Caudal Regression Syndrome with Pressure Ulcers of the Foot: A Case Report
Kosaku Yamamichi1, Tsuyoshi Manabe2, Tatsuya Uekihara3
1 Director, Department of Plastic and Reconstructive Surgery, Fukuoka Sanno Hospital, 3-6-45 Momochihama, Sawara-ku, Fukuoka, Japan.
2 Director, Department of Plastic and Reconstructive Surgery, Hakujyuji Hospital, 3-2-1 Ishimaru, Nishi-ku, Fukuoka, Japan.
3 Senior Resident, Department of Plastic and Reconstructive Surgery, Kanagawa Children’s Medical Center, 2-138-4 Mutsukawa, Minami-ku, Yokohama, Kanagawa, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kosaku Yamamichi, Director, Department of Plastic and Reconstructive Surgery, Fukuoka Sanno Hospital, 3-6-45 Momochihama, Sawara-ku, Fukuoka, 814-0001, Japan.
E-mail: yamamichi@kouhoukai.or.jp
Caudal Regression Syndrome (CRS) is a rare disorder which consists of abnormalities in the lumbosacral spine, rectum, urinary system and lower limbs. These abnormalities also include orthopaedic deformities, such as hip dislocation, knee-flexion contracture with popliteal webbing and talipes equinovarus. Because of the rarity of this condition, few medical personnel are aware of it. Here, we present a case of CRS in a 15-year-old girl with pressure ulcers on the lateral malleolus and plantar surface of the foot, which had come into contact with the wheelchair footrest. Although the foot ulcers healed after off-loading, the ulcer on the lateral malleolus did not heal with conservative treatment and was covered by a lateral supramalleolar flap after debridement. Stable coverage and good contours were present at 18 months postoperatively. CRS patients may have a risk factor for developing pressure ulcers of the foot due to the characteristic lower limb deformities and a loss of sensation. Preventive foot care measures such as off-loading devices combined with modern dressings should be applied as routine when the medical personnel is to attend such patients.
Caudal dysgenesis, Lower extremity deformities, Perforator flap
Case Report
A 15-year-old girl was referred to the Plastic and Reconstructive Department with the complaints of non-healing foot ulcers [Table/Fig-1,2] and deformed lower limbs and feet [Table/Fig-3].
Appearance of the pressure ulcer on the ankle.

Appearance of the pressure ulcers on the planter surface of the foot.

A 15-year-old girl had deformed lower limbs and congenital talipes equinovarus.

This patient was diagnosed as having CRS shortly after birth with the conditions described as follows: At birth, she had frog abdomen, hip dislocation, lower limb anomalies and bladder and rectal disturbances. Her lower limbs were hypoplastic with no muscle activity. Her knees had flexion contractures with popliteal webs and talipes equinovarus was observed. Lumber spine radiograph revealing the agenesis of the upper lumbar vertebrae L1 through L5 with complete disconnection was a determinant factor to diagnose CRS. It should be also noted that her mother had a maternal history of diabetes but no history of drug use, radiation exposure or any other serious diseases. On the contrary to her mother’s diabetic history, the patient has not developed the diabetes or hypoglycaemia so far.
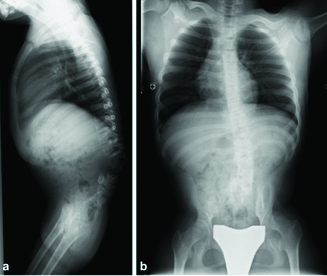
Conventional ankle-foot orthoses have been worn for equinovarus foot deformities soon after birth, however, malalignment and instability of the ankle has remained. At the age of eight, she had undergone spinal fixation, bone grafting in the spine and tendon lengthening surgery [Table/Fig-4a,b].
Radiograph of the patient at eight-years-old shows the agenesis of the spine L1 through L5 with complete disconnection and confirms the earlier diagnose of CRS when the patient was infant.
Although she was unable to walk, she had no mental retardation so that she went to the regular schools on wheelchair rather than special needs schools. Her lower limbs helped maintain her sitting balance by placing her foot on the wheelchair footrest. By the age of 13, the pressure ulcers gradually developed on her lateral malleolus and plantar surface of the foot, as they have been rubbing against the wheelchair foot rests. The ulcer on the lateral malleolus reached the bone with a subcutaneous pocket. The ulcer was 15 × 10 mm and the subcutaneous pocket was 36 × 35 mm in size respectively.
The foot ulcers on the plantar surface healed after using a non-removable fiber glass off-loading cast. However, the ulcer on the lateral malleolus did not heal with conservative treatment. In order to rectify the problem, we performed the flap coverage surgery after debridement then we used the lateral supramalleolar flap for reconstruction of skin defect on the lateral malleolus [Table/Fig-5]. The flap remained intact without complications. Stable coverage and good contour were obtained at 18 months postoperatively [Table/Fig-6]. Subsequently, we re-examined the utility of educating the patient and family regarding the pressure ulcer prevention program. We found that she was able to return to school life without any ulcer recurrences.
The lateral malleolar defect after the debridement, showing the outline of a lateral supramalleolar flap.

Appearance at 18 months after surgery. Stable coverage and good contour were obtained.

Discussion
CRS is a rare congenital malformation. It comprises varying degrees of agenesis of the sacral, lumbar and lower thoracic vertebrae. Associated malformations include vertebral, anorectal, urological, genital and lower limb anomalies [1-3]. Orthopaedic deformities, such as dysplastic vertebrae, hip dislocation, flexion contractures of the knee and popliteal webbing, frog leg and talipes equinovarus have also been observed [1-3].
Because of its rarity, few medical personnel are aware of this condition and no other documented cases of CRS with pressure ulcers of the foot have been described in the literature. CRS was first proposed by Duhamel B [4] and Sirenomelia was previously thought to be a severe form of CRS [4]. However, it has been determined that they are clinically separate diseases based on onset frequency and disease severity [5].
The prevalence of CRS is estimated to be 0.1–0.2 cases per 10,000 normal pregnancies [6]. A disturbance of the primary neurulation process during the first four weeks of development may be the pathogenesis of the CRS [1]. Although the exact cause of CRS remains unknown, an association with diabetes mellitus is considered the most common possible risk factor [7]. Clinically, sacral or lumbosacral agenesis in combination with marked hypoplasia of the lower extremities is diagnostic of CRS [8]. Many anomaly phenotypes, such as imperforate anus, horseshoe kidneys or external genitalia hypoplasia, also accompany the sacral agenesis in CRS [1-3,9,10]. Bohring A et al., reported craniofacial and cardiac malformation accompanied to caudal agenesis [11]. The patient’s mother had a maternal history of diabetes in the case presented and the patient had neurogenic bladder with urinary incontinence. There had been some similar cases previously reported [9,10,12].
As for the multiple congenital neurologic and orthopaedic abnormalities, these are always associated with CRS patient [3]. Deformed lower limbs and talipes equinovarus were recorded in most reports [9,10,12]. It has been reported that some patients had the flexion contractures with popliteal webs since birth, just as the case we described in this report [9,12]. Occasionally, knee disarticulation and prostheses can be considered if the patients lack quadriceps muscle strength. However, securing maximum functionality of the residual lower limbs is recommended [9]. The level of activities of daily living may depend on the degree of vertebral abnormalities. Patients with thoracic and upper lumbar involvement cannot be expected to ambulate and have to use wheelchairs, however, the patients with middle lumbar or sacral involvement may be able to walk [9]. Although only few reports are available, Sharma S et al., described that some adults with CRS have attended school and have found employment [8].
There are no such reports that have focused on pressure ulcers of the CRS patients’ foot so far. In CRS patients, sitting posture can be stabilised by the use of impaired lower limbs, which have a loss of sensation, but at the price of ulcer development. Therefore, awareness of ulcer risk and preventive measures are essential [13]. The patient and family should be made aware that pressure ulcers can easily occur on the surface of the foot that comes in contact with the wheelchair. Preventive foot care measures such as off-loading devices combined with modern dressings should be applied as routine when the medical personnel is to attend such patients. We also strongly believe that a multidisciplinary approach should be adopted for CRS patients.
Lower limb reconstruction for children using perforator flaps is challenging. It may be also controversial as some surgeons may question the safety of perforator flaps use to the patient with such lower limb anomaly. The lateral supramalleolar flap was described by Masquelet AC et al., in 1988 and has become one of the few options for covering the distal third of the leg, foot, ankle and heel [14]. This is a fasciocutaneous flap based on the branch of the fibular artery, which is reliable because the main trunk arteries can be preserved. The flap can be elevated rapidly and achieve the minimal donor-site morbidity without functional damage. The lateral supramalleolar flap is also used for children [15]. In the case presented, preoperative assessment using colour Doppler ultrasound was carefully undertaken and we were able to identify the perforator artery of the peroneal artery. Computed tomography angiography may also be useful to evaluate if the perforator could be used. In this report, we indicated that this flap could be a choice for covering the foot and ankle for the patient with CRS.
Conclusion
We described a case of CRS that required treatment for pressure ulcers on the foot and ankle. It should always be considered that CRS patients might have a risk factor for developing pressure ulcers of the foot due to the characteristic lower limb deformities and a loss of sensation. Preventive foot care measures such as off-loading devices combined with modern dressings should be applied as routine when the medical personnel is to attend such patients.
[1]. Nievelstein RA, Valk J, Smit LM, Vermeij-Keers C, MR of the caudal regression syndrome: embryologic implicationsAm J Med Genet 1994 15:1021-29. [Google Scholar]
[2]. Mandour C, El Mostarchid B, A rare congenital malformation: caudal regression syndromePan Afr Med J 2013 14:30 [Google Scholar]
[3]. Tsugu H, Fukushima T, Oshiro S, Tomonaga M, Utsunomiya H, Oshima K, A case report of caudal regression syndrome associated with an intraspinal arachnoid cystPediatr Neurosur 1999 31(4):207-12. [Google Scholar]
[4]. Duhamel B, From the mermaid to anal imperforation: the syndrome of caudal regressionArch Dis Child 1961 36:152-55. [Google Scholar]
[5]. González-Quintero VH, Tolaymat L, Martin D, Romaguera RL, Rodríguez MM, Izquierdo LA, Sonographic diagnosis of caudal regression in the first trimester of pregnancyJ Ultrasound Med 2002 21:1175-78. [Google Scholar]
[6]. Baxi L, Warren W, Collins MH, Timor-Tritsch IE, Early detection of caudal regression syndrome with transvaginal scanningObstet Gynecol 1990 75:486-89. [Google Scholar]
[7]. Lynch SA, Wang Y, Strachan T, Burn J, Lindsay S, Autosomal dominant sacral agenesis: Currarino syndromeJ Med Genet 2000 37(8):561-66. [Google Scholar]
[8]. Sharma S, Sharma V, Awasthi B, Sehgal M, Singla DA, Sacral agenesis with neurogenic bladder dysfunction-a case report and review of the literatureJ Clin Diagn Res 2015 9(6):8-9. [Google Scholar]
[9]. Bicakci I, Turgut ST, Turgut B, Icagasioglu A, Egilmez Z, Yumusakhuylu Y, A case of caudal regression syndrome: walking or sitting?Pan Afr Med J 2014 18:92 [Google Scholar]
[10]. Tortori-Donati P, Fondelli MP, Rossi A, Raybaud CA, Cama A, Capra V, Segmental spinal dysgenesis: neuroradiologic findings with clinical and embryologic correlationAm J Neuroradiol 1999 20:445-56. [Google Scholar]
[11]. Bohring A, Lewin SO, Reynolds JF, Voigtländer T, Rittinger O, Carey JC, Polytopic anomalies with agenesis of the lower vertebral columnAm J Med Genet 1999 87:99-114. [Google Scholar]
[12]. Kaissi AA, Klaushofer K, Grill F, Caudal regression syndrome and popliteal webbing in connection with maternal diabetes mellitus: a case report and literature reviewCases Journal 2008 1:407 [Google Scholar]
[13]. Pandey A, Gupta V, Singh SP, Kumar V, Verma R, Neuropathic ulcers among children with neural tube defects: A review of literatureOstomy Wound Manage 2015 61(2):32-38. [Google Scholar]
[14]. Masquelet AC, Beveridge J, Romana C, Gerber C, The lateral supramalleolar flapPlast Reconstr Surg 1988 81(1):74-81. [Google Scholar]
[15]. Hamdi MF, Khlifi A, Lateral supramalleolar flap for coverage of ankle and foot defects in childrenJ Foot Ankle Surg 2012 51(1):106-09. [Google Scholar]