A Rare Cause of Anaemia in HIV/AIDS
Samarth Virmani1, Rama Bhat2, Raghavendra Rao3, Ruchee Khanna4, Lipisha Agarwal5
1 Undergraduate Student, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
2 Professor, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
3 Assistant Professor, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
4 Associate Professor, Department of Pathology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Undergraduate Student, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raghavendra Rao, Assistant Professor, Department of Medicine, Kasturba Medcical College, Manipal-576104, Karnataka, India
Patients living with HIV are commonly diagnosed with anaemia which can have various aetiologies. However, one of the rare causes of anaemia in such patients is Auto Immune Haemolytic Anaemia (AIHA), which is difficult to diagnose due to the absence of reticulocytosis in HIV patients. Such patients can be treated with corticosteroids which can gradually be tapered off over a period of time. The following is a case of a 52-year-old male living with HIV who was diagnosed to have AIHA and was successfully treated with steroids.
Corticosteroids, Haemolytic anaemia, Reticulocytosis
Case Report
A 52-year-old male patient, who was a known case of retroviral illness since eight years and an old case of pulmonary tuberculosis treated eight years ago, was admitted with a chief complaint of easy fatigability for three weeks duration. The patient complained of tiredness and fatigability present throughout the day. This was associated with a decrease in appetite and occasional dysphagia. The patient also complained of retrosternal chest pain present intermittently throughout the day. There was no associated history of fever, breathlessness, palpitations or abdominal pain.
On examination, the patient’s vital signs were stable. There was conjunctival pallor and no lymphadenopathy. The rest of general physical examination was normal. Systemic examination of all systems was unremarkable. Blood investigations revealed a haemoglobin of 7.2 g/dl, platelet count of 259,000 cells/ml, total leucocyte count of 5100 cells/ml, ESR of 101 mm/hour, serum urea of 34 mg/dl, serum creatinine of 1.0 mg/dl, serum sodium of 136 mmol/l and serum potassium of 4.1 mmol/l. Peripheral smear showed normocytic normochromic anaemia and red blood cells with anisocytosis, polychromasia and occasional spherocytes. Total bilirubin was 0.2 mg/dl, direct bilirubin was 0.1 mg/dl, aspartate aminotransferase was 37 IU/ml, alanine transaminase was 34 IU/ml, alkaline phosphatase was 98 IU/ml, serum albumin was 3 gm/dl and serum globulin was 5 gm/dl. Serum lactate dehydrogenase levels were elevated (417 U/l). Serum iron, total iron binding capacity and vitamin B12 levels were found to be normal. Antinuclear Antibody (ANA) and ANA profile were negative. Stool routine and microscopy was negative for opportunistic organisms (e.g., Crytosporidia, Isospora, etc.,) and occult blood.
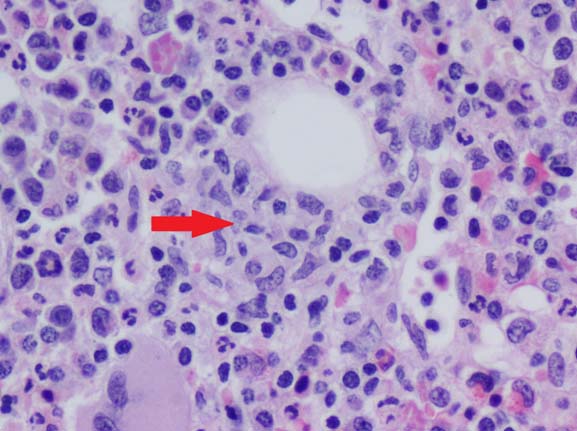
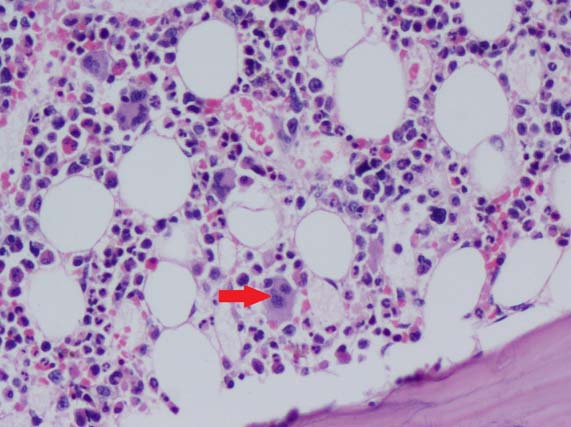
Bone marrow aspiration and biopsy were negative for acid fast bacilli and revealed HIV associated changes with increase in histiocytes [Table/Fig-1] and dyspoietic megakaryocytes [Table/Fig-2]. Glucose-6-Phosphate Dehydrogenase (G6PD) levels were found to be normal. The direct Coombs test was found to be positive. Reticulocyte count was found to be normal and reticulocyte percentage was 1.28% (normal=0.2-2.0%). The patient was diagnosed to have AIHA. The patient’s absolute CD4 count was 8 cells/μl. An esophagoscopy was done and the patient was found to have esophageal candidiasis. The patient was started on oral Itraconazole 200 mg once daily for 14 days (for esophageal candidiasis). Oral prednisolone 30 mg per day was given for four weeks, which was tapered and stopped in the next four weeks (for AIHA). Highly Active Anti-Retroviral Therapy (HAART) in the form of tenofovir, lamivudine and efavirenz was continued. The patient had come for follow up eight weeks later and was found to have a haemoglobin level of 11.2 g/dl.
Trephine biopsy showing histiocytic clusters (red arrow) (H&E staining, 40X).
Trephine biopsy showing increase in dyspoietic megakaryocytes (red arrow) (H&E staining, 40X).
Discussion
Anaemia is common among patients living with HIV and is present in about 20% of patients at the time of diagnosis and in about 70% of patients during the course of the disease [1].
Anaemia in such patients may be due to various factors such as decreased production of red blood cells due to suppression of haematopoiesis by lymphoma cells, infections like Tuberculosis (TB), disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, immune and non immune haemolysis, ineffective production secondary to vitamin B12, iron or folic acid deficiency and therapy with zidovudine which is known to suppress erythropoiesis [1].
Anaemia in patients with HIV is believed to worsen the prognosis, independent of the CD4 count, as it is associated with progression to AIDS and shorter periods of survival [2-4]. It has been shown that people living with HIV with resolved anaemia have a better prognosis than those with anaemia [5].
AIHA is a condition where anti erythrocyte autoantibodies bind to red blood cells and the reticuloendothelial system subsequently destroys these coated red blood cells [6]. The incidence of AIHA is about 1 per 75,000-80,000 population annually [7]. As per a study, the incidence of AIHA in patients with HIV was found to be 3.06% [8].
AIHA is rarely seen in patients with HIV possibly due to the difficulty in diagnosing the condition since reticulocytosis is frequently absent in AIHA in patients with HIV [9]. Our patient reticulocyte response was less than expected which may be explained by a hypo-functional bone marrow. The most preferable method of diagnosing AIHA is by the direct Coombs test, which was found to be positive in our patient.
Some cases of AIHA in HIV infected patients may occur secondary to angiotropic large cell lymphoma, Burkitt lymphoma or diffuse large B-cell lymphoma and during Castleman disease [10-13].
The first line of treatment for AIHA in HIV infected patients is corticosteroids or immunoglobulins, whereas patients who do not respond to first line treatment may be candidates for splenectomy [14]. The response to steroids is usually favorable [15]. It is important to bear in mind that such patients may have worsening of their immune status due to administration of steroids. Our patient was given oral steroids which were gradually tapered over time.
It has been shown that HIV infected patients with AIHA are at an increased risk of potentially fatal thromboembolism when they receive red blood cell transfusions, thus making it essential to screen HIV infected patients with anaemia for AIHA [16]. Moreover, most patients with the condition respond to standard treatment and those that do respond have a good prognosis, thus making screening for the condition important.
Conclusion
Autoimmune haemolytic anaemia in HIV infected patients can be difficult to diagnose due to the absence of reticulocytosis. It is important for the physician to recognise this condition and treat it because treatment of anaemia by red blood cell transfusion may prove to be detrimental for the patient. Treatment with corticosteroids is recommended, however the physician should anticipate worsening of immune status in such patients.
[1]. Lim ST, Levine AM, Hematologic aspects of human immunodeficiency syndromeWilliams Hematology 2006 McGraw- Hill Medical:1109-34. [Google Scholar]
[2]. Morfeldt-Månson L, Böttiger B, Nilsson B, Von Stedingk LV, Clinical signs and laboratory markers in predicting progression to AIDS in HIV-1 infected patientsScand J Infect Dis 1991 23:443-49. [Google Scholar]
[3]. Ellaurie M, Burns ER, Rubinstein A, Hematologic manifestations in pediatric HIV infection: Severe anaemia as a prognostic factorAm J Pediatr Hematol Oncol 1990 12:449-53. [Google Scholar]
[4]. Mocroft A, Kirk O, Barton SE, Anaemia is an independent predictive marker for clinical prognosis in HIV infected patients from across EuropeAIDS 1999 13:943-50. [Google Scholar]
[5]. Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW, Epidemiology of anaemia in human immunodeficiency virus (HIV) infected persons: Results from the multistate adult and adolescent spectrum of HIV disease surveillance projectBlood 1998 1:301-08. [Google Scholar]
[6]. Salawu L, Durosinmi MA, Autoimmune haemolytic anaemia: pattern of presentation and management outcome in a Nigerian population: a ten year experienceAfr J Med Med Sci 2002 31:97-100. [Google Scholar]
[7]. Packman CH, Haemolytic anaemia resulting from immune injuryWilliams Hematology 2006 Mcgraw-Hill Medical:729-50. [Google Scholar]
[8]. Olayemi E, Awodu OA, Bazuaye GN, Autoimmune haemolytic anaemia in HIV-infected patients: a hospital based studyAnn Afr Med 2008 7(2):72-76. [Google Scholar]
[9]. Telen MJ, Roberts KB, Bartlett JA, HIV associated autoimmune haemolytic anaemia: report of a case and review of the literatureJ Acquir Immune Defic Syndr 1990 4:1163-64. [Google Scholar]
[10]. Sukthankar AD, Bowman CA, Carey M, HIV infection with haemolytic anaemiaGenitourin Med 1997 73:66-69. [Google Scholar]
[11]. Chen M, Abedi M, Atypical lymphocytosis, cold agglutinin haemolytic anaemia, and monoclonal gammopathy in an HIV patient with marrow involvement by diffuse large B-cell lymphomaBlood 2013 122:3711 [Google Scholar]
[12]. López Dupla JM, Rodríguez Pӑrez A, Martínez Martínez P, Haemolytic anaemia due to cold-reacting antibodies: association with human immunodeficiency virus infection and non-Hodgkin’s lymphomaMed Clin 1992 98:502-04. [Google Scholar]
[13]. Gopal S, Liomba NG, Montgomery ND, Characteristics and survival for HIV-associated multicentric Castleman disease in MalawiJ Int AIDS Soc 2015 18:20122 [Google Scholar]
[14]. Oliveira LA, Oliveira BM, Murao M, Vieira ZM, Gresta LT, Viana MB, Clinical course of autoimmune haemolytic anaemia: an observantional studyJ Pediatr 2006 82:58-62. [Google Scholar]
[15]. Koduri PR, Singa P, Nikolinakos P, Autoimmune haemolytic anaemia in patients infected with human immunodeficiency virus-1Am J Hematol 2002 70:174-76. [Google Scholar]
[16]. Saif MW, Morse EE, Greenberg BR, HIV-associated autoimmune haemolytic anaemia complicated by pulmonary embolism following a red blood cell transfusion: a case report and review of the literatureConn Med 1998 62:67-70. [Google Scholar]