Tympanoplasty is a procedure done to repair tympanic membrane and middle ear sound conducting mechanism. Graft materials like temporalis fascia, vein graft, fascia lata and perichondrium are used to seal the perforations [1]. Among these temporalis fascia remains the commonly used graft with success rate of 93-97% [2,3]. However, in cases with poor eustachian tube dysfunction, adhesive otitis media, tympanic sclerosis or total or subtotal perforation, the results with temporalis fascia are poor. In these cases, being tougher, cartilage perichondrium is a better alternative as it provides stability against retraction. In the present study, we used cartilage-perichondrium composite graft in repair of various tympanic membrane perforations and study its functionality and feasibility.
Materials and Methods
It was a cross-sectional, intervention study done at Department of Otorhinolaryngology, SS Institute of Medical Science and Research Centre, Tertiary Care Teaching Hospital, Davanagere, Karnataka, India. This study was done for a period of one year and six months between January 2015 to June 2016. Ethical clearance was taken from the Institutional Ethical Clearance Committee. Written informed consent was obtained from all patients. Patients diagnosed with chronic otitis media-tubotympanic type and getting operated for same were analysed. Revision cases, cases with large, subtotal and total tympanic membrane perforations, perforation with remnant membrane showing tympanosclerotic and atrophic changes and ears with minimum six months of discharge free period were included in the study. Actively discharging ears, cases with active foci of infection in upper respiratory tract and cases medically unfit for surgery were excluded from the study.
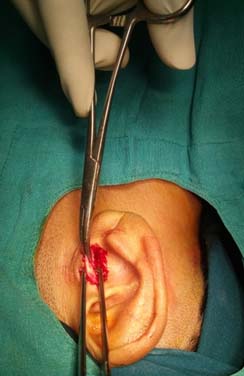
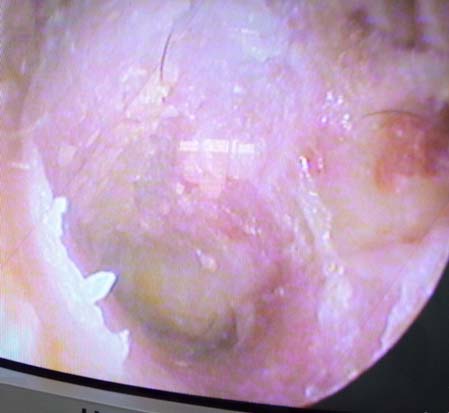
All selected patients were subjected to thorough history and clinical examination, otomicroscopy, otoendoscopy and hearing assessment by pure tone audiometry. X-Ray mastoids were taken in revision cases to rule out mastoid pathology. Post aural approach and underlay technique was employed in all to maintain uniformity. Cartilage perichondrium composite graft was harvested from tragal or conchal cartilage [Table/Fig-1]. It was randomly selected as to which patient to get tragal or conchal cartilage. Cartilage was thinned out with help of number 15 surgical blade with attached perichondrium on one side [Table/Fig-2]. After inspecting the middle ear and the ossicular status, perforation was closed by cartilage-perichondrium composite graft which was placed with bare cartilage side facing the middle ear and perichondrium to the external [Table/Fig-3].
Cartilage graft harvesting from tragal region.


All patients were followed up postoperatively at one week for suture removal and antibiotic ear drops were started. Patients were further followed up at three weeks, three months and six months interval to look for any complications like residual perforation, blunting, lateralisation of graft and graft failure. Each patient was evaluated for hearing improvement six months after the surgery [Table/Fig-4].
Results
In our study, 21 (70%) patients belonged to age group 30 to 50 years and remaining 9 (30%) in 20 to 30 years. 18 patients (60%) were females and 12 (40%) were males in our study. Of 30 cases who underwent Type-1 tympanoplasty, 24 patients (80%) had large central and subtotal perforations [Table/Fig-5]. Five patients had medium central perforation with remnant tympanic membrane showing sclerotic plaque and atrophic changes. Only one patient had a total perforation. The remnant tympanic membrane showed atrophic changes in 16 cases (53%) and sclerotic plaque was seen in 14 cases (46%). In our study, tragal cartilage was used in 17 and conchal cartilage in 13 cases. It was randomly decided which patient gets tragal or conchal cartilage.
Preoperative tympanic membrane status.
| Size of perforation | No. of patients | Percentage |
|---|
| Medium (with sclerotic/atropic changes) | 5 | 16.66% |
| Large | 16 | 53.33% |
| Subtotal | 8 | 26.66% |
| Total | 1 | 3.33% |
| TM changes |
| Sclerosis | 14 | 46.66% |
| Atropic/thin | 16 | 53.33% |
Successful graft uptake was seen in 28 cases (93%) by six months. At three weeks postoperatively, none of the patient showed wound infection or ear discharge. Two patients (7%) had a residual perforation at three months. In both of these cases, conchal cartilage was used. In four cases (13%) the neotympanum showed anterior blunting by the end of six months. Among these tragal cartilage was used in two patients and conchal cartilage in two patients.
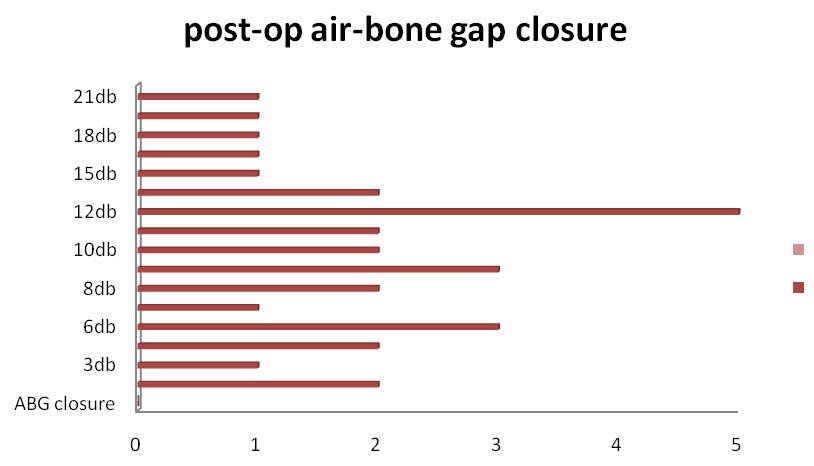
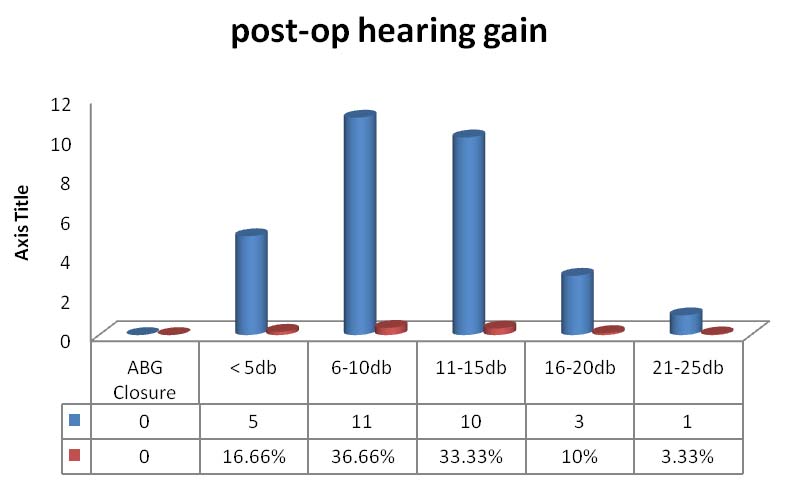
With respect to hearing, postoperative hearing was analysed in different ways. Maximum air bone gap closure achieved in our study [Table/Fig-6] was 21db in one patient and minimum was 3db. Average air-bone gap closure achieved was 10.1db [Table/Fig-7]. Eleven patients had a hearing gain of 6-10db and 10 cases by 11-15db. The average hearing gain in cases with preoperative air bone gap of 10 to 20db was 6.7 db, in 21 to 30 db was 7db, in 31 to 40 db was 13.3 db and in 41 to 50 db was 16.5 db [Table/Fig-8]. This was a considerably good improvement with respect to previous hearing status of the particular cases.
Postoperative air bone gap closure.
Postoperative hearing gain.
Air bone gap closure with respect to preoperative hearing loss.
| Pre-op ABG | Average ABG closure |
|---|
| 10-20db | 6.7db |
| 21–30 db | 7db |
| 31 - 40 db | 13.3db |
| 41 - 50 db | 16.5db |
Discussion
The use of cartilage as a grafting material can be advocated in complex perforations like in cases at high risk for graft failure such as large, subtotal, total perforations, adhesive tympanic membrane, tympanosclerotic and atropic changes of remnant tympanic membrane, recurrent perforations and in cases with chronic eustachian tube dysfunction.
In our study, all the cases had complex perforations with healthy middle ear mucosa. Grafts take up and healing process in tympanoplasty depends on the condition of the middle ear mucosa, remnant tympanic membrane and its ability to epithelise. Cartilage graft is preferred in such situations as it provides stability against negative middle ear pressure preventing its medialisation or lateralisation. Cartilage graft gets its nutrition by diffusion from micro vessels of healing margin of remnant membrane.
At three months, two patients had a residual perforation which could be due to inappropriate size of the graft taken or faulty surgical technique. Four cases had anterior blunting of graft which could again be due to the improper size of the cartilage graft used or postoperative variation in middle ear pressure leading to displacement but, due to higher stability of the cartilage and faster healing, it did not result in complete lateralisation of the graft and residual perforation.
Outcome of cartilage tympanoplasty done by various other authors and studies were analysed and results compared. In reference to those [Table/Fig-9] [2,4-8], graft uptake in our study was similar to other studies and postoperative hearing achieved was similar to few other studies with respect to average air bone gap closure [4,5,7] and postoperative ABG of less than 20db [8].
Graft take up rate and hearing results of the other studies.
| Source of data | No. of patients | Graft material | Graft success rate (%) | Postoperative hearing status (ABG or hearing gain) |
|---|
| Present study | 30 | Cartilage- perichondrium composite graft | 93% | ABG: < 25db in 93% casesABG average: 18db,Average hearing gain: 10.1dbABG: < 20db- 53% (16cases) |
| M Cavaliere et al., [2] | 306 | Cartilage- perichondrium | 99.35% | ABG: <10db in 90% |
| Dornhoffer J [4] | 533 | Perichondrium-cartilage island | 97.6% | ABG: 13.5db, hearing gain: 9.3db |
| Aidonis I et al., [5] | 62 | Cartilage shield | 98.4% | ABG: 24db, hearing gain: 8.4db, <10db-86% |
| Vadiya S et al., [6] | 65 | Cartilage- perichondrium | 98.46% | ABG: 16.23db, < 20db at 6 months: 92.33% |
| Garcia RB et al., [7] | 126 | Cartilage | 71.1% | Hearing gain: 12.8db |
| Chen XW et al., [8] | 102 | Cartilage- perichondrium | 96.1% | ABG: <20db in 55.8% |
The results of the present study suggests that cartilage is an excellent graft material especially when it comes to repair of complex perforations where cartilage-perichondrium graft promises a stable neotympanum and reduces risk of reperforations/retraction and need for revision surgeries.
From various studies and literature search, the advantages of cartilage as a grafting material and its special properties were summarised and following points noted:
The cartilage being stiff is more resistant to negative middle ear prossure [2].
Cartilage is sufficiently elastic for good sound conduction, well tolerated and resistant to resorption [9].
With time cartilage softens and this adds to the hearing improvement over years.
Cartilage slices of less than 0.5 mm thick are similar to the tympanic membrane in their acoustic properties [10].
The extrusion rate of cartilage is very minimal compared to other graft materials.
Limitation
Tragal and conchal cartilages have many differences. This study does not study them separately. It was randomly selected which patient should get either tragal or conchal cartilage. Thickness of the graft used was not measured in our study.
Conclusion
In our study, feasibility of cartilage-perichondrium composite graft in repair of complex tympanic membrane perforations was good with a graft uptake of 93%. Complications like residual perforation and blunting of graft was less with a considerably good hearing outcome. Hence, cartilage-perichondrium composite graft can be considered a good choice in repair of tympanic membrane perforations with specific selective indications.