Introduction
Periodontal disease owing to its inherent characteristics is traditionally measured using surrogate markers like Probing Pocket Depth (PPD) and Clinical Attachment Level (CAL). Traditionally therapeutic success was determined by the positive change in the patient’s clinical, physiological, radiological or biochemical parameters brought about by the treatment. In the modern day medical and dental practice, patient assumes a more active central role in decision making and treatment planning. Patient’s opinion, therefore is a fundamental measure of therapeutic success along with the various traditional markers. As the patient is the primary beneficiary of the treatment, there is a need to recognize and value the patient’s perception of change in response to treatment. The patients opinion about their health status is not only increasingly recognized in clinical practice but also being incorporated as an outcome measure in clinical epidemiology as well as in controlled clinical trials [1,2]. It was Cohen LK and Jago JD who reported for the first time, the development of patient based measures for the assessment of oral health [3]. Ever since, development and application of tools for the self-assessment of oral disease outcomes or PROs has grown remarkably over the years. The PROs are used as an umbrella term and include not only measures of subjective symptoms, but assessment of treatment satisfaction and also Health-Related Quality Of Life (HRQoL). Eisenberg HS and Goldenburg IS in 1966 first reported the use of patient’s subjective opinion as a measure in comparing the effects of treatment approaches in breast cancer surgery [4]. In this study, the quality of survival after radical mastectomy was compared to limited surgery using a questionnaire to evaluate patient’s attitude. Later USFDA [5] instructed to include the patients’QoL data as one of the key efficacy parameters in clinical trials for new anticancer agents. This decision has popularized PROs as an essential outcome variable in clinical trials. In 1986 the New England Journal of Medicine published a Randomized Controlled Trial (RCT) comparing antihypertensive drugs which used patients’ self-assessment of QoL as primary outcome measure [6]. In 2002, Somerman MJ stated that research on the regeneration of oro-craniofacial tissues (including periodontal tissues) needs to consider subjective, PRO factors when designing such therapies [7]. USFDA has defined PROs as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patients’ response by a clinician or anyone else” [5]. The term Patient Based Outcome (PBO) has been used by certain investigators pertaining to periodontal disease [2,8]. The aim of the present review was to evaluate whether surgical or NSPT has an effect on OHRQoL based on available literature.
What and How of PROs: PROs are data obtained directly from the patient over telephone, via email, by personal interview or by self-administered questionnaire. PRO has to be administered by an independent agent other than the treating periodontist or the person taking clinical measurements. Computerized assessments or questions administered by staff members who are not involved in the patient’s treatment may yield more accurate measurements. A typical PRO instrument is a set of questions or statements and each question or statement is known as an item [5]. There may be multiple items under several domains in an instrument. The patient’s response will be in Visual Analog Scale (VAS) or Likert like scale format which can be quantified as a particular total score for an individual. The items in a PRO instrument should match the context of use like nature of treatment, patients or population in which it is applied, and the objective of assessment. In other words, the PRO measure [Table/Fig-1] has to be specific to the treatment or intervention to be studied to obtain desired results. For example a PRO instrument that compares two surgical techniques for root coverage should include items on postoperative pain and discomfort, presence of donor site and associated morbidity, aesthetics, well-being and satisfaction. Pain and sensitivity are common symptoms associated with periodontal therapy. Treatment experiences like pain need to be recorded in near real time as patients tend to forget the intensity of pain over time [9]. A delay in getting such data may lead to bias in comparative clinical trials. PRO measures provide scores based upon patients opinion, which gives a clear picture about his or her health or illness. PROs are useful not only for clinicians and researchers but also for patients themselves, their family members, healthcare providers, regulatory authorities and researchers.
Ideal qualities of PRO measures [40].
| A PRO measure should1) Be free from error or reliable2) Measure what they are intended to measure or valid3) Be sensitive to changes in the patient’s condition or be able to detect treatment differences and4) Be interpretable or clinically meaningful. |
Relevance of PRO in periodontal therapy: Treatment of periodontitis is challenging because of the complexity of the condition, lack of complete understanding of the best disease control method and the need for a determined hygiene care from the patient. Assessment of therapeutic success by traditional ways therefore is inappropriate. Though the advancement in diagnostic techniques allows the clinician or researcher to measure the clinical, symptomatic and biochemical aspects after periodontal therapy, some critical patient related aspects still remain undetected. Certain data such as impact on physical functions like chewing, smiling and speech, cognitive functioning, satisfaction with treatment, psychological and social well-being and changes in OHRQoL with treatment can be obtained only from the patients self-report. Studies have shown that periodontal disease negatively impacts on OHRQoL [10,11]. A correlation between extent and severity of periodontal disease and poorer OHRQoL has also been reported [12,13]. Patients are aware of some periodontal health indicators such as teeth with mobility, recession in the aesthetic zone, and Bleeding On Probing (BOP) and these are highly correlated with their self-reported QoL. But there are certain silent indicators about which the patient is unaware like number of teeth with deep pockets or furcation involvements that do not correlate with their self-reported health status [14]. Therefore, PRO measurement of periodontal status related to treatment needs to be carefully assessed.
Satisfaction is a multidimensional construct about which there is little or no consensus. Patient satisfaction about periodontal therapy is one of the desirable outcomes and should be a main objective of the clinician. In the 21st century, assessment of patient satisfaction related to therapy has become pivotal; thanks to the increasing consumerism in health care. There is also a shift in practitioner-patient relationships from a medical model to a transformed interactive model [15]. PRO instruments are very effective in studying patient satisfaction to a particular treatment or technique. It is also a valuable tool in assessing the HRQoL. Certain OHRQoL tools like Oral Health Impact Profile-14 (OHIP 14) [16] and Xerostomia Related QoL Scale [17] have been used in many studies as a subjective indicator to assess oral health status. Other generic tools used as PRO measures of periodontal disease status include OHRQoL Model for Dental Hygiene [18] Child Perceptions Questionnaire (CPQ 11-14) [19] and Oral Impacts on Daily Performance (OIDP) [8]. If the context of use allows, one of these established generic scales can be used as a PRO measure. Otherwise the clinician or researcher has to develop a reliable and valid context specific PRO tool for their use. In 2003, AAP commissioned systematic review [20] on surgical therapies for the treatment of recession pointed out the lack of standardized PRO measures as a limitation of the studies reviewed. It recommended to incorporate PRO measures in future studies.
Minimally important difference (MID) and statistically significant change in OHRQoL score: Many studies evaluated the impact of periodontal therapy on PRO and most of them report statistically significant changes from baseline OHRQoL scores. But this does not guarantee the observed differences are clinically meaningful [20]. MID [21,22] denotes the smallest change in a score that can be perceived as beneficial. In MID assessment, no clinical measures are used rather it represents the smallest score or change in score that is likely to be important from the patients or clinicians perspective [22]. MID, therefore, is an important parameter in the study on the impact of periodontal therapy on PRO to determine whether the observed change in OHRQoL scores after treatment is clinically meaningful [6,7,23]. MID estimation is done by two methods- distributed based and anchor based methods [7,21,22]. Distributed based MID estimation utilizes two statistical parameters namely Effect Size (ES) and Standard Error of Measurement (SEM) [22,23]. According to Norman GR et al., MID can be assumed as 0.5 Standard Deviation (SD) of the baseline score or an ES of 0.5 [24]. Jonsson B and Ohrn K assessed MID one year after NSPT using two OHRQoL tools [23]. Therefore studies on the impact of periodontal therapy on patient centered outcomes need to estimate MID, ES or SEM along with the statistical significance in the change score of the OHRQoL tool post treatment compared to the baseline.
Materials and Methods
The review was registered with the Institutional Ethics Committee of Govt. Dental College Kottayam, Kerala, India (registration no.IEC/ M/13/2017/DCK).
Search strategy: An electronic search was done in Google, Google Scholar and Pubmed for articles in English language using the terms QoL or OHRQoL or PROs or patient centred outcome AND periodontal therapy. The search commenced on 1st September 2016 and ended on 15th December 2016. Reference sections of potential studies were also searched. Unpublished literature was not included.
Eligibility: Studies assessing OHRQoL in patients with periodontitis receiving surgical or NSPT were included. Only adults above 18 years as participants were included. Non surgical therapy include oral hygiene instructions, supra and subgingival scaling and root planning using hand or ultrasonic/piezo electric devices, antiplaque agents and local or systemic antimicrobial therapy. Surgical therapy include flap technique for pocket therapy with or without regenerative material and root coverage procedures. Change in the self reported OHRQoL score from baseline was the outcome of interest. Longitudinal studies and both controlled and non-controlled clinical trials were considered. Inclusion criteria were as follows: 1) Studies that employed one or more than one multi-item OHRQoL instrument to assess PROs related to either NSPT or surgical periodontal therapy; 2) proper case definition of ‘periodontitis/ periodontal disease’ for sample selection; 3) minimum follow up of one week after periodontal therapy.
The excluded studies are: 1) narrative reviews; 2) case reports; 3) OHRQoL reported by parents or care givers; 4) those with participant’s age below 18 years; and 5) those related to implant surgeries.
Titles/abstract screening was done by one reviewer and full text articles collected. Full text articles were independently assessed for eligibility by two reviewers. Observational studies were assessed for participant selection, case definition and outcome assessment criteria. Randomised controlled trials were screened for randomisation, allocation concealment and blinding. Both the reviewers independently analysed all full texts and agreement on eligibility for inclusion and quality assessment was arrived on discussion.
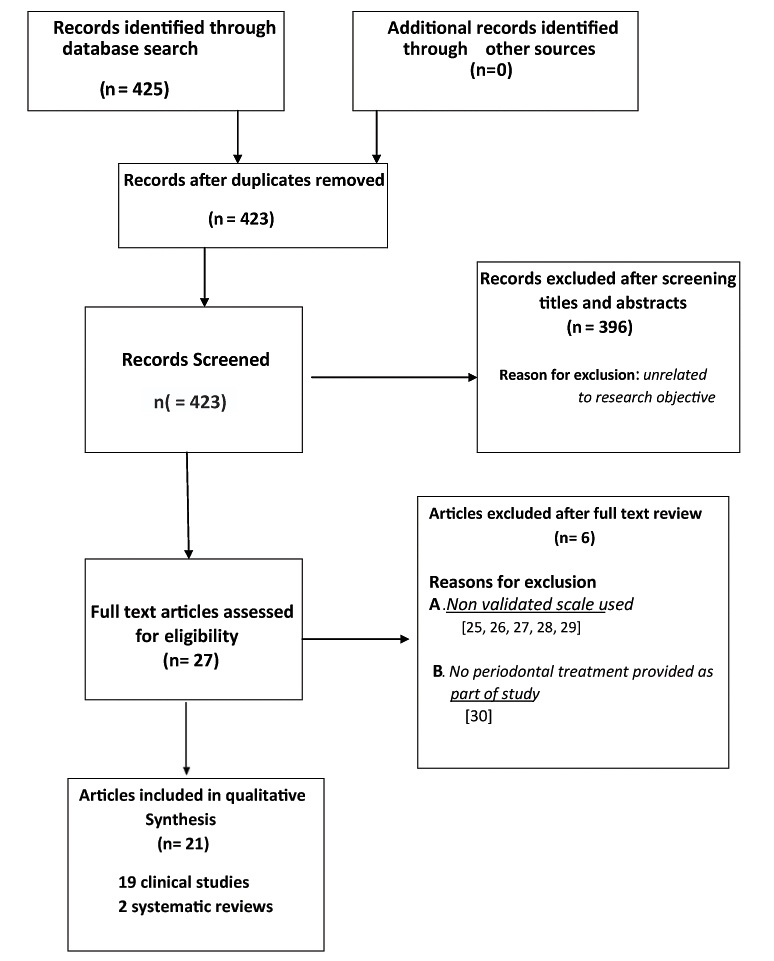
Results of the search: Initially 423 relevant articles were obtained, from which based on screening titles and abstracts 396 were excluded for not related to research objective. Full text of remaining 27 articles was retrieved. Nineteen clinical studies with 1345 participants and two systematic reviews met all the inclusion criteria. Reasons for exclusion after full text review were use of non validated QoL scale [25-29] and not providing any periodontal treatment as part of therapy [30]. Search process and study inclusion are given in [Table/Fig-2].
General characteristics of the included studies: All the included studies have defined ‘periodontitis case’ based on clinical parameters such as PD, BOP, CAL or GR. Of the 21 studies included, six were longitudinal or before after comparisons [31-36] six prospective clinical studies [1,37-41] one controlled clinical trial [42], two pilot studies [18,43], four randomised controlled trials [23,44-46] and two systematic reviews [2,47]. Eleven studies assessed the effect of NSPT on QoL [23,32-34,38,39,41-43,45,47]. Four studies compared NSPT and periodontal pocket surgery on effecting QoL changes [1,18,31,44]. Three studies investigated the role of root coverage procedures on QoL [36,37,40] and one study estimated whether Type 2 diabetes influences QoL scores in periodontally healthy and diseased subjects [35]. Four studies were from UK [32,35,43,45], three each from Brazil [40,42,46] and Japan [1,18,38], two from India [33,41] and one each from US [37] Korea [31], Turkey [44], Hong Kong [34], Germany [39] and Sweden [23]. One was a multi centre multinational study [36]. A summary of the included clinical studies is given in [Table/Fig-3].
Included PRO studies related to periodontal therapy.
| Authors/ Study design | Participants | Periodontal disease defenition | Intervention/ Comparison | OHQoL† Instrument |
|---|
| Lee JM et al., [31] Korea (Longitudinal) | 33 patients Age = 24 to 61 years | Chronic periodontitis | Modified Widman flap surgery | OHQoL† questionnaire |
| D’Avila GB et al., [42], Brazil (Contolled clinical trial) | 60 patients Age >34 years | Eight sites with a PD‡>5 mm and no deeper than 10 mm | Different NSPT§, modalities 1. SRP¶, 2. SRP¶ + Metronidazole, 3. SRP¶ + Professional, plaque removal, 4. SRP¶ +, Metronidazole + Professiona, plaque removal | OHQoL† questionnaire |
| Gamboa AB et al., [43], UK (Prospective pilot study) | 33 patients Age =20 to 60 years | Minimum of two teeth with PD‡> 4 mm | NSPT§ | Emotional intelligence questionnaire by Cooper and Sawaf |
| Ozcelik O et al., [44], Turkey (Randomised controlled trial) | 182 patients | Minimum of eight teeth with attachment loss > 5 mm At least one deep intrabony defect | 1. NSPT§ 2. ST†† 3. ST†† + EMD‡‡ | OHIP§§ – 14 GOHAI¶¶ |
| Wessel JR et al., [37] Ohio (Prospective Clinical) | 26 patients Age= 21 to 70 years | GR††† | CTG‡‡‡ vs FGG§§§ | VAS¶¶¶ |
| Aslund M et al., [45] UK (Randomised controlled trial) | 59 patients Age = 47 to 56 years | Minimum of four site with > 5 mm pockets with 2 mm attachment loss in different quadrants | NSPT§ Piezo ceramic vs Curettes | OHQoL† – UK VAS¶¶¶ SF-MPQ†††† |
| Jowett AK et al., [32] UK (Longitudinal) | 27 patients Age= 21 to 61 years | PD‡> 4 mm in atleast one sextant | 24 hour root surface debridement | OHIP§§– 14 |
| Saito A et al., [38] Japan (Prospective Clinical) | 58 patients Mean age = 53.6 | Min four sites with PD > 4 mm, Radio graphic evidence of bone loss | SRP and oral hygiene Instructions Evaluation after three weeks | OHRQL†††††† (questionnaire) |
| Shah M and Kumar S [41] India (Prospective Clinical) | 50 dentate adults Mean age = 26 and 29 years respectively in control and study groups | At least one proximal site with PD >4 mm | SRP in test group oral hygiene instructions only in control | OHIP§§ – 14 |
| Saito A et al., [18], Japan (Prospective Pilot study) | 21 patients Mean age = 56 | Moderate to severe periodontitis more than two sites with CAL‡‡‡‡>4 mm, or more than two sites with PD‡>5 mm | Phase 1 – baseline Phase 2 (NSPT§) – OHI, SRP¶ under LA. Phase 3 (ST††) – OFD§§§§ + antibiotic +NSAIDs. | OHQoL†-J (Japanese version) |
| Nagarajan S and Chandra RV [33], India (Longitudinal) | 183 patients 18–55 years | Classified into low, moderate and high-risk groups based on PRA¶¶¶¶ model | 1. NSPT§– SRP¶ 2. ST†† 3. Aggressive NSPT§–SRP¶ + local drug Delivery | OHQoL†–UK (United Kingdom version) |
| Wong RM et al., [34], Hong Kong (Longitudinal) | 65 patients 35–65 years of age | Moderate to advanced chronic periodontitis More than two sites with >5 mm PD‡ in each quadrant. | NSPT§– OHI, supra-/ sub-gingival SRP¶ | OHIP§§-4-S (questionnaire) |
| Brauchle F et al., [39] Germany (Prospective Clinical) | 93 patients Age =27-74 | Control group (PD‡< 4 mm, CPI††††† score 0–2), patients with CPI score of 3 (PD‡ = 4–5 mm) and patients with CPI††††† score of 4 (PD‡> 5 mm) | NSPT§ | OHIP§§-German version |
| Douglas de Oliviera DW et al., [40] Brazil (Prospective Clinical) | 22 patients, 25 defects 20 to 49 years of age | Miller class I or II GR‡‡‡‡‡ on maxillary canine or premolar. Presence of dentine hypersensitivity | CAF§§§§§ + CTG‡‡‡ | OHIP§§ - 14 |
| Jonsson B and Ohrn K [23] Sweden (Randomised Controlled Trial) | 87 patients 20 to 65 years of age | Moderate to advanced periodontitis | NSPT§ | GOHAI¶¶ OHQoL† - UK |
| Irani FC et al., [35] U K (Prospective) | 61 Type 2 diabetics 74 non diabetics | Grouped into healthy, gingivitis and periodontitis based on PD, bleeding and radiographic bone loss | NSPT§ comparison between diabetics and non diabetics | OHIP 49 |
| Santuchi CC et al., [46] Brazil (Randomised Controlled Trial) | 90 patients 35 to 60 years of age | Mild to moderate chronic periodontitis | SRP¶ vs One stage full mouth disinfection | OIDP¶¶¶¶¶ OHQoL† |
| Makino-Oi A et al., [1] Japan (Prospective Clinical) | 76 patients above 20years old | Two or more interproximal sites with clinical attachment ≥ 4 mm, not on the same tooth or two or more interproximal sites with probing pocket depth (PD‡) ≥ 5 mm, not on the same tooth, with radiographic evidence of bone loss | 1. Baseline 2. After initial therapy 3. After ST†† or supportive periodontal therapy | OHRQL†††††† (questionnaire) |
| Stefanini M et al., [36] Mutli national (Longitudinal) | 45 patients (90 gingival recessions) | Miller class I or II GR‡‡‡‡‡ | CAF§§§§§ vs CAF§§§§§+ CMX ‡‡‡‡‡‡ | VAS¶¶¶ |
Oral health related quality of life
Probing depth,
Non-surgical periodontal therapy,
Scaling and root planing,
Surgical therapy,
Enamel matrix derivative,
Oral Health Impact Profile,
General oral health assessment index,
Gingival recession,
Connective tissue graft,
Free gingival graft,
Visual analog scale,
Short form Mc-Gill pain questionnaire,
Clinical attachment level,
Open flap debridement,
Periodontal risk assessment,
Community periodontal index,
Gingival recession,
Coronally advanced flap,
Oral impact on daily performance,
Oral health-related quality of life model for dental hygiene,
Collagen matrix - Xenogenic
Discussion
Satisfaction to treatment after modified Widman flap surgery was assessed by Lee JM et al., in chronic periodontitis patients using PRO scale and found that satisfaction parameters related to expectation of treatment outcome decreased significantly after surgical therapy [31].
Ozcelik O et al., compared the immediate postoperative QoL of periodontitis patients after non surgical, surgical and surgical plus enamel matrix derivative treatments [44]. They report that surgery alone group experienced the worst OHRQoL in the immediate postoperative period.
Postoperative comfort after root coverage surgery was compared between connective tissue graft and Free Gingival Graft (FGG) using PRO measures and reports more discomfort and pain for FGG [37]. Douglas de Oliveria DW et al., attributes the reduction in dentinal hypersensitivity as the reason for the improvement of QoL after root coverage surgery [40]. Irrespective of the procedure used, root coverage surgery significantly improved QoL scores posttreatment [36].
Aslund M et al., supports the concept that periodontitis may negatively affect a patient’s QoL and that non surgical treatment may improve it [45]. D’Avila GB et al., and Santuchi CC et al., reported that regardless of the protocol used, non surgical periodontal treatment led to significant reduction of self perceived impacts [42,46].
Four more studies were in agreement that non-surgical therapy improves QoL in periodontitis patients [32,34,38,41]. Patients with severe periodontal disease showed better improvement in QoL after therapy when compared to those with mild or moderate disease [39]. Brauchle F et al., reported the influence of age, gender and tobacco consumption on OHRQoL [39].
One study compared the impact of periodontal surgery with that of initial therapy (non surgical therapy) on QoL [18]. Both treatments improved OHRQoL. But the QoL didn’t significantly improve in the interval between post initial therapy and after surgery. Makino-Oi A et al., also reported the positive effect of initial therapy in bringing about OHRQoL improvement compared to subsequent non surgical or surgical therapy [1].
Nagarajan S and Chandra RV et al., assessed the impact of various OHRQoL items among three risk groups based on periodontal risk assessment -PRA model and showed that in moderate and high risk groups surgical and non surgical treatment resulted in QoL improvement when compared to low risk groups [33].
Jonsson B and Ohrn K et al., reported that NSPT resulted in QoL improvements beyond the MID in 46%-50% of patients [23]. One study assessed the effect of Type 2 diabetes on OHRQoL [35]. The QoL of non diabetic patients improved after non surgical periodontal treatment significantly, but in diabetics, there was no statistically significant change on OHRQoL scores after periodontal therapy.
Two systematic reviews on the topic were obtained [2,47]. The focussed question of the systematic review by Shanbhag S et al., was “Does surgical or non surgical periodontal therapy improve the OHRQoL in adults with periodontal disease”? The results of 11 studies reviewed suggested that all forms of nonsurgical therapy can improve the OHRQoL immediately after treatment as well as at 12 months. The ES of improvement ranges from small, medium to large among the studies reviewed. The OHRQoL domains that improve after periodontal therapy are those of function, psychology and pain. Surgical therapy does not have significant additional benefit on those who have received non-surgical therapy [2].
Buset SL et al., investigated the effect of gingivitis and periodontitis on OHRQol in a recent systematic review [47]. Twenty eight studies reported a significant association between periodontal disease and QoL. Eight studies point to increasing impacts with increased disease severity. The review also included articles that assessed the effect of periodontal therapy on QoL, even though it was not the primary objective [2,18,32,38,39,45].
The results from the included studies suggested that both surgical and NSPT can potentially improve the QoL of patients. Root coverage procedures like connective tissue grafts improved OHRQoL of patients with recession irrespective of the amount of root coverage attained. Surgical therapy didn’t result in significant additional improvement in QoL scores when compared to initial therapy. Gingivitis and periodontitis are associated with reduced QoL compared to periodontal health. OHRQoL of patients with periodontal disease improved significantly after periodontal treatment. The only study on diabetic subjects suggested that Type 2 diabetes has no impact on OHRQoL [35].
Patient centred outcome assessment- advantages and disadvantages: Patients self-report is a simple, convenient and less expensive mechanism for getting primary information related to therapeutic success. However such measures are heavily influenced by their personal beliefs, cultural background, social, educational and environmental factors. They often provide contrasting assessment from those of clinically determined metrics. Generally patients are less likely to assess adequately their periodontal status than the condition of restoration or status of teeth. Therefore, the patients self-report of their periodontal health may not be corresponding to the clinically determined measures. There is enough evidence [48,49] to show that the self-reported periodontal status is less predictive and thus less reliable. Moreover, self-reported measures are subjected to participants reporting biases. But when used to assess success of periodontal therapy in a clinical and research setting, PRO measures offer several advantages. Patient-based outcomes were identified as a research priority at the 2003 World Workshop on Emerging Science in Periodontology [50]. A validated PRO measure calibrated to normative clinical indicators is highly useful [48]. In clinical research situations where full mouth periodontal examination is impractical, validated PRO instruments are useful in determining periodontal health status. A simple and accurate PRO instrument is inexpensive and highly practical in clinical trials. Thus, it can be used in resource poor settings where expense is a concern.
Limitation
The search didn’t include articles from Embase due to inaccessibility. Articles only in English language were included. Due to the heterogenicity of the variables meta analysis could not be performed.
Conclusion
Until recently, PRO have been largely neglected in periodontal therapeutic research. Studies have shown that PRO measures like treatment satisfaction and QoL are more relevant to patients than clinical changes in PPD or CAL. Evidence suggests that PRO add value to periodontal clinical practice and research. Both non surgical and surgical periodontal treatment improved OHRQoL. However, the improvement affected by surgical therapy after initial therapy is not significant. There is a need for a specific PRO scale that could potentially tap the entire dimension of the change in patients perception brought about by periodontal therapy. More longitudinal studies using scales with good responsiveness are needed to strengthen the evidence.
†Oral health related quality of life
‡Probing depth,
§Non-surgical periodontal therapy,
¶Scaling and root planing,
††Surgical therapy,
‡‡Enamel matrix derivative,
§§Oral Health Impact Profile,
¶¶General oral health assessment index,
†††Gingival recession,
‡‡‡Connective tissue graft,
§§§Free gingival graft,
¶¶¶Visual analog scale,
††††Short form Mc-Gill pain questionnaire,
‡‡‡‡Clinical attachment level,
§§§§Open flap debridement,
¶¶¶¶Periodontal risk assessment,
†††††Community periodontal index,
‡‡‡‡‡Gingival recession,
§§§§§Coronally advanced flap,
¶¶¶¶¶Oral impact on daily performance,
††††††Oral health-related quality of life model for dental hygiene,
‡‡‡‡‡‡Collagen matrix - Xenogenic
[1]. Makino-Oi A, Ishii Y, Hoshino T, Okubo N, Sugito H, Hosaka Y, Effect of periodontal surgery on oral health-related quality of life in patients who have completed initial periodontal therapyJ Periodont Res 2016 51:212-20. [Google Scholar]
[2]. Shanbhag S, Dahiya M, Croucher R, The impact of periodontal therapy on oral health-related quality of life in adults: a systematic reviewJournal of clinical periodontology 2012 39:725-35. [Google Scholar]
[3]. Cohen LK, Jago JD, Toward the formulation of sociodental indicatorsInt J Health Serv 1976 6:681-98. [Google Scholar]
[4]. Eisenberg HS, Goldenberg IS, Hayward JL, Bulbrook RD, A measurement of quality of survival of breast cancer patientsClinical evaluation in breast cancer 1966 LondonAcademic press [Google Scholar]
[5]. US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research, Center for Devices and Radiological HealthGuidance for Industry. Patient-reported outcome measures: Use in medical product development to support labeling claims 2009 Silver Spring, MDFood and Drug Administration [Google Scholar]
[6]. Croog SH, Levine S, Testa MA, Brown B, Bulpitt CJ, Jenkins CD, The effects of antihypertensive therapy on the quality of lifeN Engl J Med 1986 314:1657-64. [Google Scholar]
[7]. Somerman MJ, Inglehart MR, Bagramian RA, Quality of life and basic research in the oral health sciencesOral health-related quality of life 2002 ChicagoQuintessence:07-12. [Google Scholar]
[8]. Tsakos G, Bernabe E, D’Aiuto F, Pikhart H, Tonetti M, Sheiham A, Assessing the minimally important difference in the oral impact on daily performances index in patients treated for periodontitisJournal of Clinical Periodontology 2010 37:903-09. [Google Scholar]
[9]. McGuire MK, Scheyer ET, Gwaltney C, Commentary: incorporating patient-reported outcomes in periodontal clinical trialsJournal of Periodontology 2014 85:1313-19. [Google Scholar]
[10]. Patel RR, Richards PS, Inglehart MR, Periodontal health, quality of life, and smiling patterns--an explorationJournal of Periodontology 2008 79:224-31. [Google Scholar]
[11]. Ng SK, Leung WK, Oral health-related quality of life and periodontal statusCommunity Dentistry and Oral Epidemiology 2006 34:114-22. [Google Scholar]
[12]. Needleman I, McGrath C, Floyd P, Biddle A, Impact of oral health on the life quality of periodontal patientsJournal of Clinical Periodontology 2004 31:454-57. [Google Scholar]
[13]. Cunha-Cruz J, Hujoel PP, Kressin NR, Oral health-related quality of life of periodontal patientsJournal of Periodontal Research 2007 42:169-76. [Google Scholar]
[14]. Inglehart MR, Enhancing periodontal health through regenerative approaches: a commentary on the need for patient-reported outcomesJournal of Periodontology 2015 86:S4-57. [Google Scholar]
[15]. Newton JT, Buck DJ, Anxiety and pain measures in dentistry: a guide to their quality and applicationJournal of the American Dental Association 2000 131:1449-57. [Google Scholar]
[16]. Slade GD, Derivation and validation of a short-form oral health impact profileCommunity Dentistry and Oral Epidemiology 1997 25:284-90. [Google Scholar]
[17]. Henson BS, Inglehart MR, Eisbruch A, Ship JA, Preserved salivary output and xerostomia-related quality of life in head and neck cancer patients receiving parotid-sparing radiotherapyOral on cology 2001 37:84-93. [Google Scholar]
[18]. Saito A, Ota K, Hosaka Y, Akamatsu M, Hayakawa H, Fukaya C, Potential impact of surgical periodontal therapy on oral health-related quality of life in patients with periodontitis: a pilot studyJournal of Clinical Periodontology 2011 38:1115-21. [Google Scholar]
[19]. Tomazoni F, Zanatta FB, Tuchtenhagen S, da Rosa GN, Del Fabro JP, Ardenghi TM, Association of gingivitis with child oral health–related quality of lifeJ Periodontol 2014 85:1557-65. [Google Scholar]
[20]. Oates TW, Robinson M, Gunsolley JC, Surgical therapies for the treatment of gingival recession. A systematic reviewAnnals of Periodontology/the American Academy of Periodontology 2003 8:303-20. [Google Scholar]
[21]. Wyrwich KW, Norquist JM, Lenderking WR, Acaster S, Industry Advisory Committee of International Society for Quality of Life R. Methods for interpreting change over time in patient-reported outcome measuresQuality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation 2013 22:475-83. [Google Scholar]
[22]. Revicki D, Hays RD, Cella D, Sloan J, Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomesJournal of Clinical Epidemiology 2008 61:102-09. [Google Scholar]
[23]. Jonsson B, Ohrn K, Evaluation of the effect of non-surgical periodontal treatment on oral health-related quality of life: estimation of minimal important differences 1 year after treatmentJournal of Clinical Periodontology 2014 41:275-82. [Google Scholar]
[24]. Norman GR, Sloan JA, Wyrwich KW, Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviationMedical Care 2003 41:582-92. [Google Scholar]
[25]. Lo´pez A, Nart J, Santos A, Alca´zar J, Freixa O, Assessment of morbidity after periodontal resective surgeryJournal of Periodontology 2011 82:1563-69. [Google Scholar]
[26]. Matthews DC, McCulloch CA, Evaluating patient perceptions as short-term outcomes of periodontal treatment: a comparison of surgical and non-surgical therapyJournal of Periodontology 1993 64:990-97. [Google Scholar]
[27]. Kloostra PW, Eber RM, Wang HL, Inglehart MR, Surgical versus non-surgical periodontal treatment: psychosocial factors and treatment outcomesJournal of Periodontology 2006 77:1253-60. [Google Scholar]
[28]. Ribeiro FV, Casarin RC, Palma MA, Ju´nior FH, Sallum EA, Casati MZ, Clinical and patient-centered outcomes after minimally invasive non-surgical or surgical approaches for the treatment of intrabony defects: a randomized clinical trialJournal of Periodontology 2011 82:1256-66. [Google Scholar]
[29]. Vettore M, Quintanilha RS, Monteiro da Silva AM, Lamarca GA, Lea o AT, The influence of stress and anxiety on the response of non-surgical periodontal treatmentJournal of Clinical Periodontology 2005 32:1226-35. [Google Scholar]
[30]. Goh V, Corbet EF, Leung WK, Impact of dentine hypersensitivity on oral health related quality of life in individuals receiving supportive periodontal careJ Clin Periodontol 2016 43:595-602. [Google Scholar]
[31]. Lee JM, Song KB, Sohn HY, Jeong SH, Kwon HK, Comparison between patient expectation before and satisfaction after periodontal surgical treatmentJournal of Periodontology 2002 73:1037-42. [Google Scholar]
[32]. Jowett AK, Orr MT, Rawlinson A, Robinson PG, Psychosocial impact of periodontal disease and its treatment with 24-h root surface debridementJournal of Clinical Periodontology 2009 36:413-18. [Google Scholar]
[33]. Nagarajan S, Chandra RV, Perception of oral health related quality of life (OHQoL-UK) among periodontal risk patients before and after periodontal therapyCommunity Dental Health 2012 29:90-94. [Google Scholar]
[34]. Wong RM, Ng SK, Corbet EF, Keung Leung W, Non-surgical periodontal therapy improves oral health-related quality of lifeJournal of Clinical Periodontology 2012 39:53-61. [Google Scholar]
[35]. Irani FC, Wassal RR, Preshaw PM, Impact of periodontal status on oral health related quality of life in patients with and without diabetesJournal of Dentistry 2015 43:506-11. [Google Scholar]
[36]. Stefanini M, Jepsen K, de Sanctis M, Baldini N, Greven B, Heinz B, Patient-reported outcomes and aesthetic evaluation of root coverage procedures: a 12-month follow-up of a randomized controlled clinical trialJournal of Clinical Periodontology 2016 43:1132-41. [Google Scholar]
[37]. Wessel JR, Tatakis DN, Patient outcomes following subepithelial connective tissue graft and free gingival graft proceduresJournal of Periodontology 2008 79:425-30. [Google Scholar]
[38]. Saito A, Hosaka Y, Kikuchi M, Akamatsu M, Fukaya C, Matsumoto S, Effect of initial periodontal therapy on oral health related quality of life in patients with peiodontitis in JapanJ Periodontol 2010 81:1001-09. [Google Scholar]
[39]. Brauchle F, Noack M, Reich E, Impact of periodontal disease and periodontal therapy on oral health-related quality of lifeInternational Dental Journal 2013 63:306-11. [Google Scholar]
[40]. Douglas de Oliveira DW, Marques DP, Aguiar-Cantuaria IC, Flecha OD, Goncalves PF, Effect of surgical defect coverage on cervical dentin hypersensitivity and quality of lifeJournal of Periodontology 2013 84:768-75. [Google Scholar]
[41]. Shah M, Kumar S, Improvement of oral health related quality of life in periodontitis patients after non surgical periodontal therapyJ Int Oral Health 2011 3:15-21. [Google Scholar]
[42]. D’Avila GB, Carvalho LH, Feres-Filho EJ, Feres M, Leao A, Oral health impacts on daily living related to four different treatment protocols for chronic periodontitisJournal of Periodontology 2005 76:1751-57. [Google Scholar]
[43]. Gamboa AB, Hughes FJ, Marcenes W, The relationship between emotional intelligence and initial response to a standardized periodontal treatment: a pilot studyJournal of Clinical Periodontology 2005 32:702-07. [Google Scholar]
[44]. Ozcelik O, Haytac MC, Seydaoglu G, Immediate postoperative effects of different periodontal treatment modalities on oral health-related quality of life: a randomized clinical trialJournal of Clinical Periodontology 2007 34:788-96. [Google Scholar]
[45]. Aslund M, Suvan J, Moles DR, D’Aiuto F, Tonetti MS, Effects of two different methods of non-surgical periodontal therapy on patient perception of pain and quality of life: a randomized controlled clinical trialJournal of Periodontology 2008 79:1031-40. [Google Scholar]
[46]. Santuchi CC, Cortelli JR, Cortelli SC, Cota LO, Fonseca DC, Alencar CO, Scaling and root planing per quadrant versus one-stage full-mouth disinfection: assessment of the impact of chronic periodontitis treatment on quality of life--a clinical randomized, controlled trialJournal of Periodontology 2016 87:114-23. [Google Scholar]
[47]. Buset SL, Walter C, Friedmann A, Weiger R, Borgnakke WS, Zitzmann NU, Are periodontal diseases really silent? A systematic review of their effect on quality of lifeJ Clin Periodontol 2016 43:333-44. [Google Scholar]
[48]. Liu H, Maida CA, Spolsky VW, Shen J, Li H, Zhou X, Calibration of self-reported oral health to clinically determined standardsCommunity Dentistry And Oral Epidemiology 2010 38:527-39. [Google Scholar]
[49]. Gilbert AD, Nuttall NM, Self-reporting of periodontal health statusBritish Dental Journal 1999 186:241-44. [Google Scholar]
[50]. Newman MG, Caton JG, Gunsolley JC, The use of the evidence-based approach in a periodontal therapy contemporary science workshopAnnals of Periodontology 2003 8:1-1. [Google Scholar]