Intracranial Aneurysms Involving Circle of Willis in a Child with Human Immunodeficiency Virus Associated Vasculitis- A Rare Case Report
Amol Madanlal Lahoti1, Abhijit Kishor Taori2, Avinash Parashuram Dhok3, Jitesh Subhash Rawat4, Nihar Umakant Chandak5
1 Junior Resident, Department of Radiodignosis, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India.
2 Assistant Lecturer, Department of Radiodignosis, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India.
3 Professor and Head, Department of Radiodignosis, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India.
4 Senior Resident, Department of Radiodignosis, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India.
5 Junior Resident, Department of Surgery, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amol Madanlal Lahoti, F4/8, Vindhychal Hostel, NKP Sims and Lata Mangeshkar Hospital, Nagpur 440017, Maharashtra, India.
E-mail: amollahoti_203@yahoo.co.in
Intracranial Arterial Aneurysms (IAAs) are relatively rare in paediatric population and they account for at least 10%–15% of haemorrhagic strokes which occur during the first two decades of life. Here we present a unique and unusual case of Human Immunodeficiency Virus (HIV) infected child who presented with intracranial aneurysms with formation of collaterals and vasculopathy, demonstrating low viral count despite receiving adequate antiretroviral treatment. Intracranial vascular involvement, their complications and its incidence in these patients may become increasingly common as the management of human immunodeficiency virus infection continues to improve and afflicted patients survive for longer periods because of advancement in the antiretroviral treatment. Diagnosing aneurysm of cerebral circulation needs high degree of suspicion and correlation between clinical and radiological findings.
Collateralization, Early diagnosis, HIV, Paediatric
Case Report
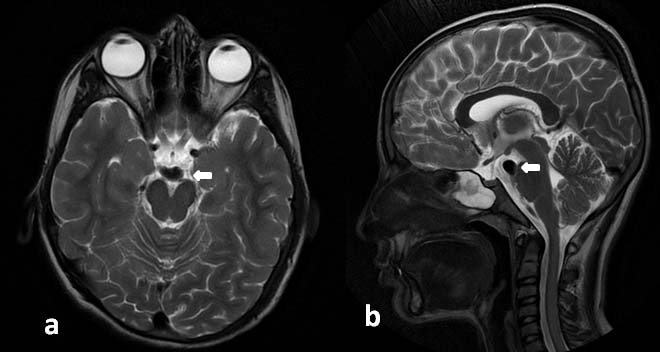
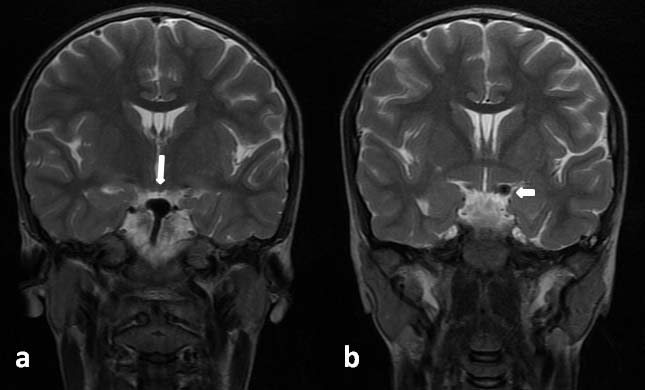
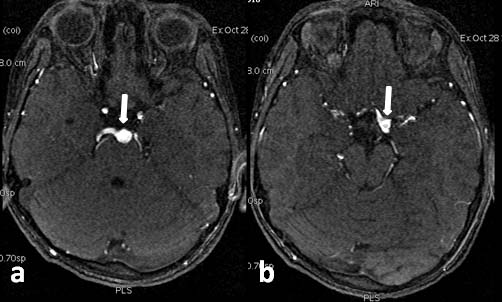
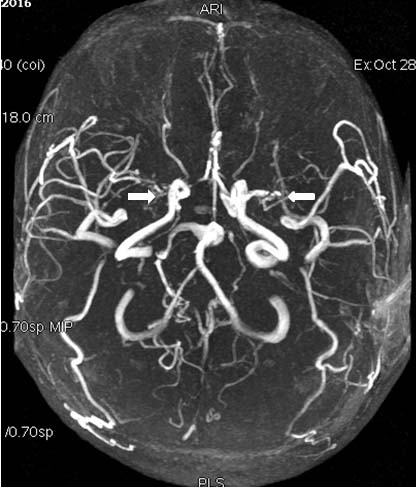
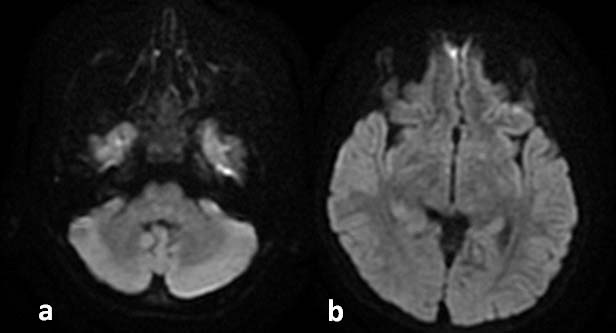
A 12-year-old male child with congenital human immunodeficiency virus/Acquired Immune Deficiency Syndrome (AIDS) was brought to the emergency department with chief complaints of partial weakness and abnormal movements of right upper and lower limb since 15 to 30 days. On admission and physical examination, he was febrile and grossly normal. Routine serological tests and blood cultures for bacteria and fungus were performed and were negative except low CD4 count. On detailed past history, it was found that, he has congenital human immunodeficiency virus syndrome/AIDS and was diagnosed with HIV in 2009. He has positive family history of diagnosed AIDS of both the parents. Two days back, he had a CD4 cell count of 21 cells/mm3, CD4 cell percentage of 2%. Patient had been compliant with several antiviral regimens. In view of abnormal body movements and partial weakness, patient was advised MRI brain and later MRI contrast angiography was done. On plain MRI brain study, fusiform aneurysmal dilatation along left lateral aspect of the basilar artery approximately 8 x 8 x 8 mm in maximal orthogonal planes, was found [Table/Fig-1]. Aneurysmal dilatation was involving basilar artery and the terminal left internal cerebral artery and its bifurcation [Table/Fig-2,3]. Irregular thickening and narrowing of bilateral middle and anterior cerebral arteries with formation of subtle collateralization were also found [Table/Fig-4]. These imaging findings may represent sequelae to immunocompromised status (HIV/AIDS) associated vasculitides and also there were small vessel ischemic changes in the form of multiple small focal areas of altered signal intensity involving cortical/sub cortical white matter in bilateral frontal, parietal and occipital lobes likely sequelae of vasculitic insult. However, there is no evidence of obvious infarct [Table/Fig-5]. On dynamic Digital Subtraction Angiography (DSA) study, above imaging findings were confirmed. Recently, he is being prescribed antiretroviral, nutritional multivitamin and multimineral supplementation. He was compliant with these medications and was asymptomatic apart from recently developed symptoms.
Magnetic resonance imaging a) Axial; b) Sagittal- T2 weighted images showing fusiform aneurysmal dilatation of the basilar artery measuring 8 x 8 x 8 mm (arrows).
Magnetic resonance imaging T2WI, coronal section showing: a) Aneurysmal dilatation of basilar artery; b) Left internal cerebral artery (arrows).
Magnetic resonance imaging, Time of Flight (TOF) angiography sequence showing: a) Aneurysmal dilatation of basilar artery; b) Left internal cerebral artery (arrows).
Magnetic resonance imaging, Time of Flight (TOF) angiography sequence showing partial obliteration of bilateral middle cerebral arteries with extensive collateralisation (arrow).
Magnetic resonance imaging, Diffusion weighted imaging, axial images does not show restriction (no evidence of ischemia).
Discussion
Cerebral aneurysms cause the most of spontaneous subarachnoid haemorrhage in children and account for more than 10% of childhood haemorrhagic stroke overall [1]. Usual vascular risk factors, which are more commonly seen in the adult population, are generally absent in the paediatric population [2]. Causes of paediatric IAAs include idiopathic aneurysms, traumatic aneurysms, and aneurysms due to excessive haemodynamic stress, vasculopathic aneurysms, infection related aneurysms, noninfectious inflammatory aneurysms, oncotic aneurysms, and familial aneurysms [2]. Observational studies have showed AIDS with an increased risk of ischemic and haemorrhagic stroke [3]. Intracranial arterial aneurysms account for as much as 57% of cases of pure spontaneous subarachnoid haemorrhage in paediatric patients [2]. Cerebrovascular complications also include haemorrhage into neoplasms, embolic phenomenon and haemorrhage associated with thrombocytopenia [4] and a rare complication, which is seen in our case, cerebral aneurysmal arteriopathy.
In patients with AIDS, infarction and haemorrhage is more commonly seen in opportunistic infections such as varicella-zoster virus, cytomegalo virus, tuberculosis, cryptococcosis and toxoplasmosis as compared to cerebral vasculitis [4,5]. Pathogenesis of vasculitis results from different mechanisms which include endothelial cell infection, immune complex deposition, and impaired regulation of cytokines and adhesion molecules [6]. Now it is known that human immunodeficiency virus infects endothelial cells of the cerebral vasculature, leading to endothelial dysfunction [5]. Human immune deficiency virus-associated cerebral aneurysmal arteriopathy has been described in several case reports and case studies in the paediatric medical literature [7]. Central nervous system vasculopathy in human immunodeficiency virus positive children is rare but more common than that in the general paediatric population. Exact incidence is not mentioned in literature. Incidence of vasculopathy among human immune deficiency virus positive subjects was 3.4 cases per 10,000 person/years [8]. Multiple intracranial arterial aneurysms are rare in young children except who have acquired (secondary to immune deficiency states) or congenital cerebral aneurysmal arteriopathy or cases of infectious intracranial arterial aneurysms [2].
The paediatric cases have featured diffuse fusiform aneurysmal dilatation in the large arteries of the circle of Willis [7] as seen in our case. In reported cases in literature of paediatric cerebral aneurysmal arteriopathy, the patients were typically of age group 8–13 years and they had advanced human immune deficiency virus disease, all meeting the criteria for acquired immune deficiency syndrome. Aneurysms of the basilar artery terminus, which are the most common posterior circulation IAA in older patients, are unusual in paediatric patients [2]. Aneurysmal dilatation of the arteries of circle of Willis and thickening of arterial walls were found in autopsy studies of children with known acquired immune deficiency syndrome and pathology revealed medial fibrosis, destruction of internal elastic lamina, loss of muscularis and intimal layer hyperplasia [9]. Intracranial aneurysmal arteriopathy is very less common even in children infected with human immunodeficiency virus and that to causing fusiform aneurysmal dilatation of the basilar artery, internal cerebral artery and its bifurcation. Aneurysmal dilatation of vessels of posterior circulation with collateral formation and with features of vasculitis without obvious neurodeficit and no evidence of subarachnoid haemorrhage or stroke. Patient is presenting with features of partial weakness but without any imaging features of infarction/haemorrhage. Thus, if such cases are diagnosed early and treated with proper antiretroviral drug therapy and then life threatening complications can be prevented. In our patient, non-human immunodeficiency virus infectious aetiologies and autoimmune diseases were excluded by detailed clinical history, serologic tests. Human immune deficiency virus associated cerebral aneurysmal arteriopathy should be considered in the differential diagnosis with acquired immune deficiency syndrome who present with signs and symptoms consistent with weakness, intracranial haemorrhage or stroke. Children usually have a latent period of around 2–11 years after initial human immunodeficiency virus infection. Aneurysmal arteriopathy occurs 2.5 years or longer after the diagnosis of acquired immune deficiency syndrome in these patients [9]. Similar findings as reported by few researchers were also noted in our case but with complications associated with aneurysmal rupture was seen [10].
Early diagnosis is important because treatment with highly active antiretroviral therapy, corticosteroid and if needed with interventional techniques may stop disease progression or even induce regression of the vasculopathy and prevent further complications.
Management: Following are treatment options available to the patient: observation, endovascular therapy and surgical therapy. Patients with unruptured aneurysm recover from endovascular treatment or surgery much faster than those who suffer from subarachnoid haemorrhage which may complicate the disease course and outcome. As the risk of rupture is more so it is necessary to compare the risk against the surgical options available.
Conclusion
Diagnosing aneurysm of cerebral circulation needs high degree of suspicion, strong correlation between clinical and radiological findings. Most patients present with subarachnoid haemorrhage or stroke, but sometimes can present without these features, as in our case. From this case, “we believe and conclude that human immunodeficiency virus associated cerebral aneurysmal arteriopathy should be considered as one of the differential diagnosis for patients with acquired immune deficiency syndrome, who may or may not present with signs and symptoms consistent with intracranial haemorrhage or stroke”.
[1]. Jordan LC, Johnston SC, Wu YW, Sidney S, Fullerton HJ, The importance of cerebral aneurysms in childhood haemorrhagic strokeStroke 2009 40(2):400-05. [Google Scholar]
[2]. Aeron G, Abruzzo TA, Jones BV, Clinical and imaging features of intracranial arterial aneurysms in the pediatric populationRadiographics 2012 32(3):667-81. [Google Scholar]
[3]. Benjamin LA, Bryer A, Emsley HC, Khoo S, Solomon T, Connor MD, HIV infection and stroke: current perspectives and future directionsThe Lancet Neurology 2012 11(10):878-90. [Google Scholar]
[4]. Snider WD, Simpson DM, Nielsen S, Gold JW, Metroka CE, Posner JB, Neurological complications of acquired immune deficiency syndrome: analysis of 50 patientsAnn Neurol 1983 14(4):403-18. [Google Scholar]
[5]. O’Charoen P, Hesselink JR, Healy JF, Cerebral aneurysmal arteriopathy in an adult patient with acquired immunodeficiency syndromeAmerican Journal of Neuroradiology 2007 28(5):938-39. [Google Scholar]
[6]. Brannagan TH, Retroviral-associated vasculitis of the nervous systemNeurol Clin 1997 15(4):927-44. [Google Scholar]
[7]. Ake J, Jay C, Lowry K, Cerebral aneurysmal arteriopathy associated with HIV infection in an adultClinical Infectious Diseases 2006 43:e46-50. [Google Scholar]
[8]. Schieffelin JS, Williams PL, Djokic D, Anderson JP, Nachman S, Oleske JM, Central nervous system vasculopathy in HIV-infected children enrolled in the pediatric AIDS clinical trials group 219/219C studyJ Pediatric Infect Dis Soc 2013 2(1):50-56. [Google Scholar]
[9]. Dubrovsky T, Curless R, Scott G, Chaneles M, Post MJ, Altman N, Cerebral aneurysmal arteriopathy in childhood AIDSNeurology 1998 51(2):560-65. [Google Scholar]
[10]. Bakhaidar MG, Ahamed NA, Almekhlafi MA, Baeesa SS, De Novo intracerebral aneurysm in a child with acquired immunodeficiency syndromeNeurosciences (Riyadh) 2015 20(3):285-91. [Google Scholar]