Concurrent Acute Glomerulonephritis and Retropharyngeal Abscess in 10 Year Boy: A Case Report
Sudha Yadav1, Deepali Garg2, Narain Das Vaswani3, Jaya Shankar Kaushik4, Seema Rohilla5
1 Resident, Department of Pediatrics, Pt B D Sharma PGIMS, Rohtak, Haryana, India.
2 Resident, Department of Pediatrics, Pt B D Sharma PGIMS, Rohtak, Haryana, India.
3 Professor, Department of Pediatrics, Pt B D Sharma PGIMS, Rohtak, Haryana, India.
4 Associate Professor, Department of Pediatrics, Pt B D Sharma PGIMS, Rohtak, Haryana, India.
5 Professor, Department of Radiodiagnosis, Pt B D Sharma PGIMS, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jaya Shankar Kaushik, Associate Professor, Department of Pediatrics, Pt B D Sharma PGIMS, Rohtak-124001, Haryana, India.
E-mail: jayashankarkaushik@gmail.com
Postinfectious Glomerulonephritis (PIGN) usually follows 1-2 weeks after respiratory tract infection and 4-6 weeks after skin infection. Acute Glomerulonephritis (AGN) is uncommon with simultaneous severe throat infections. We describe a 10-year-old boy who was presented with high grade fever, dysphagia and tender swelling over left side of neck. Examination also revealed enlarged multiple cervical lymph nodes on the same side of neck. Magnetic Resonance Imaging (MRI) of soft tissue of neck revealed evidence of retropharyngeal abscess. The next day, he subsequently developed haematuria and oliguria with borderline raised blood pressure. His corresponding blood urea and serum antistreptolysin O (ASO) levels were raised with low C3 levels. He had a remarkable improvement on injectable broad spectrum antibiotics with complete resolution of fever and neck symptoms. At eight weeks follow up, complete resolution of microscopic haematuria with normal C3 levels was observed. The present case highlights a 10-year-old young boy with retropharyngeal abscess presenting with clinical and laboratory evidence of Poststreptococcal Glomerulonephritis (PSGN).
Haematuria, Hypocomplementemic glomerulonephritis, Nephritic syndrome, Respiratory tract infections
Case Report
A 10-year-old boy presented with a history of high-grade fever, dysphagia and pain during neck movements for last five days. He had restricted neck movement with difficulty in swallowing and a swelling over the left side of neck. By the second day of illness, he developed decreased urine output with the passage of cola coloured urine. By day 4, he also developed minimal periorbital puffiness. There was no history of rash, joint pain, excessive sensitivity to sunlight or bleeding from any other site. There was no history of any prolonged drug intake or past history of similar illness. He was developmentally normal fifth grade student who has been immunized as per the age. On examination, he was conscious and alert with a heart rate of 98/min, respiratory rate of 24/min and blood pressure was 120/82mm Hg (>95th percentile for age and height) as measured through right arm in supine position. His anthropometric variables were within normal percentiles for age and gender. On general physical examination, there was clinical evidence of facial puffiness and pitting pedal oedema. There was no pallor or icterus. He had a painful, warm swelling over left side of the neck with multiple discrete small (0.5 x 0.5 cm) submental, submandibular and upper cervical group of lymph nodes with restriction of neck movement. Oral examination revealed a diffuse bulge in posterior pharynx with normal tonsils. There was no organomegaly and the rest of systemic examination was unremarkable. Laboratory investigations revealed leucocytosis {TLC 22,400/cumm (88% polymorphs)} and X-ray of neck was unremarkable. However, MRI of neck revealed T1 hypointense and T2 hyperintense lesions measuring 2.4×5×5 cm seen in left retropharyngeal space pushing the carotids posterolaterally and parapharyngeal fat anteriorly suggestive of retropharyngeal abscess [Table/Fig-1a]. His blood urea was 125 mg/dl and serum creatinine was 1.9 mg/dl. His urine output remained at 0.5-0.6 ml/kg/hr with gross haematuria. Urine microscopic examination revealed Red Blood Cells (RBCs) and the urine protein as determined by reagent strip was graded 2+ (100 mg/dl). Complement C3 levels were decreased (21 mg/dl; 90-180 mg/dl) and ASO level was raised to 812 mg/dl (<400 mg/dl). Moreover, negative titres of Anti-Nuclear Antibody (ANA) and no growth revealed in throat culture confirmed a clinical diagnosis of PSGN with retropharyngeal abscess.
Sagittal MRI neck image showing T2 hyperintense collection in retropharyngeal space (yellow arrow) extending from C1 to C4 vertebral level suggestive of a) retropharyngeal abscess b) with decrease in size of abscess at eight weeks follow up.
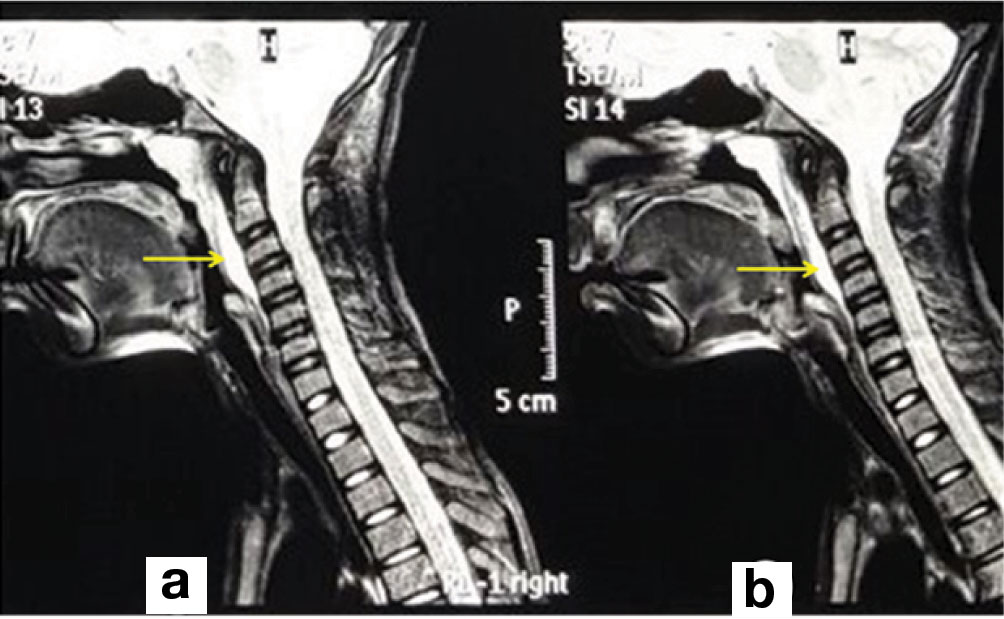
The child was started on intravenous ceftriaxone and linezolid. He showed remarkable improvement in symptoms of neck and was able to start swallowing the food by fourth day of admission. Fever had subsided and the blood pressure returned to normal percentiles within five days (without antihypertensives). Subsequently, gross haematuria had resolved and urine output had improved, although, microscopic haematuria persisted till discharge. The surgical opinion was sought for retropharyngeal abscess and in view of remarkable clinical improvement with antibiotics, surgical intervention was deferred. Hence, pus drainage and its culture were not performed from the retropharyngeal abscess. The child was discharged after four weeks of intravenous antibiotics and was started on oral cefixime and oral linezolid for the next four weeks. At eight weeks follow up, neck swelling had clinically subsided, microscopic haematuria also resolved, urine albumin reached within the range of traces, ASO titers returned to 250 mg/dl. Repeated MRI of neck showed a decrease in the size of the abscess to 0.5 × 1 × 1 cm [Table/Fig-1b]. Renal biopsy was deferred in view of consistent improvement in gross haematuria, also, oedema had subsided, hypertension got settled and C3 levels returned to normal, at eight weeks follow up.
Discussion
PIGN is an immunologic response of the kidney to Group A streptococcal infection that usually occurs 1-2 weeks following the throat infection and 4-6 weeks following skin infection [1]. To the best of our literature search, severe infections like retropharyngeal abscess simultaneously presenting with clinical and serological evidence of PIGN have not been reported previously. This case highlights an uncommon association of retropharyngeal abscess with PSGN that occurred simultaneously and prompts the physician to search for other infection that causes glomerulonephritis.
Development of acute nephritic syndrome following infection is broadly labelled as PIGN. PSGN is a form of PIGN that is caused by infection with Streptococcus pyogenes. It is characterized by the sudden appearance of haematuria, proteinuria, oedema and hypertension [2]. It is accompanied by serological evidence of streptococcal infection (antistreptolysin O titre or anti-DNase B titre) and low complement C3 level which returns to normal within eight weeks. Conventionally, majority of PIGN follows pyoderma and occasionally respiratory tract infection. However, in a study done by IIyas M et al., it was observed that there has been a paradigm shift in epidemiology of PSGN with recent cohort depicting decline in incidence, mild severity, resulting from pharyngeal infection rather than skin infection and clustering of cases during monsoon months [3].
PSGN is commonly triggered by streptococci and it results from the glomerular deposition of circulating immune complexes (IgG, IgM, C3) or direct antibody binding to an antigen expressed in the glomerulus. Long-term renal complications including rapidly progressive glomerulonephritis secondary to crescentic glomerulonephritis are uncommon [4]. Indications for renal biopsy in children with PSGN include normal C3 level, negative ASO titre, persistent renal insufficiency beyond seven days, persistently low C3 level beyond 6-8 weeks and recurrent episodes of haematuria. Hence, in view of clinical remission with return of normal C3 level in the index case, renal biopsy was deferred. PSGN by convention is considered a nonsuppurative complication of Group A streptococcal infection [5]. Co-occurrence of the retropharyngeal abscess with PSGN is not known in the medical literature.
Clinical differentials for AGN in children include infectious (Streptococcus, Staphylococcus, Salmonella typhosa, hepatitis B virus, cytomegalovirus, rubella, coxsackievirus, Epstein-Barr virus and Plasmodium falciparum) and non-infectious causes (vasculitis, Henoch-Schönlein purpura, systemic lupus erythematosus and polyarteritis nodosa) [6]. Considering presence of retropharyngeal abscess in our case and negative titres of ANA along with lack of clinical features suggestive of systemic vasculitis or collagen vascular disease, infective cause seems more likely in our case.
Retropharyngeal abscess is second most common deep neck infection after tonsillar infection in children and is often caused by beta hemolytic Streptococcus, Staphylococcus aureus or rarely Gram-negative organism like Haemophilus parainfluenzae [7]. It may develop by contiguous spread of tonsillar, pharyngeal, salivary gland, dental infections or lymphatic spread from cervical lymphadenitis. It may also result from oropharnygeal trauma, instrumentations, foreign body aspiration or among those with immunosuppression like HIV infection [8]. We believe that significant cervical lymphadenopathy in our case could be the possible focus of retropharyngeal abscess. However, pus aspiration or drainage for identifying organism was not performed. It is important to note that despite extensive search, 20%-50% of deep neck infections have no identifiable cause [8]. Despite a wide list of causes of AGN in children, the most common cause of AGN remains Group A Streptococcus. Antecedent pharyngeal infection in PIGN is common among those above six years of age [2]. Serological evidence of recent streptococcal infection (positive ASO titres) in the background of the acute nephritic picture of haematuria, proteinuria, oliguria and hypertension along with hypocomplementaemia fits the definition of PSGN in our case. AGN as an infective complication of severe pharyngeal infection is a possible differential diagnosis considering the fact that symptoms had resolved following medical therapy with antibiotics. However, hypocomplementaemia, positive serological evidence of streptococcal infection and lack of positive throat culture for active streptococcal infection point towards PIGN rather than acute infective glomerulonephritis.
Conclusion
Traditionally, PSGN occurs 1-2 weeks following throat infection with Group A Streptococcus. The present case highlights co-occurrence of severe pharyngeal infection (retropharyngeal abscess) with AGN. This prompts the physician to look for other infections that could cause acute AGN in children.
[1]. Vogt B, Nephrology update: Glomerular disease in childrenFP Essent 2016 444:30-40.quiz 41-43 [Google Scholar]
[2]. VanDeVoorde RG, Acute poststreptococcal glomerulonephritis: the most common acute glomerulonephritisPediatr Rev 2015 36(1):3-12.quiz 13 [Google Scholar]
[3]. Ilyas M, Tolaymat A, Changing epidemiology of acute post-streptococcal glomerulonephritis in Northeast Florida: a comparative studyPediatr Nephrol 2008 Jul 23(7):1101-06. [Google Scholar]
[4]. Gunasekaran K, Krishnamurthy S, Mahadevan S, Harish BN, Kumar AP, Clinical characteristics and outcome of post-infectious glomerulonephritis in children in southern India: A prospective studyIndian J Pediatr 2015 82(10):896-903. [Google Scholar]
[5]. Nissenson AR, Baraff LJ, Fine RN, Knutson DW, Poststreptococcal acute glomerulonephritis: fact and controversyAnn Intern Med 1979 91(1):76-86. [Google Scholar]
[6]. Dagan R, Cleper R, Davidovits M, Sinai-Trieman L, Krause I, Post-infectious glomerulonephritis in pediatric patients over two decades: severity-associated featuresIsr Med Assoc J 2016 18(6):336-40. [Google Scholar]
[7]. Huang CM, Huang FL, Chien YL, Chen PY, Deep neck infections in childrenJ Microbiol Immunol Infect 2015 Sep 9 [Google Scholar]
[8]. Craig FW, Schunk JE, Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current managementPediatrics 2003 111(6 Pt 1):1394-98. [Google Scholar]