Neglected Necrotizing Fasciitis - A Rare Complication of Spinal Anaesthesia
Karikal Chakaravarthi1, Ashish Gupta2, Lileswar Kaman3
1 Senior Resident, Department of General Surgery, ESI Hospital, Bengaluru, Karnataka, India.
2 Senior Medical Officer, Department of General Surgery, PGIMER, Chandigarh, India.
3 Professor, Department of General Surgery, PGIMER, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lileswar Kaman, Professor, Department of General Surgery, Pgimer, Chandigarh-160012, India.
E-mail: drashish0403@yahoo.in
Necrotizing Fasciitis (NF) is a rare, rapidly progressive severe bacterial soft tissue infection with a high mortality rate. NF classically involves the trunk, groin/perineum, lower limbs, and postoperative wound sites. NF secondary to spinal anaesthesia in a young postpartum female is extremely rare. Here we are describing a young postpartum female who underwent cesarean section for the delivery of child but developed NF of the back starting from the site of spinal needle insertion. She was referred to our center after 21 days of surgery with extensive NF. She underwent serial debridement but succumbed to septic shock secondary to gram negative and fungal sepsis.
Caesarean section, Gram negative sepsis, Spinal anaesthesia
CASE-REPORT
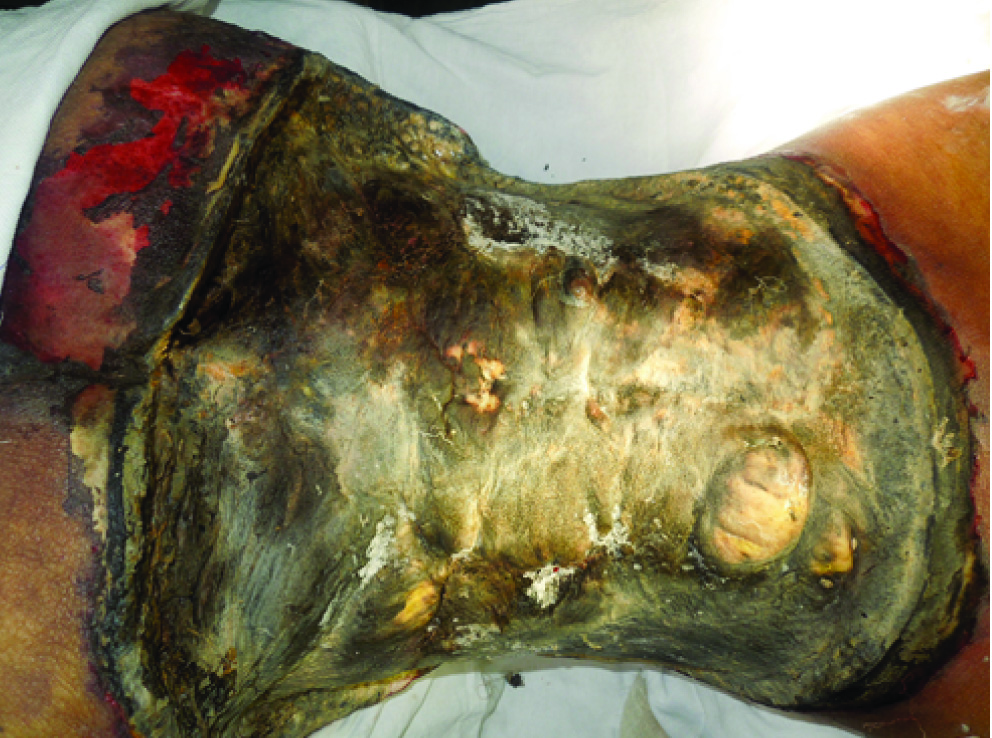
A 27-year-old female came to our emergency department with blackening involving nearly whole of the back, part of anterior abdomen and gluteal regions. The patient underwent caesarean section at term in another hospital under spinal anaesthesia. On postoperative day four, blisters and erythema were noted in the area of spinal block, for which she underwent debridement and intravenous antibiotics were started. After a management of 21 days with antibiotics and serial debridement she was referred to our center. Patient presented to us with extensive blackening and necrosis of the back extending upto bilateral mid axillary lines and bilateral gluteal region with purulent discharge from the wound [Table/Fig-1].
Preoperative picture of the patient with necrotizing fasciitis of the back.
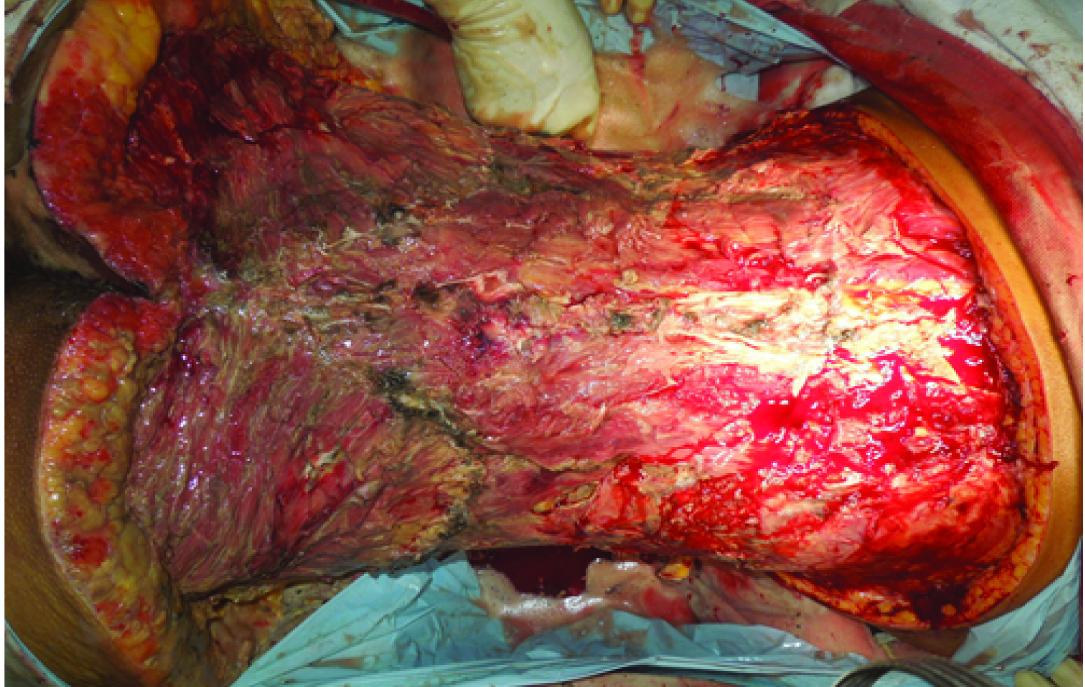
She had no history of fever or chills. Patient was not a known case of any immunosuppressive disease like HIV, diabetes mellitus or tuberculosis. There was history of administration of NSAIDS like diclofenac sodium that was administered as deep intramuscular injections in left gluteal region post cesarean. At the time of admission patient had a pulse rate of 120 beats/min and blood pressure 100/60 mmHg without any inotropic support. Laboratory investigations revealed increased total leukocyte count-42,000 cells/dl and de-arranged coagulation Prothrombin time index-44%. Serum electrolytes and renal function test were within normal limits. With LRINEC score (Laboratoty Risk Indicator For Necrotizing Fasciitis) of 9 this patient was taken to operating room after optimisation. On first-sitting she was debrided superiorly upto ninth thoracic vertebrae, inferiorly upto gluteal cleft and laterally upto bilateral anterior axillary lines. The muscle was unhealthy. All the necrosed and infected tissue was removed [Table/Fig-2].
Post debridement photograph of the same patient.
Postoperatively patient had fever, metabolic acidosis and persistent elevation of leukocyte count. She also had new onset septic encephalopathy. Blood culture grew E.coli and candida. Urine culture was sterile. Intra-operative tissue culture grew mucor and patient was started on Amphotericin B. This patient continued to deteriorate and she had progression of the necrosis on the margins of the wound despite all the measures. Patient was taken for second session of debridement. Patient continued to worsen and there was onset of septic shock. This female developed multiple organ dysfunction syndrome over a period of few days. Inspite of all these measures patient succumbed to her illness secondary to gram negative as well as fungal sepsis.
Discussion
NF is rapidly progressing infection of the skin and soft tissue [1]. It carries a mortality rate between 8.7-76% [2,3]. Mortality is high when this infection is associated with delayed treatment and immune compromised host [4]. Early diagnosis and prompt treatment offers the only chance of cure. NF secondary to various inciting aetiologies have been reported in literature, but there are few cases of NF secondary to a spinal anaesthesia for a cesarean section [5-7]. This rare and possibly avoidable complication of spinal anesthesia makes this case a unique presentation. It also provides the insight to the young anaesthesiologists and surgeons about the lethal complications of a routinely performed procedure.
NF has been classified according to the microbial infestation of the necrotic wound. Type I NF is caused by polymicrobials including the anaerobes. Whereas Type II is caused by monomicrobials commonly by group A streptococcus [8,9]. A Type III NF caused by gram negative bacilli of vibrio species has been described. Fungal infections caused by candida especially in cases of trauma and immunocompromised individuals are classified as type IV NF. Type I is the most common (70-80%) NF [9].
NF can lead to gross morbidity and mortality upto 76% if left untreated [2,3]. NF occurs more frequently in patients suffering from diabetes, alcohol addiction, immunosuppressive diseases and intravenous drug addiction [1]. However, we could not identify any of these risk factors in our patient. NF can be diagnosed in its early phase. Typically, patients with a predisposing factor and history of minimal trauma begin to have unexplained severe and continuous pain with paucity of the clinical signs [10].
So far three cases of NF after spinal anaesthesia have been reported in literature [Table/Fig-3].
Table representing the reports of the similar cases.
| Study | Treatment | Outcome |
|---|
| Singh RK and Dutta G [5] | Debridment with antibiotic therapy | Expired |
| Agarwal A et al. [6] | Debridment with antibiotic therapy | Expired |
| Kundra S et al. [7] | Debridment with antibiotic therapy | Survived |
All the cases were reported from India. One patient survived after three sitting of debridement and other two patients succumbed to septic shock. Infected vials and syringes of the local anaesthetic drug, commensals of the skin of the patient as well as the nasopharyngeal organisms of the operating suite staff are the proposed mechanisms of infection post spinal anaesthesia. Prolong hospital stay with delay in the debridement leads to poor outcome. Our patient also had E. Coli infection as reported in the previous cases [5-7].
LRINEC score as proposed by Wong CH et al., helps to screen the patients with soft tissue infection. It takes C-Reactive Protein (CRP), haemoglobin, Total Leucocyte counts (TLC), serum sodium, creatinine and blood glucose into consideration [11]. A score of more than 6 should raise the suspicion of necrotizing infections while the score of more than 8 has high predictive value of 92%. Our patient had a score of 9 at the time of presentation to our centre, so she definitely had NF with dismal prognosis.
Early diagnosis and prompt treatment of NF gives best results. Surgical debridement with antibiotics is pillars of the therapy [4]. Use of hyperbaric oxygen has also been shown to improve wound healing and reduce mortality.
The stress of the postpartum state as well as reduced ability of the body to combat the pathogens put females at risk of these infections. The role of NSAIDS like diclofenac sodium has been implicated to cause NF in postoperative patients. Diclofenac cause reduced activity of macrophages and activated T cells. It also reduces the lipopolysacchride induced IL2 production and macrophage migration leading onto decreased immunological activity. All these factors may be a possible cause of this dreaded infection in index patient [12].
Conclusion
NF is a challenging and potentially lethal disease. Early diagnosis and aggressive multidisciplinary treatment is mandatory. Such rare complications can be avoided by observing strict aseptic precautions while giving regional anaesthesia.
[1]. Catena F, La Donna M, Ansaloni L, Agrusti S, Taffurelli M, Necrotizing fasciitis: A dramatic surgical emergencyEur J Emerg Med 2004 11:44-48. [Google Scholar]
[2]. Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A, Current concepts in the management Of necrotizing fasciitisFront Surg 2014 1:36 [Google Scholar]
[3]. Anaya DA, Dellinger EP, Necrotizing soft -tissue infection: diagnosis and managementClin Infect Dis 2007 44:705-10. [Google Scholar]
[4]. Stephensen H, Dotters DJ, Katz V, Droegemueller W, Necrotizing fasciitis of the vulvaAm J Obstet Gynecol 1992 166:1324-27. [Google Scholar]
[5]. Singh RK, Dutta G, Fatal necrotising fasciitis after spinal anaesthesiaJ Cutan Aesthet Surg 2013 6(3):165-66. [Google Scholar]
[6]. Agarwal A, Babu MS, Verma M, Agarwal S, A rare case of necrotising fasciitis after spinal anaesthesiaIndian J Anaesth 2013 57(3):316-18. [Google Scholar]
[7]. Kundra S, Singh RM, Grewal A, Gupta V, Chaudhary AK, Necrotizing fasciitis after spinal anesthesiaActa Anaesthesiol Scand 2013 57:257-61. [Google Scholar]
[8]. Vijayakumar A, Pullagura R, Thimmappa D, Necrotizing fasciitis: diagnostic challenges and current practicesISRN Infectious Diseases 2014 2014:208072 [Google Scholar]
[9]. Morgan MS, Diagnosis and management of necrotising fasciitis: a multiparametric approachJournal of Hospital Infection 2010 75(4):249-57. [Google Scholar]
[10]. Bisno AL, Cockerill FR, Bermudez CT, The initial outpatient physician encounter in group A streptococcal necrotizing fasciitisClin Infect Dis 2000 31:607-08. [Google Scholar]
[11]. Wong CH, Khin LW, Heng KS, Tan KC, Low CO, The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infectionsCritical care medicine 2004 32(7):1535-41. [Google Scholar]
[12]. Villalonga N, David M, Bielaska J, González T, Parra D, Soler C, Immunomodulatory effects of diclofenac in leukocytes through the targeting of Kv13 voltage-dependent potassium channelsBiochemical pharmacology 2010 80(6):858-66. [Google Scholar]