The risk of biological deterministic effects of radiation on the exposed skin increases with the effective dose and has effects ranging from an erythema, to epilation and as far as skin necrosis [1-4]. The shielding of the hands from X-ray represents a rarely used option of radiation reduction. This is difficult to realize in everyday clinical practice. The newer generation X-ray gloves are characterized by the use of lead-free material (for example bismuth oxide) and by a high flexibility. These gloves contain a metal-polymer composite, consisting of a binder (elastomer, e.g., epoxy resin), and a filler (e.g., bismuth). Bismuth is used as an alternative material because it possesses shielding properties. Due to this composition, it is possible to produce a substance which, in addition to its absorption properties, also retains its flexibility [5,6]. The new generation of radiation protection gloves is primarily made based on the requirement to use less lead and thus protect the environment from heavy metal. Bismuth metal is considered environmentally friendly, but there is limited information on the effects on the environment.
Angiographic interventions represent a high radiation exposure for the examiner, which is predominantly caused by scattered radiation [7]. The exposure can be reduced by active application of the known procedural rules of radiation protection, according to X-ray regulations, by consistently applying the protective measures (lead skirt, thyroid gland protection, protective goggles, lead lamellae at the examination table, lead glass protection, etc.) and by increasing improvement of the interventional techniques (learning curve) [8].
The purpose of this prospective study was to evaluate the use of lead-free X-ray protective gloves in clinical practice in terms of shielding and sense of touch.
Materials and Methods
The study design was a prospective single center observation made by radiologists from March 2016 to June 2016. The consent of the Institutional Review Board was obtained. For determination of the hand dose, a direct dosimeter was used. The sensor of the dosimeter was fixed at the left hand under the sterile glove during the interventional angiography procedure. In addition to the dose (in μSv), the dose rate (in μSv/s) was also determined.
Phantom Measurement
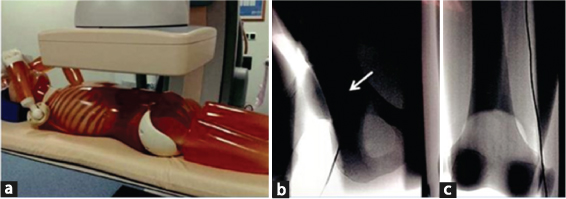
A whole-body phantom (PBU-50, Kyoto Kagaku, Japan) was used for the standardized determination of the dose values. As appropriate to usual clinical procedures, the dose was determined at the puncture site in the direct fluoroscopic X-ray beam, and at a distance of 20 cm, with and without protective gloves. A 1-min fluoroscopy was performed at a frequency of 15 per second [Table/Fig-1a-c].
Experimental setup of the phantom measurement: a) Phantom position in the angiolab; b) Imaging of the right inguinal region with the direct dosimeter afield the caput femoris (white arrow); c) Imaging of the lower limb.
Patients
A total of 50 patients (female: 23, male: 27, mean age: 74±9.8 years, 49-94 years) were examined through angiography and then angioplasty was performed. The main reason for vascular intervention was Peripheral Arterial Occlusive Disease (PAOD) (Stage II b to IV according to fontaine). The patients were randomly assigned for the study. Inclusion criteria were a PAOD with planned antegrade puncture technique.
Examiner
The examination was conducted by an experienced interventional radiologist (more than 5,000 interventions). Typical X-ray protective garments were worn, like a protective apron with 0.35 mm Pb equivalent, a thyroid protection and goggles.
Angiography
The investigations were carried out on a digital flat detector angiography system (Allura Xpert FD 20, Philips Healthcare, Da Best, Netherlands) using pulsed fluoroscopy (image frequency: 15/s). The device features automatic dosage modulation. Puncturing of the common femoral artery was performed under sterile conditions by an antegrade technique. For the preparation of serial angiograms, a contrast agent application was performed manually.
Dosimeter
According to the guidelines of the X-ray ordinance [9], officially endorsed personal dosimetry was performed under the protective apron in the area of the front of the torso. To the thermoluminescence dosimeters, a direct dosimeter (model EDD-30, Unfors Instruments, Billdal, Sweden) was used. The sensor of the direct dosimeter was fixed to the back of the left hand under the sterile glove.
Protective Glove
The sterile protective glove (Peha-shield, Paul Hartmann AG, Heidenheim, Germany) made of natural rubber has a shielding effect against X-ray diffuse radiation by the use of lead-free metal oxide. Elastic latex keeps the glove flexible. The lead equivalence value of the glove is 0.03-0.04 mm Pb. Under test conditions of the manufacturer, the attenuation of the primary radiation of 20%-25% at 80 kVp, as well as the scattered radiation of 52%-58% at 60 kVp and 42%-48% at 80 kVp is shown for the Phantom. Compared to conventional sterile gloves, the protective gloves are slightly thicker and firmer. After the intervention, an opinion of the examiner was requested for evaluation of the sense of touch. This was supposed to indicate whether there was a relevant restriction with the protective glove in relation to the pulsation of the inguinal artery and the handling of the materials.
Statistical Analysis
Statistical pretest power analysis was verified to check the required sample size for the t-test. Statistical evaluation was carried out using SPSS (version 15.0 for Windows). The data was analysed using the t-test. All values are given as a mean ± standard deviation or number of patients and percentage. A p<0.05 was considered to be statistically significant.
Results
Phantom Measurement
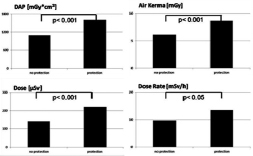
The measurements at the puncture site without a protective glove with direct radiation effects yielded an air kerma of 6.07±0.04 mGy at 58 kV and 4.7 mAs, a DAP of 1084.2±7.36 mGy*cm2. As well, the direct dosimeter showed 143±1.2 μSv and 9.73±2.63 mSv/h. With a protective glove, an air Kerma of 8.66±0.06 and a DAP of 1603.8±13.59 was measured. With the direct dosimeter 221.75±1.21 μSv and 13.48±0.08 mSv/h at 62 kV and 5.5 mAs were observed. In comparison with and without a protective glove, there was a highly significant difference with respect to Air Kerma (p<0.001), DAP (p<0.001), and μSv (p<0.001) [Table/Fig-2].
Phantom measurements: Direct radiation. t-test analysis. Comparing the dose values with and without a protection glove. Significant increase of the dose area product was observed with the protection device: 1084.2 to 1603 mGy*cm2 (p<0.001). Furthermore, the dose on the examiner’s hand showed an increase with the protection device: 143 to 221.8 μSv (p<0.001). In the direct X-ray beam, there was a significant increase of the radiation exposure both for the patient and the examiner.
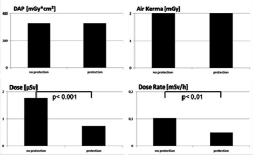
The measurements in the periphery (scattered radiation) with and without a protective glove resulted in a dose autoregulation up to 48 kV and 3 mAs. For both, an Air Kerma of 2.01±0.03 mGy and a DAP of 325.7±2.1 mGy*cm2 were found. Differences could be determined for the dose and dose rate with the direct dosimeter: Without protective glove 1.76±0.05 μSv and 0.1±0.02 mSv/h; with protective glove 0.75±0.07 μSv and 0.05±0.002 mSv/h. In comparison, there was a very significant difference in relation to the dose (p<0.001). With respect to the dose rate, a very significant difference could be determined (p<0.01) [Table/Fig-3].
Phantom measurements: Scattered radiation. t-test analysis. Comparing the dose values with and without a protection glove. There is a significant decrease of the radiation exposure for the examiner: Dose 1.76 to 0.75 μSv (p<0.001).
Examiner Measurement
The mean body mass index of the exanimated patients for the groups had no significant difference: With protective glove 30.3±3 and without protective glove 29.9±3.6.
There were 26 interventions carried out without protective gloves: The mean age of the patients was 77.9±6.6 years; 15 women and 11 men. Average transmission time 323.69±325.7 seconds. Mean dose of the examiner’s hand was 47.24±40.83 μSv.
There were 24 interventions carried out with protective gloves. The mean age of patients was 70±11.1 years; 8 women and 16 men. Mean transmission time of 431.63±344.02 seconds. Mean dose of 60.61±78.66 μSv.
In the group, without a protective glove, a mean dose value of 0.76 mSv/h with a DAP of 6183.19 mGy*cm2 was obtained. In the group with protection, the resulting mean value was a dose rate of 0.43 mSv/h with a DAP of 10462.92 mGy*cm2. In comparison, there was a reduction of the dose rate by approximately 57%. There are no significant differences for the transmission time and the dose (t-tests for independent samples).
A significant difference of p<0.05 between the groups can be determined for the dose rate, whereby the dose rate for the protective glove was significantly lower. The DAP also showed a significant difference of p<0.05. In the group with a protective glove, the DAP was significantly higher [Table/Fig-4].
Examiner measurements: Cumulative dose values. t-test analysis. Comparing the dose values with and without a protection glove. Significant increase of the dose area product radiation using the protective glove: 6183.2 to 10462.9 mGy*cm2 (p<0.05). Reduction of the exposure for the examiner’s hand dose 0.76-0.43 μSv (p<0.05).

Regarding the sense of touch, no relevant restrictions were documented in 18 out of 24 applications. In 6/24 cases, the protective glove was evaluated as negative. These six cases were women with adipose tissue, with thin vascular lumina, so the inguinal pulse was difficult to detect anyway.
Discussion
A short distance of the examiner’s hand to the direct X-ray beam is in most cases unavoidable during interventional procedures. As well as, a lack of effective shielding threatened the interventional radiologist in the daily clinical routine. Wearing radiation protective gloves can make work in the angiolab safer but it is still not standard practice [10]. That may be due to the fact that radiological protection is currently based on leaded gloves [11]. Only a few studies mention the doses received by the hands and evaluated the options of radiation protection with a lead-free glove [12].
Interventional procedures require the examiner to remain close to the patient, which is the main source of scattered radiation. The interventional radiologist can also be subjected to primary irradiation, because of unhealthy practice, their hands enter the primary X-ray beam. Using the standard radiation protection garments, the examiner’s hand was always unshielded. Keeping the annual dose limit of 500 mSv for the hands in mind, it is important to protect the hand so that the limit of the dose values is not exceeded.
Interventional investigators were interested in collecting occupational dosimetric data with the aim of avoiding unnecessary radiation exposure for the patient and examiners. The interventional radiology represents a wide field of partly complex procedures. Depending on the complexity of the procedures [13], it was difficult to compare the data from different studies. Apart from technical settings (shielding and angiographic equipment), the dosimetric data were influenced by the experience of the interventionalist as well as the patient habitus [14-18].
In this study, the mean hand dose of an interventional angiography without a glove in antegrade technique was low by 47 μSv and equal to a study of Ingwersen M et al., by 42 μSv per procedure. Using the protection glove, an increase up to 60 μSv was observed [19] because of an automatic upregulation of the kV number while operating partly in the direct X-ray beam. In relation to the period of investigation, the increase of the dose was low because of the low lead equivalence value of the glove by 0.03-0.04 mm Pb. To avoid a kV upregulation, the kV automatic regulator can be switched of.
In any case, the examiner’s hands should not be placed in the primary X-ray beam. For some steps of the procedure, it is indispensable to act in the X-ray field. The more important is to develop shielding devices that not affect the performance of the procedure. Especially for shielding devices of the examiner’s hand, it is important to receive the feel to avoid prolonging of the procedure and thus also increasing the dose to the patient [20,21]. Efstathopoulos EP et al., mentioned disposable surgical gloves incorporating 0.02 mm of lead, with a dose reduction of only 15-20% [10]. With the new generation of protective, lead-free gloves a significant reduction of the examiners hand dose for scattered radiation under laboratory conditions (43%) and for the clinical practice (57%) was possible. The requirements for lead reduction are also fulfilled.
Because the angiographic interventional procedure, at the time of the inguinal artery puncture, makes it virtually impossible to keep the examiner’s hand out of the primary beam path, the phantom measurement was carried out specifically in the path of the direct X-ray beam. The comparison with and without protective glove shows a dosage control of 58 kV and 4.7 mAs up to 62 kV and 5.5 mAs, with a highly significant increase of the measured dosage parameters (Air Kerma, DAP, examiner’s hand dose).
The phantom measurement in the area of the scattered radiation shows a significant dose reduction for the examiner’s hand with a protective glove if device parameters remain unchanged (48 kV, 3 mAs).
With the phantom and also with the patient, the study confirms the protective properties of the new generation of protective gloves with regard to radiation.
The flexibility of the gloves increases the acceptance of the protective measures and allows them to be used in angiography where, as a rule, an acquired finger dexterity is of great importance. However, the high costs involved must be considered.
To protect examiners from radiation effects, dose limits have been established. An important component of radiation protection is therefore the official personal dosimetry.
The official personal dosimetry requires a whole body dosimeter, which is to be worn under the lead protective apron in the area of the front of the torso. However, this dosimeter does not allow monitoring at the site of unprotected exposure. As part of an optimization of the radiation protection, one should rely not only on the data of dosimeters worn underneath the protective apron but also on dosimetry measurements of unprotected body regions. Hand-held finger ring dosimeters can provide those information [22,23]. The disadvantage of these dosimeters is the timewise delay of the evaluation so that no direct conclusions can be drawn about the radiation exposure during an intervention.
In the medical field, furthermore, personal dosimeters are used which provide direct information, eg., electronic personal dosimeters. The working group of Adamus R et al., dealt with personal dosimetry in interventional measures, using a direct dosimeter for partial body dosage measurement [24]. With a direct dose measurement, the interventional radiologist gathers informations during the procedure and gets the opportunity to react on the radiation exposure. After reaching a threshold value, an additional acoustic signal amplifies the information flow this lead to a situation analysis of the examiner, which may lead to a change in behavior [7]. There occurs a sort of training, with which an improvement in radiation protection can be achieved. Accurate knowledge of exposure may influence the acceptance and application of additional safeguards [25,26].
Limitation
In this single-center study, only one intervention technique (antegrade puncture) was examined. Further techniques in multicenter studies with a higher number of investigations are needed to show more correlation between procedural characteristics and radiation exposure of the operator’s hand.
Conclusion
The new generation of protective gloves is characterized by a shielding effect against X-ray scattered radiation, without restricting the sense of touch. A significant reduction in radiation doses to the examiner can be accomplished with these gloves in the area of scattered radiation only. If the gloves were used in the direct X-ray beam, escpecially while the artery puncture was performed, a significant increase of the dose values were observed.