Solid Variant of Aneurysmal Bone Cyst Masquerading as Malignancy
Ashok Singh1, Abdul Majeed2, Supriya Mallick3, Shah Alam Khan4, Asit Ranjan Mridha5
1 Assistant Professor, Department of Pathology, ANIIMS, Port Blair, Andaman and Nicobar Islands, India.
2 Senior Reisdent, Department of Orthopaedics, AIIMS, New Delhi, India.
3 Research Officer, Department of Radiotherapy, AIIMS, New Delhi, India.
4 Professor, Department of Orthopaedics, AIIMS, New Delhi, India.
5 Assistant Professor, Department of Pathology, AIIMS, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asit Ranjan Mridha, Assistant Professor, Department of Pathology, AIIMS, New Delhi, India.
E-mail: ashok128128@gmail.com
Solid Variant of Aneurysmal Bone Cyst (SVABC) is an uncommon neoplasm seen in young patients. The lesion presents clinically as well as on radiology like a malignant bone tumour. The aggressive features in most of the cases lead to a wrong diagnosis. Radiologically, it is expansile osteolytic with cortical breach being seen in many of the cases. We report two cases of SVABC which were misdiagnosed as malignant bone tumours. Both cases were seen in long bones. Radiologically both lesions were expansile, osteolytic, solid cystic, with destruction of cortex and were diagnosed as osteosarcomas. Both the cases were referred to us for further management and were subsequently diagnosed as SVABC. Being extremely rare these tumours have a high chance of getting misdiagnosed and knowledge of this entity along with close correlation with clinical, radiological and histopathological findings plays a critical role in accurately diagnosing this condition. An accurate diagnosis is of utmost importance as this changes the treatment drastically avoiding mutilating surgeries and unnecessary chemo radiotherapy.
Long bones, Malignant, Osteosarcoma, Osteoclastic giant cells, Radiology
Case 1
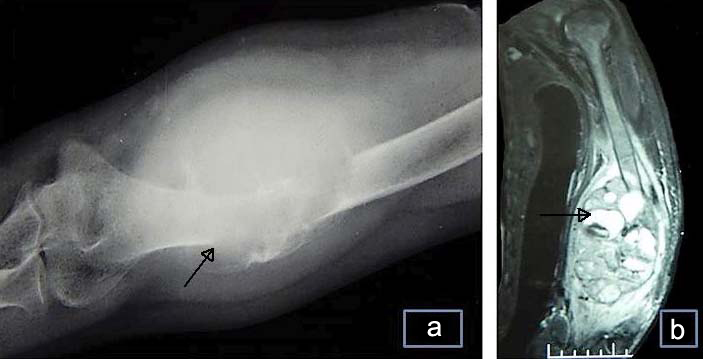
A 25-year-old female presented to orthopedic outpatient department with complaints of swelling of left distal arm for last one year and pain over distal arm for seven months. There was no history of trauma or any other swelling found in other parts of body. There was no history of weight loss or anorexia was given by the patient. On examination patient was conscious, well oriented with normal vital parameters. Systemic examination was within normal limits. The swelling was tender and measured 10x5 cm. There was no sinus or any discharge. The range of movement was restricted to 70-80 degrees, with a fixation deformity of 70 degree; however no neurovascular deficit was seen. X-ray and CT scan were done. On radiology an expansile lytic lesion [Table/Fig-1a,b] was seen with solid cystic areas and a differential diagnosis was provided favouring telangiectatic osteosarcoma over giant cell tumour of the lower end of left humerus. She underwent excision of tumour, diaphysectomy with fibular graft reconstruction. Grossly the swelling was globular and measured 13 cm. On cut section a multiloculated solid cystic lesion expanding and destroying the bone was seen [Table/Fig-2a]. The cysts contained haemorrhagic fluid and varied in size from 0.5-4.5 cm. Tumour was breaching the cortex and extending into soft tissue. On microscopic examination a solid cystic tumour was seen, solid areas showed a spindle cell proliferation with irregularly distributed osteoclastic giant cells and variable amount of stromal collagen. The stroma was oedematous and showed areas of haemorrhage at places. Reactive bone formation was also seen [Table/Fig-2b-f]. Small cystic spaces contained blood with patchy chronic inflammatory infiltrate in the surrounding stroma. No significant cellular pleomorphism, mitotic activity or any necrosis was seen. Based on radiological and histopathological findings a diagnosis of SVABC was made. Patient was on regular follow up till one year. No recurrence of lesion was seen till last follow up.
a) Radiograph shows an expansile lytic lesion (arrow) with cortical breach and extension into soft tissue; b) CT scan shows a solid tumour with fluid filled cystic areas (arrow) and solid areas destroying the cortical bone.
a) Grossly a predominantly solid tumour with multiple variable sized blood filled cysts was seen; b) Spindle cell proliferation in sheets along-with osteoid formation (H&E 10X); c) Higher magnification of another area showing numerous osteoclastic giant cells eroding the cortex; background shows haemorrhage in stroma, no mitosis or necrosis is seen (H&E 20X); d) Giant cell lesion pushing the cortical bone and thinning it (H&E 10X); e) Blood filled cyst with aggregates of osteoclastic giant cells at the periphery (H&E 10X); f) Osteopontin is non-reactive (IHC 10X).

Case 2
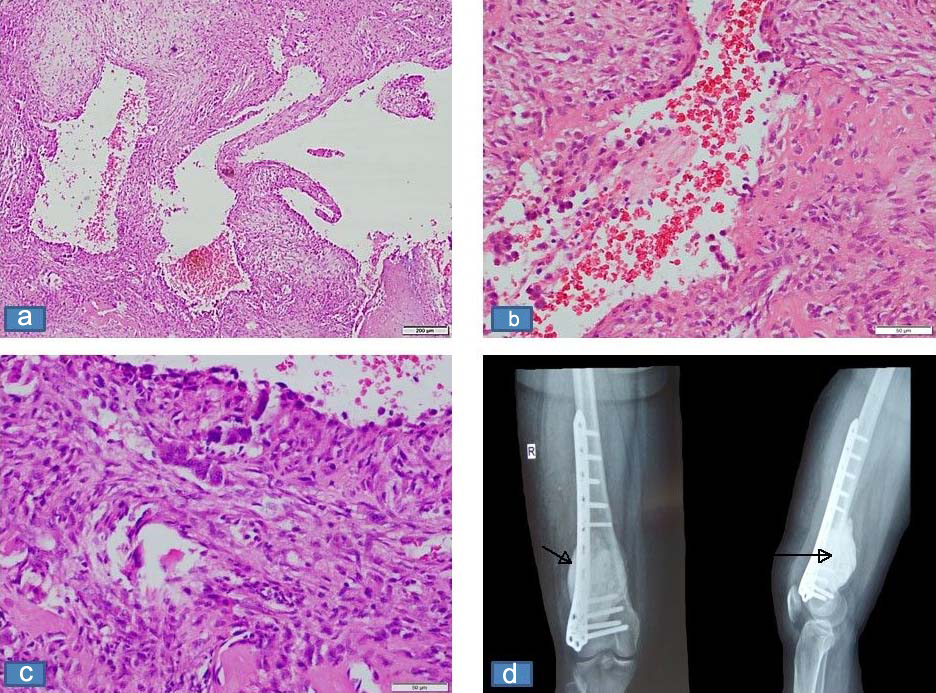
A 19-year-old female referred to the oncology department with a diagnosis of conventional osteosarcoma lower end of femur diagnosed in a different centre for further management. She presented initially with complaint of pain in right lower limb for one year. On examination, swelling was seen in the right lower thigh and knee joint region. The swelling was increasing progressively and patient was not able to bend the right knee. The skin over the swelling was stretched. No regional lymphadenopathy was seen. On X-ray a lytic mass was seen involving the lower lateral aspect of right femur. On Magnetic Resonance Imaging (MRI) scan a lesion measuring 6.4x5.9x7.8 cm was seen, it was showing focal cortical breach posteriorly however not reaching up to the articular surface of the knee joint. Biopsy blocks were submitted for histopathological examination. On microscopy a solid cystic tumour was seen. The solid lesion comprised of benign looking spindle shaped cells were seen. Interspersed cyst like spaces filled with blood were seen. The spindle cells showed little pleomorphism. No mitotic figures were seen. No malignant osteoid formation was seen. Interspersed within the spindle cells haemosiderin laden macrophages were seen. Focal aggregates of (osteoclastic) giant cells were seen in a non-uniform distribution. Based on the above features a diagnosis of solid variant of aneurysmal bone cyst was made. The patient underwent curettage with cement filling and plate arthrodesis [Table/Fig-3a-d]. Postoperative period was uneventful. The patient was on regular follow up for eight months with no recurrence of lesion was seen.
a) Microscopic section shows solid proliferation of spindle cells, cystic spaces without any endothelial lining filled with blood (H&E 10X); b) Higher magnification shows plump spindle shaped cells with minimal pleomorphism, no necrosis or mitotic activity is seen, Focally slit like spaces are also seen (H&E 20X); c) New bone formation and giant cells are also seen (H&E 20X); d) X-Ray shows an expansile lytic lesion (arrow) at the lower end of femur with cortical breach (arrow).
Discussion
SVABC is an uncommon entity accounting for <10% of aneurysmal bone cysts [1,2]. It is infrequently encountered and posing a diagnostic challenge both to the pathologists and radiologists. It was first described in the year 1983 by Sanerkin NG [3]. It comprises of solid cystic areas with presence of giant cells mimicking at times a malignant giant cell tumour of bone. It is also known as giant cell reparative granuloma of long bones and has been used interchangeably with it. SVABC is a uncommon lesion occurring mostly in head and neck region, small bones but also reported in long bones [3-7]. Rare reports in spinal location are also there [1,5,8]. The most common location in long bones being metaphyseal/diaphyseal region, many of the lesion are predominantly solid and may not show any aneurysmal areas at all [4]. Diagnosing a solid variant of aneurysmal bone cyst is very challenging as the features radiologically overlap with malignant lesions of bone notably osteosarcomas [2,4,5]. Accurate diagnosis is an absolute necessity for this as treatment approach changes drastically and salvage of the limb is possible. The mean age of diagnosis is second decade [3-5] similar to patients of aneurysmal bone cysts [4,5]. Slight female preponderance is seen. Average size of the lesion is less than 7 cm [3-5]. On histopathology solid areas comprising predominantly of fibroblastic proliferation is seen. Mitotic figures may rarely be seen in the proliferating areas. Aneurysmal sinusoids are constant finding and cyst like areas may or may not be seen. Haemorrhage is frequently seen and focal areas of osteoclastic giant cell proliferation are seen mimicking giant cell tumour of the bone [3,5-7]. Reactive osteoid formation may be seen, however in all the cases spindle cell proliferation is mostly benign looking [3,5-7]. On histopathology, the differential diagnosis includes giant cell rich lesions like giant cell tumour of bone, giant cell rich osteosarcoma and telangiectatic osteosarcoma. The notable absence of highly pleomorphic cells and malignant osteoid, rules out the osteosarcomas, the irregular distribution of giant cells and absence of neoplastic stromal proliferation rules out giant cell tumour of bone. Further the presence of aneurysmal areas filled with haemorrhagic fluid and lined by osteoclastic giant cells near the cystic areas favour diagnosis of solid variant of aneurysmal bone cyst over malignant lesions of bone [1,3-5].
Earlier thought to be a reactive recurring bone lesion but recently studies done have shown translocation and rearrangements of USP6/CDH11 and USP6/TRE7 indicating that aneurysmal bone cysts indeed are neoplastic lesions with identifiable molecular genetics [9,10].
As compared to the high recurrence rate seen in aneurysmal bone cysts of jaw and small bones solid variant of aneurysmal bone cyst has a very low recurrence rate when treated with local excision and radiotherapy [1,3-5,11].
Conclusion
SVABC is uncommon variant of aneurysmal bone cyst. It is often misdiagnosed radiologically and should always be kept in differential diagnosis on histopathology when a solid looking tumour with osteoblastic activity, fibroblastic proliferation and presence of giant cell tumour like areas are seen in a bone tumour.
[1]. Al-Shamy G, Relyea K, Adesina A, Whitehead WE, Curry DJ, Luerssen TG, Solid variant of aneurysmal bone cyst of the thoracic spine: a case reportJ Med Case Rep 2011 5:261 [Google Scholar]
[2]. Bertoni F, Bacchini P, Capanna R, Ruggieri P, Biagini R, Ferruzzi A, Solid variant of aneurysmal bone cystCancer 1993 71:729-34. [Google Scholar]
[3]. Sanerkin NG, Mott MG, Roylance J, An unusual intraosseous lesion with fibroblastic, osteoclastic, osteoblastic, aneurysmal and fibromyxoid elements. "Solid" variant of aneurysmal bone cystCancer 1983 51:2278-86. [Google Scholar]
[4]. Ilaslan H, Sundaram M, Unni KK, Solid variant of aneurysmal bone cysts in long tubular bones: giant cell reparative granulomaAm J Roentgenol 2003 180:1681-87. [Google Scholar]
[5]. Oda Y, Tsuneyoshi M, Shinohara N, "Solid" variant of aneurysmal bone cyst (extragnathic giant cell reparative granuloma) in the axial skeleton and long bones. A study of its morphologic spectrum and distinction from allied giant cell lesionsCancer 1992 70:2642-49. [Google Scholar]
[6]. Takechi R, Yanagawa T, Shinozaki T, Fukuda T, Takagishi K, Solid variant of aneurysmal bone cyst in the tibia treated with simple curettage without bone graft: a case reportWorld J Surg Oncol 2012 10:45 [Google Scholar]
[7]. Lekka JA, Gavresea TV, Stanc-Giannakopoulos GA, Demertzis NS, Solid variant of aneurysmal bone cyst of the heel: a case reportJ Med Case Rep 2011 5:145 [Google Scholar]
[8]. Gezer HÖ, Oguzkurt P, Temiz A, Demir S, Hiçsönmez A, Solid variant of aneurysmal bone cyst of the rib presenting as a left intrathoracic mass without radiological bone destructionTurk J Pediatr 2014 56:303-06. [Google Scholar]
[9]. Oliveira AM, Perez-Atayde AR, Inwards CY, Medeiros F, Derr V, Hsi BL, USP6 and CDH11 oncogenes identify the neoplastic cell in primary aneurysmal bone cysts and are absent in so-called secondary aneurysmal bone cystsAm J Pathol 2004 165:1773-80. [Google Scholar]
[10]. Ye Y, Pringle LM, Lau AW, Riquelme DN, Wang H, Jiang T, TRE17/USP6 oncogene translocated in aneurysmalbone cyst induces matrix metalloproteinase production via activation of NF-kappa BOncogene 2010 29:3619-29. [Google Scholar]
[11]. Sato K, Sugiura H, Yamamura S, Takahashi M, Nagasaka T, Fukatsu T, Solid variant of an aneurysmal bone cyst (giant cell reparative granuloma) of the 3rd lumbar vertebraNagoya J Med Sci 1996 59:159-65. [Google Scholar]