Dental pathologies cause disruption of oral health, may be a causative factor for maxillary sinusitis and also may be related with systemic diseases like cardiovascular diseases, osteoporosis, gastrointestinal malignancies etc., [1-3]. Moreover, early diagnosis and treatment is important to prevent tooth loss or other complications.
Multidetector Computed Tomography (MDCT) is a widespread method for evaluating paranasal sinuses and nasal cavity in daily practice [4,5]. Axial, sagittal and coronal reformatted images in soft tissue and bone algorithm enable to determine both soft tissue and bone pathologies [4]. In a paranasal sinus CT scan, the whole of the maxillary molar teeth are frequently visible. Anteriorly located maxillary teeth are often partially included in the images [6].
There are 16 teeth in each arch (maxilla and mandible) and they are composed of multiple components [Table/Fig-1]. Crown is covered by enamel which is highly opaque. Dentin and cementum cannot be distinguished by CT. Dentin surrounds the root canal and pulp chamber. Pulp chamber and root canal are most hypodense structures in teeth and contains neurovascular elements [7]. Periodontal ligament is seen as a thin radiolucent layer between the root surface and lamina dura. Teeth are situated in the alveolar process [3]. Teeth have proximal, lingual, occlusal and buccal surfaces.
It is possible to detect dental pathologies with MDCT before they cause symptoms [6]. However, radiologists sometimes do not care enough to evaluate teeth and related pathologies [6,8]. Therefore, this study was conducted to review the pathologies of Maxillary Alveolar Arcus (MAA) in paranasal sinus CT scans and to determine the incidence of dental pathologies and reveal the clinically important ones.
Materials and Methods
A retrospective study was performed in Radiology Department of Balikesir University, Training and Education Hospital, Turkey between December 2014 to June 2015 and consecutive 395 paranasal sinus CT scans were retrospectively evaluated. Patients admitted to outpatient department of hospital for nasal or paranasal sinus problems were included. The CT scans of seven patients with previous facial trauma, operation or invasive tumor history and four patients with repeated exams were excluded. The consent for ethical approval was obtained from the local Ethical Committee before the commencement of study.
All CT images were obtained with 64 detector-scanner (Toshiba Aquillon 64, Otawara, Japan). Axial CT scans obtained from frontal sinus apex to the end of hard palate without contrast administration. Technical parameters were as informed; slice thickness 0.5 mm, spacing 0.3 mm, tube voltage 120 kv, miliampere 150 mA. Average number of slices was 300-350. Sagittal and coronal images in bone algorithm were constituted in workstation (Aquarius Intuition edition ver4.4.7, TeraRecon, CA, USA) in addition to axial images. Window width and window level values were changed to 3500 and 1500HU if necessary, because teeth could be more apparently visualised by changing window width and level values.
All visible parts of maxillary teeth were checked, beginning from the incisors to third molars in the right and left sides, respectively. Firstly, the existence of tooth loss, developmental dental anomalies, dental procedures or instrumentation was evaluated. Then the visible parts of each maxillary tooth (crown, dentin, pulp and roots) were examined for pathologies. Only the roots of incisors could be seen. The visible parts of teeth were gradually increased from anterior to posterior and the whole of molar teeth were evaluated. Bony structure of MAA was also checked for periodontal and periapical diseases.
Detected findings were classified as “tooth loss, dental restorations or procedures and dental pathologies (carious lesions, dental developmental anomalies, periapical lesions and periodontal diseases)”. Radiologic criteria used for classifying dental pathologies were modified according to Textbook of Oral Radiology: Principles and Interpretation, 6th edition by White and Pharaoh [9].
Statistical Analysis
Statistical test applied were in simple percentiles.
Results
Paranasal sinus MDCT scans of 384 patients were included in our study. Two hundred and twenty seven (59%) patients were male, 157 (41%) of them were female. Average age was 45 years old (between 12 and 90). One hundred and ninety five (51%) patients had one or more dental pathologies. Dental restorations or procedures were determined in 129 (33.5%) patients. Thirty four (8.8%) patients had normal teeth count and morphology. Two hundred and sixty four (68.75%) patients had at least one tooth loss.
Periapical lesions and periodontal disease were detected in 46 (11.9%) and 44 (11.4%) patients, respectively [Table/Fig-2,3 and 4].
The ratio of 272 incidental pathologies in maxillary teeth on 384 patients MDCT scans.
| Incidental pathology | n | % |
|---|
| Carious lesions | 104 | 27.0 |
| Developmental anomalies | 78 | 20.3 |
| Periapical lesions | 46 | 11.9 |
| Periodontal disease | 44 | 11.4 |
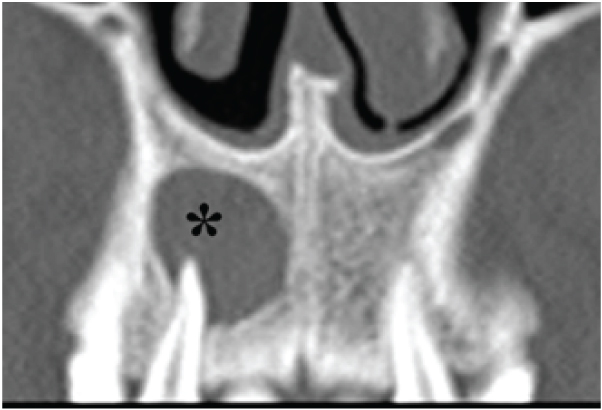
Coronal CT image demonstrates a well-defined periapical lucent lesion (black *) surrounding the root of second maxillary incisor.
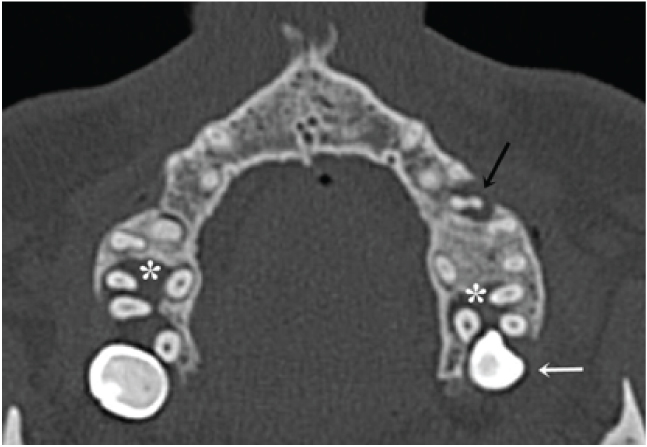
Axial CT image shows the periodontal ligament space enlargement and bone resorption between root furcation around the left premolar (black arrow) and bilateral second molar teeth (white *). The left third molar tooth was (white arrow) impacted.
Carious lesions were the most common dental pathology. One hundred and forty six carious lesions were detected in 104 (27%) patients out of which 64 were proximal caries [Table/Fig-5]. Nineteen carious lesions were in buccal surface, 32 in occlusal surface and four in lingual surface. Twenty seven extensive carious lesions were also seen [Table/Fig-6].
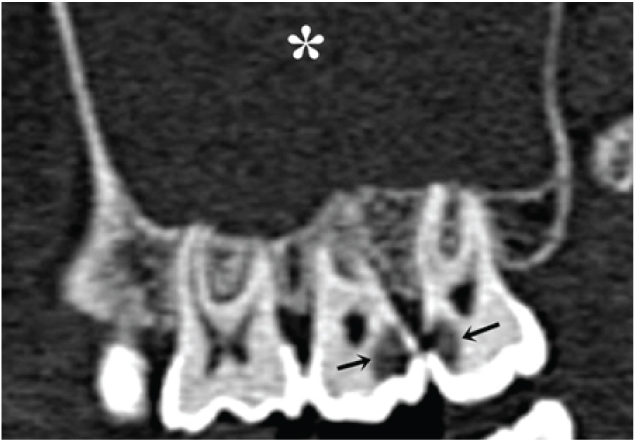
Sagittal oblique CT image demonstrates proximal caries (black arrows) between the 2nd and 3rd molar teeth. Soft tissue density is seen (white *) in the maxillary sinus.
Carious lesion types detected in the study.
| Type | n | % |
|---|
| Proximal caries | 64 | 41.8 |
| Occlusal surface caries | 32 | 20.9 |
| Buccal surface caries | 19 | 12.5 |
| Lingual surface caries | 4 | 2.6 |
| Extensive caries | 27 | 17.6 |
| Total | 146 | 100 |
In addition residual tooth root were detected in 19 (4.9%) patients. Ninety-three dental developmental anomalies were detected in 78 (20%) patients. The most common dental developmental anomaly was impacted molar teeth. Thirty eight impacted molar teeth were seen in 31 (8%) patients. Twenty five premolar and molar teeth with single root, 15 molar teeth root protrusion to maxillary sinus floor, four impacted canine, seven mesiodens, three residual decidual teeth and one four-rooted molar tooth were the other developmental anomalies [Table/Fig-7,8].
Dental developmental anomalies detected in the study.
| Anomalies | n | % |
|---|
| Impacted molar tooth | 38 | 40.9 |
| Premolar or molar tooth with single root | 25 | 26.9 |
| Molar tooth root protrusion into maxillary sinus floor | 15 | 16.1 |
| Mesiodens | 7 | 7.4 |
| Impacted canine | 4 | 4.3 |
| Retained deciduous tooth | 3 | 3.2 |
| Four-rooted molar tooth | 1 | 1.1 |
| Total | 93 | 100 |
Axial CT image shows a mesiodens (white arrow) posterior to the left maxillary incisor teeth. The apex of the mesiodens is between first incisor teeth.

Discussion
Dental pathologies in the maxillary teeth and MAA were detected in more than half of the patients with paranasal sinus CT scans in our study. Many previous studies about incidental findings of maxillofacial region reported in literature [10-15]. The incidental findings at the airways area, temporomandibular joints, soft tissues, paranasal sinuses and teeth were investigated in these studies. Most of them were based on Cone-Beam CT (CBCT) findings. Moreover, in some studies patients were referred to CBCT for dental implications. Our study is different from these studies by some ways. In our study all patients were referred for upper nasal airway and paranasal sinus pathologies evaluation. We focused on the dental pathologies and did not evaluate other regions. In a recent study reported by Steinklein J and Nguyen V et al., dental pathologies encountered on head and neck CT scans were described [15]. However, they did not mention about the incidence of dental pathologies. We could not find a study reporting the incidence of dental pathologies in paranasal sinus CT scans. Dental pathologies were observed in 195 (51%) patients in our study.
A carious lesion is demineralization of dental hard tissues. Bacteria produce lactic acid via carbohydrate fermentation which is responsible for demineralization [16]. It may take long time before caries penetrate the enamel, however, it may spread rapidly in the dentin [6]. Caries may destroy the whole tooth with progression. It is one of most prevalent disease and can be detected by CT [6,15]. A total of 153 carious lesions were detected in 104 (27%) patients in this study. An early carious lesion may be seen in a mushroom shape and an advanced one is ovoid in CT [6]. Dental carious lesions are classified according to localization: occlusal, proximal, lingual and buccal [9]. An early carious lesion which is limited into the enamel usually requires only an interceptive treatment. However, in an advanced carious lesion, the surface is cavitated and a restoration is required [9]. In our study, considerable amount of the dental caries were detected at the proximal surfaces which may be difficult to visualise by physical examination [17]. Incidentally detection of caries at an early stage with paranasal sinus CT may prevent caries progression and tooth loss with appropriate treatment.
Periodontal disease is a common cause of teeth loss [18]. The inflammatory changes in the surrounding soft tissue and bone around the teeth cause destruction of periodontal ligament. The bone loss occurs between the teeth and furcation of the teeth [9]. Decreasing density at the intercrestal bone and widening of the periodontal ligament space can be detected by CT [4]. The periodontal ligament space is normally thin and its width is approximately 0.2 mm or less in CT images [19]. These findings may be evident in severe disease but they are non-specific findings. So, a clinical examination may be advised if periodontal ligament space widening is detected and periodontal disease is suspected in CT [9]. In 44 (11.4%) patients, periodontal disease was suspected with CT findings in our study, however, clinical examination was not performed.
Pulp infections may cause periapical granuloma, cyst or abscess [20]. Periapical lesions were detected in 46 (11.9%) patients and were seen as a lucent lesion around the root apex having similar appearance in CT scans [6,20]. Granulomas are generally smaller than cysts, have ill-defined borders and higher attenuation values in CT [21]. Cysts are usually smaller than 1 cm diameter, well-defined and sclerotic borders [22]. It may not be clinically important to differentiate a small cyst and granuloma. However, cysts may increase in size and cause complications like displacement of roots, resorption of bone and roots and maxillary sinusitis [20]. Ill-defined lucent area with inflammatory changes at the tooth root, surrounding bone and soft tissues in MDCT with clinical findings like pain, facial swelling and fever suggests an abscess [6]. Appropriate treatment and radiological follow-up may be indicated in periapical lesions [23]. Therefore, it may be beneficial to report the periapical lesions which were incidentally detected with paranasal sinus CT.
Developmental dental anomaly is not rare [24]. Developmental dental anomalies were detected in 78 (20%) patients in this study. Tooth impaction is a frequent condition and it is usually detected in the third molars [24]. Impacted canine is second. It is not recommended to extract impacted tooth unless that cause a complication. But impacted teeth can have caries, periodontal bone loss, cyst and tumors. Regular oral examination is recommended to keep asymptomatic impacted third molars in good health [24]. In our study, 31 (8%) patients over 30-years old had impacted third molars. Additionally, four patients (1%) had impacted canines. A mesiodens is a supernumerary tooth located in the incisor region and prevalence is reported between 0.3% and 2.2% [25]. It has usually a conical shape and located inversely in CT [26]. The mesiodens can delay eruption of central incisors; rarely causes root resorption and vitality loss. It is not a rule to extract an incidentally diagnosed mesiodens, however, surgical intervention may be considered to prevent complications like cystic bone changes, root resorption or eruption disturbance of adjacent teeth [9,25]. In our study, mesiodens were detected in 7 (1.82%) patients but there was no sign of complications.
The root and canal number in teeth may vary [27]. These variations can be detected with CBCT and MDCT [28]. Twenty five molar or premolar teeth with single root and one molar tooth with four roots were detected in our study. Identifying the root and canal variations make contribution to choosing the treatment method in endodontic treatment and improve the success [27]. Determining and reporting the canal and root variations incidentally in paranasal sinus MDCT scan may be helpful during management of the affected tooth if that needs treatment.
MDCT is capable of depicting dental pathologies by multiplanar images and thin sections [15]. Also, oblique planar images, three dimensional surface-rendered images and reconstructed dental panoramic images can be obtained by advanced software in bone and soft tissue algorithms which may be helpful for detailed information [6]. MDCT has a capability to detect various dental pathologies like carious lesions, periodontal disease, periapical lesions, cysts, tumors etc. [6,15]. However, MDCT has limitations for dental implications like higher radiation dose and cost [9]. CBCT is a newer and alternative three-dimentional imaging method in dentistry. The lower cost and radiation exposure compared to MDCT are advantages of CBCT [9,13,29]. On the other hand CBCT has limitations like the lack of a soft tissue window and precise Hounsfield units and higher image noise [30,31].
Limitation
Mandibular teeth were not included in the paranasal sinus MDCT so we were not able to collect data of mandibular teeth. Our study was retrospective and we could not perform a dental examination, so we were not able to correlate MDCT findings with clinical findings. Additionally, ratio of dental pathologies may probably change according to socio-economic development of countries. If this study was performed in a developed Eastern country, less dental pathologies could be found.
Conclusion
Dental pathologies such as carious, periapical, periodontal and developmental lesions were encountered in more than half of the patients with paranasal sinus MDCT in this study. Detecting dental pathologies with paranasal sinus CT may prevent tooth loss and improve oral health. The radiologist should keep in mind dental pathologies while evaluating the paranasal sinus CT scans.