Granular Cell Tumour of the Chest Wall: FNA Diagnosis with a Review of Literature and Elaboration of Cytological Mimickers
Zeba Choudhary1, Prajwala Gupta2, Purnima Malhotra3, Minakshi Bhardwaj4, Prafull Kumar Sharma5
1 Senior Resident, Department of Pathology, Pgimer, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
2 Associate Professor, Department of Pathology, Pgimer, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
3 Specialist, Department of Pathology, Pgimer, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
4 Professor, Department of Pathology, Pgimer, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
5 Professor, Department of Dermatology, Pgimer, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prajwala Gupta, Room No.-302, 3rd Floor Opd Building, PGIMER, Dr. Ram Manohar Lohia Hospital, Babakharak Singh Marg, New Delhi-110001, India.
E-mail: zebachoudhary@gmail.com, prajwala2000@yahoo.com
Granular Cell Tumours (GCTs) are uncommon tumours which can be confused with other benign soft tissue tumours on clinical examination. Fine Needle Aspiration Cytology (FNAC) plays a significant role in their diagnosis. There are certain cytological mimickers of GCTs so a cytopathologist must be aware of its characteristic cytomorphology. These tumours can be present anywhere on the body; however, chest wall is one of the uncommon sites. We present a case of GCT present on the chest wall in an elderly male as a subcutaneous nodule. We have discussed the common cytological differential of GCTs, features of malignant GCTs along with cytomorphological and immunohistochemical features.
Lymphadenopathy, Pleomorphism, Subcutaneous nodule
Case Report
A 70-year-old male patient presented to the Dermatology OPD with a complaint of left sided anterior chest wall swelling which was gradually increasing in size since two years. On examination, the swelling was present over the anterior 5th and 6th thoracic segment. The swelling was subcutaneous, non-tender, nodular, measuring approximately 2 x 2 cm in size and was fixed to the overlying skin [Table/Fig-1]. There was no ulceration or pigmentation of the overlying skin. There was no palpable peripheral lymphadenopathy. The patient had no systemic complaint. Routine haematological and biochemical investigations were normal. A clinical diagnosis of dermatofibroma was kept. Ultrasonographic evaluation of the swelling revealed a well defined, heteroechoic lesion measuring 2.2 x 1.7 x 1.8 cm, present in the subcutaneous plane. The swelling was causing indentation of the underlying muscle; however, no direct invasion was seen in the muscle or overlying skin. FNAC of the swelling was done which yielded thick cellular aspirate. Smears were prepared and fixed in 95% ethyl alcohol and air dried and was subsequently stained with Papanicolaou and Giemsa stains respectively.
Well defined subcutaneous lesion on chest wall.

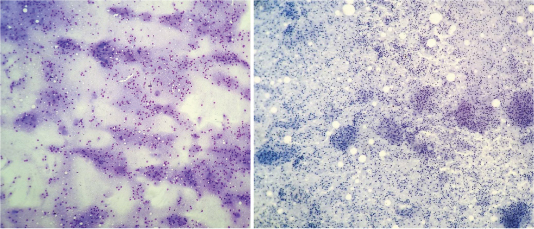
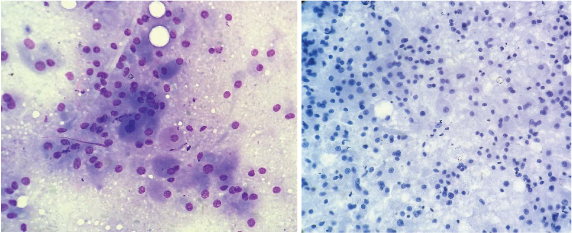
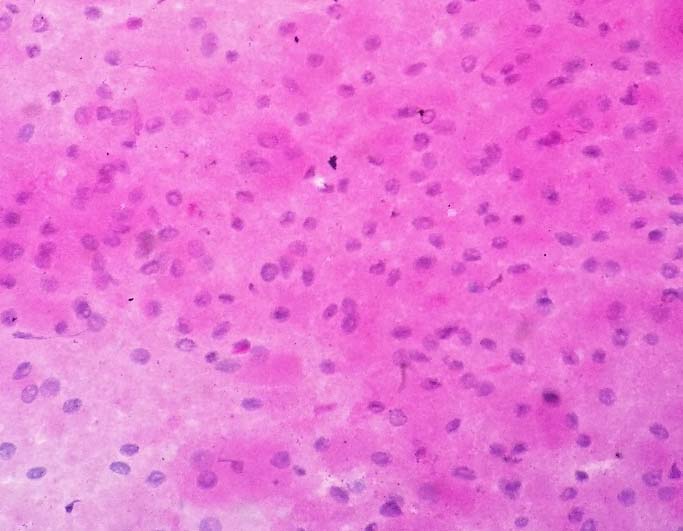
Smears were moderately cellular comprising large, polygonal cells seen as loosely dispersed clusters, sheets, syncytium and singly scattered. The cells revealed eccentric nuclei with fine nuclear chromatin, inconspicuous to prominent nucleoli and abundant granular cytoplasm and many cells showed indistinct cytoplasmic border [Table/Fig-2, 3]. No intranuclear inclusion or pseudoinclusion was seen. Few binucleate and occasional spindle shaped cells were also noted. Background revealed dispersed granular material [Table/Fig-2, 3]. No nuclear atypia, mitosis or necrosis was seen. Periodic Acid-Schiff stain with Diastase Digestion (PAS- D) was done and showed PAS positive, diastase resistant cytoplasmic granules [Table/Fig-4]. A diagnosis of benign GCT was given on FNAC and excision was advised. The excised tumour was sent for the histopathological examination.
Moderately cellular smears comprising of loosely dispersed, round to polygonal cells in a granular background (a-Giemsa stain, 10X, b-papanicolaou stain 10X.
Polygonal cells with eccentric nuclei, fine nuclear chromatin and granular cytoplasm arranged in loose clusters (a-Giemsa 40X, b-pap, 40X).
PAS positive and diastase resistant granules of granular cell tumour with PAS positive background (PAS-D, 40X).
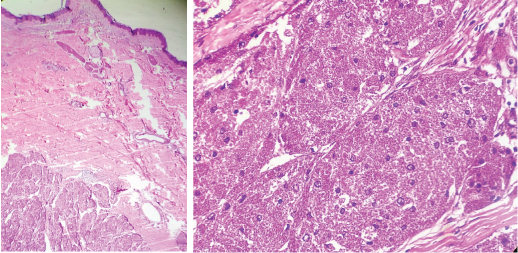
A single, circular, skin covered soft tissue piece measuring 5 x 2 x 2 cm was received in the Histopathology Department. Cut section showed a circumscribed, greyish yellow, subcutaneous nodule measuring 2.5 cm in diameter. Microscopic examination revealed a well circumscribed tumour comprising of nests and sheets of cells.
The cells were polygonal with abundant eosinophilic cytoplasm and showed round small central nuclei and vesicular chromatin. No necrosis, pleomorphism or mitosis was noted. A diagnosis of Benign GCT on the basis of histomorphology was given. Immunohistochemistry for confirmation was not performed as both the cytomorphology and histomorphology were strongly suggestive of GCT [Table/Fig-5a, b]. The patient was followed-up after a month and was found to be stable and without any recurrence of the tumour.
Granular cell tumour present in the lower dermis, comprising of benign looking tumour cells with prominent granular cytoplasm arranged in nests (H&E 10X & 40X).
Discussion
GCTs are rare tumours first reported by Abrikossoff A [1]. They account for 0.5% among soft tissue tumours and only 2% of all GCTs are malignant [2]. Most common site of this tumour is the head and neck region. Other common sites for GCT are tongue (40%), breast (15%), respiratory tract (10%) and oesophagus (2%) [3]. The aetiology of GCT is still controversial, however, the most accepted hypothesis is that it arises from Schwann cells or their precursors. Finding supporting this hypothesis is the strong and consistent positivity for S-100 [4].
These tumours primarily affect adults with a predilection for females between second to the sixth decade with a male:female ratio of 1:1.8-2.4. GCTs have characteristic cytological features which are well described in the literature; however, it often becomes difficult to differentiate it from the similar tumours with eosinophilic granular cytoplasm [5]. The GCT cells are round to polygonal with abundant amount of finely granular, eosinophilic cytoplasm, round to oval, eccentric nuclei with fine chromatin and occasionally small to inconspicuous nucleoli. These cells usually have indistinct cell membranes and often a granular background. The characteristic feature which is the cytoplasmic granularity is due to the accumulation of lysosomes. These accumulated lysosomes/autophagosomes are noted on electron microscopy along with replicated basal lamina and these granules give positive reaction to the Periodic acid-Schiff stain and CD 68 [6,7].
GCTs are usually benign tumours with malignant GCT being quite rare. Malignant GCTs present as rapidly growing tumours with size usually measuring more than 5 cm. Studies like Wieczorek TJ et al., Fanburg-Smith JS et al., and Wang J et al., have evaluated diagnostic criteria for malignant GCTs [8-10]. Three out of six features should be present to label it as malignant GCT which include necrosis, the presence of spindle cells, mitosis (>2/10 HPF), the presence of a vesicular nucleus and large nucleolus, high N:C ratio and pleomorphism. The tumour is labeled as ‘atypical GCT’ if two out of these six features are present.
The common differential diagnosis of GCT includes rhabdomyoma, Alveolar Soft Part Sarcoma (ASPS), xanthogranuloma or histiocytes rich lesions, oncocytic tumours and hibernoma. FNAC with ancillary investigations helps to resolve the diagnosis [Table/Fig-6] [6,11-15].
Common cytological mimickers of GCTs with cytomorphological and immunohistochemical features.
| Differential diagnosis | Cytomorphological features | Special stain/IHC |
|---|
| Granular cell tumour [6] | Cells with granular cytoplasm, indistinct cell borders, and eccentric nuclei arranged in syncyitium, clusters or singly scattered. | PAS + diastase resistant cytoplasmic granules S-100 + CD 68+ NSE+ CK negative |
| Rhabdomyoma [11] | Cells with well defined cell borders and ‘cross striations’ intense eosinophillic fibrillary cytoplasm | PAS + diastase sensitive Desmin+ Myoglobin+ MSA+ CK negative CD 68 negative |
| Alveolar Soft Part Sarcoma (ASPS) [12] | Frequent bi-multi-nucleate cells with granular cytoplasm showing prominent nucleoli and characteristic needle like rhombhoid crystals | PAS+ diastase resistant TFE3+ {transcriptional factor E3(strong nuclear)} S-100 negative CK negative |
| Xanthogranuloma/ histiocytes rich lesions [13] | Bean shaped nuclei of histiocytes Foamy rather than granular cytoplasm Background inflammation | PAS negative CD 68 + |
| Oncocytic tumours [14] | Central nucleus with distinct cell border, prominent nucleoli | CK+ PTAH+ (mitochondrial) PAS-D negative |
| Hibernoma [15] | Distinct cell borders with cytoplasmic multivacoulations and fatty background | S-100 + Fat stains+ CK negative |
Further, Rhabdomyoma may have characteristic radiological feature [12]. ASPS occur in children and young adults with a predilection for lower extremities, trunk, genitals and pharynx [12].
Other tumours like Extra Gastrointestinal Stromal Tumours (EGIST), Melanoma, epithelioid sarcoma and metastatic carcinoma may also come under the differential diagnosis of malignant GIST and in these cases the immunohistochemistry becomes obligatory. Epithelioid variant of EGIST may resemble GCT but these tumours are positive for CD-117(c-kit), vimentin, CD 34 and negative for CD 68, NSE and PAS. Similarly, GCT is negative for HMB-45, Melan-A/MART-1, desmin, myogenin, Myo-D 1 and cytokeratins AE1/AE3 [11-14]. In our case, the characteristic cytomorphology on FNA smears as well as the use of special stain PAS with diastase helped in reaching the correct diagnosis of GCT.
Our case is a rare case as our patient is an elderly male and the site of the tumour is chest wall which is a rare site for the Granular cell tumours and this site has been rarely reported in the literature [16].
Conclusion
The Granular cell tumours are rare tumours which can arise anywhere on the body and has a wide spectrum of cytological mimickers. A simple procedure like FNAC can accurately diagnose the lesion if the cytopathologist is aware of its characteristic cytomorphology and a simple stain like Periodic acid-Schiff can help in arriving at a correct diagnosis.
[1]. Abrikossoff A, About fibroids, emanating from the cross-strained wilful musculatureVirchows Arch Pathol Anat 1926 260:215-33.Translated from German to English language [Google Scholar]
[2]. Khansur T, Balducci L, Tavassoli M, Granular cell tumour. Clinical spectrum of the benign and malignant entityCancer 1987 60:220-22. [Google Scholar]
[3]. Liu Z, Mira JL, Vu H, Diagnosis of malignant granular cell tumour by fine needle aspiration cytology. A case reportActa Cytol 2001 45:1011-21. [Google Scholar]
[4]. Le BH, Boyer PJ, Lewis JE, Kapadia SB, Granular cell tumour: Immunohisto-chemical assessment of inhibin-alpha, protein gene product 9.5, S100 protein, CD68, and Ki-67 proliferative index with clinical correlationArch Pathol Lab Med 2004 128:771-75. [Google Scholar]
[5]. Liu K, Madden JF, Olatidoye BA, Dodd LG, Features of benign granular cell tumour on fine needle aspirationActa Cytol 1999 43:552-57. [Google Scholar]
[6]. Agarwal A, Sinha A, Rijal A, Karki S, Nizamani SM, Cytology diagnosis of granular cell tumour of umbilicus mimicking metastatic skin nodule and review of literatureMedical Channel 2010 16:103-05. [Google Scholar]
[7]. Toi P, Siddaraju N, Basu D, Fine needle aspiration cytology of granular cell tumour: A report of two casesJ Cytol 2013 30(3):195-97. [Google Scholar]
[8]. Wieczorek TJ, Krane JF, Domanski HA, Akerman M, Cytologic findings in granular cell tumours, with emphasis on the diagnosis of malignant granular cell tumour by fine needle aspiration biopsyCancer 2001 93(6):398-408. [Google Scholar]
[9]. Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG, Malignant granular cell tumour of soft tissue: Diagnostic criteria and clinicopathologic correlationAm J Surg Pathol 1998 22:779-94. [Google Scholar]
[10]. Wang J, Zhu XZ, Zhang RY, Malignant granular cell tumour: A clinicopathologic analysis of 10 cases with review of literatureZhonghua Bing Li Xue Za Zhi 2004 33:497-502. [Google Scholar]
[11]. Limbach AL, Goyal A, Adult rhabdomyoma: A challenging diagnosis on cytologyCytojournal 2012 9:20 [Google Scholar]
[12]. Folpe AL, Deyrup AT, Alveolar soft part sarcoma: A review and updateJ Clin Pathol 2006 59:1127-32. [Google Scholar]
[13]. Naresh KN, Soman CS, Granular cell tumour of the mammary skinActa Cytol 1996 40:610-12. [Google Scholar]
[14]. McCluggage WG, Sloan S, Kenny BD, Alderdice JM, Kirk SJ, Anderson NH, Fine needle aspiration cytology (FNAC) of mammary granular cell tumour: A report of three casesCytopathology 1999 10:383-89. [Google Scholar]
[15]. Lemos MM, Kindblom LG, Meis-Kindblom JM, Remotti F, Ryd W, Gunterberg B, Fine needle aspiration characteristics of hibernomaCancer 2001 93:206-10. [Google Scholar]
[16]. Park JY, Hwang JJ, Lee SA, Lee WS, Kim YH, Chee HK, Granular cell tumour occurring in the chest wall: A case reportKorean J Thorac Cardiovasc Surg 2012 45(3):196-98. [Google Scholar]