Hypertensive disorders are the most common medical problem during pregnancy. These disorders are responsible for complications in 10%-15% of the pregnancies which can cause significant maternal and perinatal morbidity and mortality. Intracranial hemorrhage is the commonest complication associated with hypertension [1,2]. The hypertensive disorders of pregnancy have been classified by the Working Group of the National High Blood Pressure Education Program [NHBPEP] (2000) into five types [3]:
Preeclampsia is one of the common and important hypertensive disorders of pregnancy both in high and low-income countries which causes maternal and foetal morbidity and mortality [4]. It causes imbalance in maternal homeostasis and creates unfavorable environment for the foetus. It also leads to acute and chronic uteroplacental insufficiency due to which there is development of antepartum or intrapartum anoxia that may cause IUGR, preterm delivery and foetal death. It is also a frequent cause for emergency hospitalization, labor induction and dystonic labor [5].
Normal pregnancy is associated with physiological blood changes like neutrophilic leukocytosis, hyperlipidemia, procoagulant property and inflammation. Preeclampsia is a condition which leads to enhancement of these changes and also leads to placental abnormalities which can cause haematological abnormalities and foetal complications [6,7].
Hence, the purpose of the study was to identify the changes in neonatal haematological profile so that early detection and prophylactic treatment can reduce the morbidity and mortality of the newborn.
Materials and Methods
This prospective case control study was conducted at R.L.Jalappa Hospital and Research Centre Karnataka, India, for duration of six months (March 2016 to November 2016). Before starting the study, ethical clearance was taken from the Institutional Ethical Committee. It included 60 cases and 60 controls. Case group included the neonates born to pregnant women with Preeclampsia i.e., a) hypertension with proteinuria (systolic pressure elevated > 140 mm of Hg and diastolic pressure >90 mm of Hg appearing for the first time after 20 weeks of gestation b) proteinuria alone (>300 mg /24 hour). Babies born to mothers with other risk factors like Rh incompatibility, diabetes mellitus, medical illness such as severe anaemia, chronic hypertension, renal disease, heart disease, connective tissue disease, babies born to mothers with hypertension diagnosed before 20 weeks of gestation and babies with congenital malformations were excluded from the study.
For all the neonates who were included in the study detailed maternal history, details of labour, details of baby were taken. Thorough clinical examination of the neonates was done. Anthropometric parameters like head circumference, chest circumference, length, height, weight, and ponderal index were recorded.
After birth, immediately 2 ml of blood was collected from the umblical cord into the vaccutainer anticoagulated with EDTA and following parameters were studied:
Hb, TC, DC, platelet count and the red cell indices - MCV, MCH, MCHC was estimated using 5 part Sysmex Automated cell analyser. This analyser works on the principal of volumetric impedance and photometric measurement of light absorbance.
Reticulocyte count was estimated using the peripheral smear stained with supravital stain i.e., methylene blue stain.
Statistical Analysis
Data was entered into Microsoft excel data sheet and was analyzed using SPSS 22.0 version software. The difference between the two groups was compared using independent student ‘t’ test. The p-value <0.05 was considered as statistically significant.
Results
All the cases both in the case and control were booked (registered cases who were on regular check up). Details of study and control group have been shown in [Table/Fig-1]. APGAR scores of the babies in case group at the first and fifth minute was 7.9 and 9.2 and that of control group was 8.1 and 9.4 respectively.
Details of the mother and baby of both study and control group.
| Parameter | Study group | Control group |
|---|
| Mean maternal age | 23.6 | 23.8 |
| Parity | Primipara-70% (42/60)Multipara-30% (18/60) | Primipara-50% (30/60)Multipara-50% (30/60) |
| Mean systolic BP | 151 mmHg | 122mmHg |
| Mean diastolic BP | 105 mmHg | 80mmHg |
| Mean proteinuria | 2.15 g/24 hour urine | Nil |
| Operative delivery | 80% (48/60) | 40% (24/60) |
| Premature babies(<37 weeks) | 70% (42/60) | 10% (6/60) |
| Mature babies (>37 weeks) | 30% (18/60) | 90% (54/60) |
| Mean Birth weight | 2.35 kg | 2.9 kg |
| IUGR | 55% (33/60) | 10% (6/60) |
| Sepsis | 50% (30/60) | 15% (9/60) |
The comparison of haematological profile in case and control group is shown in [Table/Fig-2].
Complete blood count and peripheral smear parameters of the study group and control group.
| Parameter | Study group(Mean±SD) | Control group(Mean±SD) | p-value |
|---|
| Hb (g/dl) | 17.6 ± 1.17 | 14.6 ± 0.65 | <0.001 |
| RBC (x 106/mm3) | 4.96 ± 0.32 | 4.56 ± 0.22 | <0.001 |
| Haematocrit (%) | 53±3.6 | 45.1±1.7 | <0.001 |
| MCV (fl) | 108.9±4.7 | 104.76±1.93 | <0.001 |
| MCH (pg) | 35±1.25 | 35.2±2.01 | 0.406 |
| MCHC (g/dl) | 32.85±0.83 | 33.37±1.02 | 0.08 |
| Total leukocyte count | 8989±818 | 15382±992 | <0.001 |
| Neutrophils (%) | 45.9±2.12 | 52.2±1.72 | <0.001 |
| ANC | 4723.15±255 | 9233±630 | <0.001 |
| Lymphocytes (%) | 43.03±2.29 | 44.91±2.25 | <0.001 |
| nRBC (/100wbc) | 20.3±2.47 | 6.30±1.31 | <0.001 |
| Reticulocytes (%) | 10.75±2.52 | 2.04±0.87 | <0.001 |
| Platelet count(x103/mm3) | 94.2±10.3 | 202.6±31.05 | <0.001 |
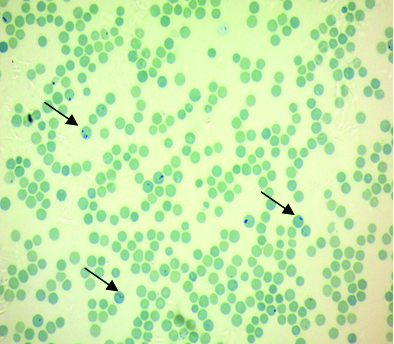
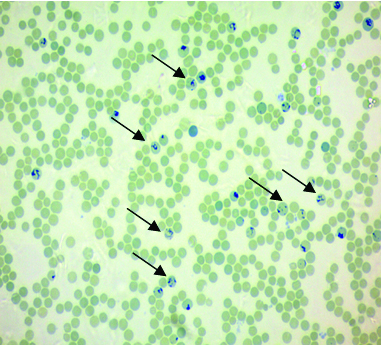
In our study, mean Hb, PCV, red cell count, MCV, reticulocyte count [Table/Fig-3, 4] and nRBC were significantly increased p<0.001 whereas total leucocyte count, mean neutrophil count, absolute neutrophil count, platelet count were significantly decreased p<0.001 in babies born to preeclamptic mothers. Lymphocyte count was also decreased in the study group with p <0.001. No difference was found between the two groups in the MCH and MCHC value p >0.05.
Microphotograph of the supravital stain of control group showing less number of reticulocytes (arrow) (methylene blue 40X);
Microphotograph of the supravital stain of case group showing increased number of reticulocytes (arrow) (methylene blue 40X).
Discussion
Preeclampsia is a pregnancy specific disorder which causes multisystem dysfunction and is the leading cause of maternal and neonatal morbidity and mortality worldwide. About 2%-8% of preeclamptic mothers develop complications and it results in more than 63,000 maternal deaths every year worldwide [8,9].
The International Society for the Study of Hypertension in Pregnancy (ISSHP) has suggested the following definitions for study purposes but has also considered a proposal for clinical diagnostic criteria [10].
New onset of hypertension with a systolic blood pressure ≥140 and/or a diastolic blood pressure ≥90 mm Hg after 20 weeks of gestation
Proteinuria ≥300 mg/24 hour or a spot urine protein/creatinine ratio ≥30 mg/mmol.
The blood pressure should return to normal postpartum.
The pathogenesis of preeclampsia is failure of trophoblastic invasion of the spiral arteries. These arteries will have accumulation of the fibrinoid material and foam cells which leads to reduced blood flow and favours the interaction between the surrounding cells. Longer exposure of RBCs to oxygen metabolites and proteases produced by inflammatory cells causes RBC damage which may compromise maternal foetal exchange of oxygen and hence, alters placental homeostasis and foetus development [11].
The frequency of preeclampsia in pregnant women ranges between 10%-14% in primigravida and 5.7-7.3% in multigravida. It is commonly seen in first pregnancy and in younger age group [12]. In our study also, 70% were primigravida who presented with preeclampsia.
Majority of mothers in the study group were delivered by caesarean section when compared to control group to prevent complications for both mother and the foetus.
Preeclampsia is a significant risk factor and most common cause for development of intrauterine growth restriction and foetal mortality. The proposed hypothesis for this is that decreased uteroplacental blood flow and ischemia leads to decrease in nutrients nourishing the baby and causes IUGR [12]. In our study, birth weights in the study group were found to be lower when compared to the control group.
Newborn infants born to preeclampsia present with prematurity, respiratory distress syndrome, bronchopulmonary dysplasia and higher incidence of sepsis [13]. In our study, 70% of the babies born to preeclamptic mothers were premature and 50% of the babies developed sepsis. The percentage of preterm and also incidence of sepsis were high in this study as seen in the earlier studies too [14, 15].
Haemoglobin concentration showed a mean of 17.6 g/dl i.e., polycythemia and RBC count of 4.96 x 106/mm3 which was comparable to Bolat A et al., [12]. In the study done by Kurlat I et al., the risk of polycythemia in babies born to hypertensive mothers compared to general population was 12.6 fold and was proven that maternal hypertension constitutes a significant risk for polycythemia independent of foetal growth [16].
Mean haematocrit observed in this study was 53% in cases and 45.1% in controls as compared to Saarinen UM and Siimes MA (35-59%) [17]. As haemoglobin increases haematocrit also increases.
In this study, we noted an increase in MCV (108.9±4.8) in the infants born to mothers of preeclampsia which correlated well with Prakash PL et al., and Saarinen UM and Siimes MA. and this increase may be due to increase in the size of RBCs in preterm babies [5,17].
There was no significant difference found in MCH (35.04±1.25) and MCHC (32.85±0.81) which was comparable to Sivakumar S et al., Bolat A et al., and Prakash PL et al., [18,12,5].
In our study, we noted an increased number of nRBCs in the peripheral smear of babies born to preeclamptic mothers with a mean of 20.30/100 WBCs when compared to nRBCs of babies born to normal mothers with a mean of 6.30/100 WBCs. This difference was strongly statistically significant with p<0.001. Thus, nRBCs count will be predominantly increased in the babies born to preeclamptic mothers. This finding correlated with Salaia CM et al., and Philip et al., [19,2].
There is a hypothesis which has been proposed for increased number of nucleated RBC’s in preeclampsia. It states that the cytotrophoblasts are unable to differentiate correctly and this leads to failure of invasion of cytotrophoblasts and its arterioles into the uterus. This relatively leads to hypoxic environment in the placenta which results in increased production of erythropoietin which in turn leads to stimulation of erythropoesis and thereby increased number of nucleated RBC. Therefore, increased count of nRBC is considered as a marker of hypoxia [20].
This study showed an increase in the number of reticulocyte count with a mean of 10.75% in the study group and was found to be strongly significant when compared to control group with p<0.001. This finding correlated well with Bolat A et al., [12] and Cristina C et al ., [21]. Increase in reticulocyte count is mainly due to high erythropoietic stimulus to face a higher RBC destruction and removal. It also reflects an underlying placental hypoxic condition [20,22].
The mean total leucocyte count and neutrophil count in the study group was 8989 /mm3 and 45.9% respectively and it was less when compared to controls with p<0.001 which correlated well with Bolat A et al., Cristina C et al., and Prakash PL et al., [12,21,5]. Leucopenia was found in 28.5% of the babies in the study done by Mosayebi Z et al., which was more common in babies of gestational age of 32-37weeks [23]. Harms K et al., demonstrated leucopenia in 21% of the affected infants [24].
Preeclampsia is a common known risk factor for neonatal neutropenia with the incidence of 50% [23] and is the cause for neonatal sepsis mainly in premature newborns. It is a transient haematologic alteration which lasts for days and weeks. Koenig TN and Christensen RD stated that neutropenia and leucopenia was caused by decrease in Granulocyte Colony Stimulating Factor (G-CSF) which is an important haematopoietic growth factor for granulocyte differentiation and proliferation. Neutropenia associated with maternal preeclampsia is also associated with uteroplacental insufficiency which inhibits foetal bone marrow production of the myeloid lineage [25,12].
In this study, neutropenia caused decrease in absolute neutrophil count which was 4723 /mm3 and was statistically significant with p<0.001. This finding correlated well with Dagar J and Aundhakar C et al., and Prakash PL et al., [26,5].
Lymphocyte count was also reduced in this study with 43.03% and p<0.001 which correlated with the finding of Bolat et al and Prakash PL et al., [12,5].
The most significant feature found in our study was the presence of thrombocytopenia in the babies born to preeclamptic mothers and it was 94,250/mm3 when compared to babies of normotensive mothers having mean platelet count of 2 lakh/mm3 with p<0.001. In newborns born to preeclamptic mothers, the incidence of thrombocytopenia was found to be higher compared to the newborns of normotensive mothers. The underlying pathophysiologic mechanism for thrombocytopenia is not clear but there are studies which states that pathology arises at the placental level, in which thrombocytes gets attached to endothelial cells which are damaged due to segmental vasoconstriction and dilatation of the blood vessels in the placenta of preeclamptic mothers leading to thrombocytopenia [27].
Limitation
The duration of the study was short. Follow up of the neonates could not be done. The correlation between neonates and mother’s haematological parameters were not analysed.
Conclusion
Preeclampsia is a maternal pathology involving placental modification which is associated with foetal complications. Maternal and foetal morbidity and mortality are serious concerns in preeclampsia and are attributable to poor management.
In our study, we observed many changes in the haematological profile of newborns born to preeclamptic mothers. All changes should be kept in mind while interpreting the haematological values in these babies and haematologic follow up should be performed in these newborns to decrease the risk of sepsis and bleeding manifestation. Hence, early haematological screening of these babies with laboratory tests like complete blood count and peripheral smear examination helps in early diagnosis of haematological complications and thus early management of sepsis and bleeding manifestations.
Funding: We would like to acknowledge the ICMR-STS for the financial support.