery: The Right VA continued as right PICA. It had a sinuous course with two convex loops towards pontomedullary sulcus. Proximal loop had antero-superior convexity towards left side, at the level of medulla, ventral to right pyramid and olive. The distal loop had postero-superior convexity at right cerebello-pontine angle. Thereafter, the artery descended downwards and disappeared towards inferior vermis, dorsal to the medulla oblongata.
Branches on the right side: Three branches were emerging from the first convex loop, which were numbered as one, two and three for descriptive purpose from left to right.
First branch, the RPHVA originated from the junction of Right VA and right PICA, and followed the course of a normal VA and joined the VA of left side at the lower border of pons near the mid line. It had a very thin caliber as compared to the normal caliber of the VA. It had a sinuous course where the artery crossed the midline towards the left side and again reached the midline near the point of joining with the opposite VA.
Second branch, the RDHVA originated from the junction of right VA and right PICA, distal to the RPHVA, ascended and crossed the Ponto medullary junction to join the right border of the BA near the middle of the pons. This branch gave an offshoot towards right side at the level of ponto medullary junction called as RPAICA. RPAICA passed obliquely towards middle cerebellar peduncle above the facial and vestibulocochlear nerves and disappeared superior to flocculus of right lobe of cerebellum.
Third branch after originating from right PICA took the normal course of AICA, and is called RDAICA for descriptive purpose. It passed ventral to the facial and vestibulocochlear nerves and passed inferior to the flocculus of right lobe of cerebellum towards the cerebellopontine angle and went on to supply the anterior part of inferior surface of the cerebellum.
Left vertebral artery: This artery continued with BA from the level of ponto medullary junction. Numerous slender branches originated from the left border of the left VA which went on to supply the superior and inferior surfaces of cerebellum along with left part of pons and medulla oblongata.
Arterial Circle of Willis in normal is compared with the index case in a schematic diagram shown in [Table/Fig-2].
Comparative schematic diagram of normal arterial circle of Willis and Index case.
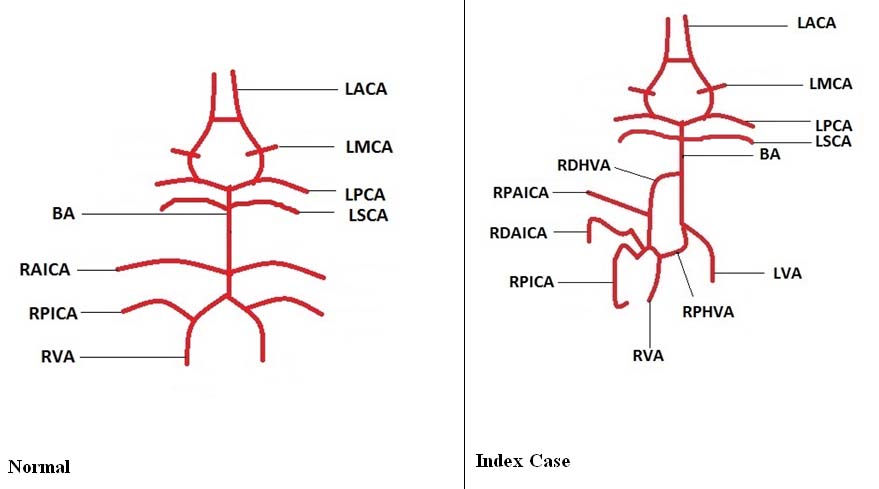
RVA: Right Vertebral Artery, RPICA: Right Posterior Inferior Cerebellar artery, RDAICA: Right Distal Anterior Inferior Cerebellar Artery, BA: Basilar Artery, LACA: Left Anterior Cerebellar Artery, LMCA: Left Middle Cerebral Artery, LSCA: Left Superior Cerebellar Artery, RPAICA: Right Proximal Anterior Inferior Cerebellar Artery, RPHVA: Right Proximal Hypoplastic Vertebral Artery, RDHVA: Right Distal Hypoplastic Vertebral Artery, LVA: Left Vertebral Artery.
Discussion
An uncommon variation of duplicated HVA is important because it may lead to acute brainstem or cerebellar ischemic stroke due to hypoperfusion; and lateralization of vestibular neuropathy [1]. Iatrogenic injury of VA during surgical procedures carries a mortality risk of 0.1% [2]. Therefore, the possibility of variations in the VA should be considered to reduce the risk of its iatrogenic injuries.
Variations, such as hypoplasia, asymmetrical configurations, and fenestrations increase the risk of vertebrobasilar ischemia and posterior circulation stroke. Hypoplastic VA was more commonly observed on the right side [3]. Narrowing and occlusion occurs at earlier age in a hypoplastic vessel as compared to normal vessel in an atherosclerotic disease [4]. In addition, malformations, injuries that affect in the perinatal period (such as basal meningitis, arteritis and arterial occlusion) or in the early childhood trauma, may impede the normal reproduction of the smooth muscle cells in the media from maintaining the capacity of the artery to grow with the brain, have been suggested in development of hypoplastic arteries [5]. Szdzuy D and Lehmann R described angiographic findings of incomplete fusion of the distal part of the BA associated with VA hypoplasia in two cases presented with symptoms of brain stem ischaemia and termed this condition as distal hypoplasia [6]. VA fenestration or partial duplication of VA was reported in seven cases out of 23 angiographic studies by Kowada M et al., [7]. Index case is different from earlier reported variations like fenestration or dolichoectasia of VA as the right VA is both hypoplastic and duplicated. An artery is said to be duplicated, if it has two origins and different course and fusion [8].
Duplication and triplication of AICA arising from BA was reported by Martin RG et al., in 26% and 2% of his cases, respectively [3]. Our case also presents duplication of AICA. However, the two arteries originated from two different sources. The RDAICA being a branch of the RPAICA from RDHVA. Such type of origin has not been reported earlier. This variation is crucial, because in any occlusion of right VA, both AICA and PICA will be affected. Under normal circumstances, any occlusion of right VA affects only right PICA.
Tokuda K et al., reported lower origin of PICA from C2 level and duplication of VA above and below C2 level. He noted that one of the limbs of duplicated VA took normal course whereas the second limb entered the spinal canal from C2 and rejoined the first limb while it ascended in the spinal canal. He also reported lower origin of PICA at C2 [9]. Machhi V et al., studied the origin and relationship of PICA with medullary and cerebellar surfaces and adjacent cranial nerves. He observed that in 42.5% of instances, PICA originated from the lateral medullary segment of the VA and in 32.5% from its premedullary segment, which is similar to the observation of the present study. After passing inferior to hypoglossal nerve, anterosuperior looping (41%) and straight course (41%) was observed in PICA, when it arises from lateral medullary segment of VA. Further, the Tonsillo Medullary (TM) and Telovelo Tonsillary (TVT) segments of PICA had inferior and superior looping, respectively [10]. However, in the present case PICA was the continuation of right VA from its anterior medullary segment, yet had a caudal loop in TM segment and a cranial loop in the TVT segment. Thus, the findings of present study are partly consistent with the findings of Macchi V et al.
Vertebral artery develops from coalescing of plexiform and longitudinal anastomotic connections from primitive dorsal aorta between cervical intersegmental arteries during 32-40th day of embryonic development. Fenestration and duplication of vertebral artery is due to persistent vertebrobasilar anastomoses after fifth week of intrauterine period [11].
Kowada M et al., elucidated that an anomalous anastomosis during embryologic development will result in fenestration or partial duplication of VA. He observed that the fenestrated VA is associated with other congenital intracranial and extracranial vascular aneurysms and malformations [7]. Tokuda K et al., explained that the arterial variations are due to malarrangement of embryonic segmental arteries [9]. Macchi V et al., described the embryological basis for anomalous origin of PICA. He observed that PICA developed from the myelencephalic plexus which progress rostrocaudally and feed the cerebellum. Variable retention of primitive lateral vertebrobasilar anastomosis in the trunk of the definitive PICA, could result in variation in the origin and course of PICA [10]. The embryological basis for the vertebral artery variations described by Macchi et al., is more suitable to explain the variation observed in the index case.
It is important to report rare variations of VA like in the index case to increase the knowledge about possible variations which helps in prevention of iatrogenic injuries to VA during surgery. Stenosis of VA is the cause of infarcts in vertebrobasilar circulation in 20-25% of the stroke cases [12].
The present case report deals with the variant V4 segment of right VA. The complete course of VA could not be observed as the variation was noted after the removal of brain from the cranial cavity.
Conclusion
Variations of V3 and V4 segments of VA are very rare. The present study reports duplication of V4 segment of right VA along with duplication of right AICA and variant origin of right PICA. Such variations are not reported in the past, which makes the present case a rare one. Knowledge of variations of VA such as duplication and hypoplasia is important for surgeries in posterior cranial fossa, radiological procedures like CT angiographies. Hypoplasia may lead to hypoperfusion and ischemic stroke of the brainstem and cerebellum.
[1]. Chuang YM, Chern CM, Liao WH, Hsu WH, Lien CF, Lirng JF, Contribution of intracranial vertebral artery asymmetry to vestibular neurpathyJ Neurol Neurosurg sychiatry 2011 82:823-25. [Google Scholar]
[2]. Iqbal S, Vertebrobasilar variants and their basic clinical implicationsInt J Med Res Health Sci 2013 2:799-808. [Google Scholar]
[3]. Martin RG, Grant JL, Peace D, Theiss D, Microsurgical relationships of the anterior inferior cerebellar artery and the facial-vestibulocochlear nerve complexNeurosurgery 1980 6:483-507. [Google Scholar]
[4]. Fischer CM, Gore I, Okabe N, White PD, Atherosclerosis of the carotid and vertebral arteries extracranial and intracranialJ Neuropathol Exp Neurol 1965 24:455-76. [Google Scholar]
[5]. Hegedus K, Hypoplasia of the basilar arteryEur Arch Psychiatr Neurol Sci 1985 234:395-98. [Google Scholar]
[6]. Szdzuy D, Lehmann R, Hypoplastic distal part of the basilar arteryNeuroradiology 1972 4:118-20. [Google Scholar]
[7]. Kowada M, Yamaguchi K, Takahashi H, Fenestration of the vertebral artery with a review of 23 cases in JapanRadiology 1972 103:343-46. [Google Scholar]
[8]. Ionete C, Omojola MF, MR angiographic demonstration of bilateral duplication of the extracranial vertebral artery: unusual course and review of the literatureAJNR Am J Neuroradiol 2006 27:1304-06. [Google Scholar]
[9]. Tokuda K, Miyasaka K, Abe H, Abe S, Takei H, Sugimoto S, Anomalous atlantoaxial portions of vertebral and posterior inferior cerebellar arteriesNeuroradiology 1985 27(5):410-13. [Google Scholar]
[10]. Macchi V, Porzionato A, Guidolin D, Parenti A, De Caro R, Morphogenesis of the posterior inferior cerebellar artery with three-dimensional reconstruction of the late embryonic vertebrobasilar systemSurg Radiol Anat SRA 2005 27:56-60. [Google Scholar]
[11]. Uchino A, Sawada A, Takase Y, Kudo S, Extreme fenestration of the right vertebral artery: magnetic resonance angiographic demonstrationEur Radiol 2002 12(Suppl 3):S32-S34. [Google Scholar]
[12]. Nouh A, Remke J, Ruland S, Ischemic posterior circulation stroke: A review of anatomy, clinical presentations, diagnosis, and current managementFront Neurol 2014 5:30-34. [Google Scholar]