Malignant Pilomatricoma: A Report of Two Cases and Review of Literature
Anita Flynn1, Anuradha Durga Agastyaraju2, N Sunitha3, Aradhana Harrison4
1 Consultant Pathologist, Department of Pathology, St. Martha’s Hospital, Bengaluru, Karnataka, India.
2 Junior Consultant, Department of Pathology, St. Martha’s Hospital, Bengaluru, Karnataka, India.
3 Senior Registrar, Department of Pathology, St. Martha’s Hospital, Bengaluru, Karnataka, India.
4 Junior Consultant, Department of Pathology, St. Martha’s Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anita Flynn, Central Laboratory, St. Martha’s Hospital, 5 Nrupathunga Road, Bengaluru-560001, Karnataka, India.
E-mail: anitaflynn_cmc@yahoo.com
Malignant pilomatricoma is an extremely rare tumour arising from the hair follicle. About 80 known cases are reported in literature till date. Presented herewith are two cases of malignant pilomatricoma, occurring in young female patients, each with a different clinical presentation and outcome. It is important to be aware of this entity as malignant pilomatricoma, though, initially locally aggressive, can recur if incompletely excised and also can metastasize to lungs, bones and lymph nodes.
Anaplasia, Basaloid cells, Metastases, Tumours of epidermal appendages
Case 1
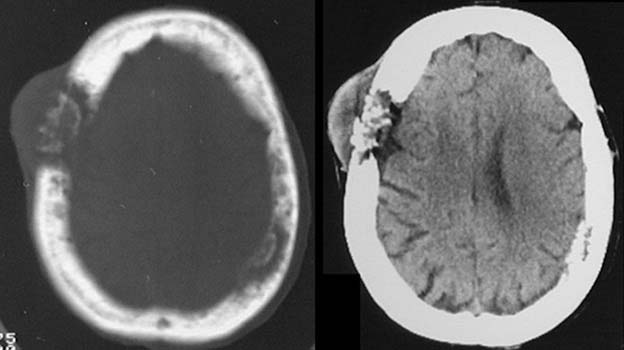
A 24-year-old female presented in casualty with signs of altered sensorium and increased intracranial pressure. On examination, a lobulated swelling measuring 12 x 6 x 7 cm was seen on the scalp in the right temporo-parietal region. Her relative gave a history of a slow growing mass first noticed five years ago. Excision of the mass was done in another hospital 16 months prior to current presentation. Histopathology then was reported as malignant pilomatricoma with involvement of base and margins of specimen. Underlying bone was also involved. The patient refused radiotherapy post-surgery. She now presented at our hospital with recurrence of the tumour. CT scan report showed a malignant tumour invading the skull bones and brain in the cavernous sinus and draining veins [Table/Fig-1]. Laboratory tests including complete haemogram, coagulation profile, routine urine analysis, liver function tests, serum electrolytes, serum creatinine and Blood Urea Nitrogen (BUN) were done. HIV and HBsAg tests were negative. A repeat biopsy was done.
Case 1 - CT scan image of tumour invading skull bone.
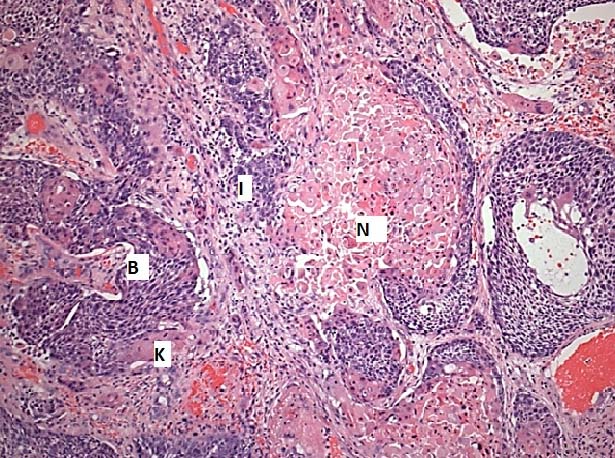
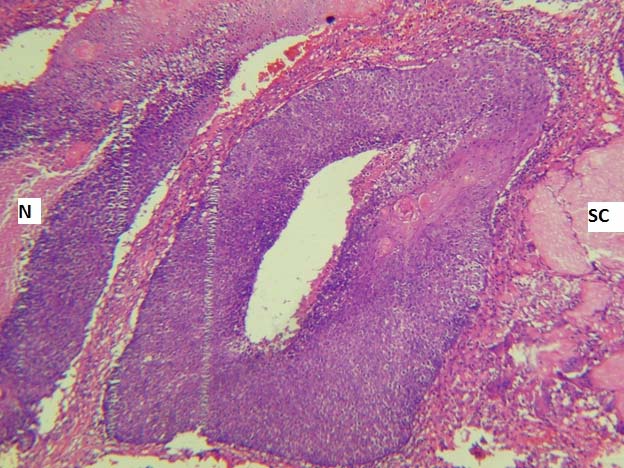
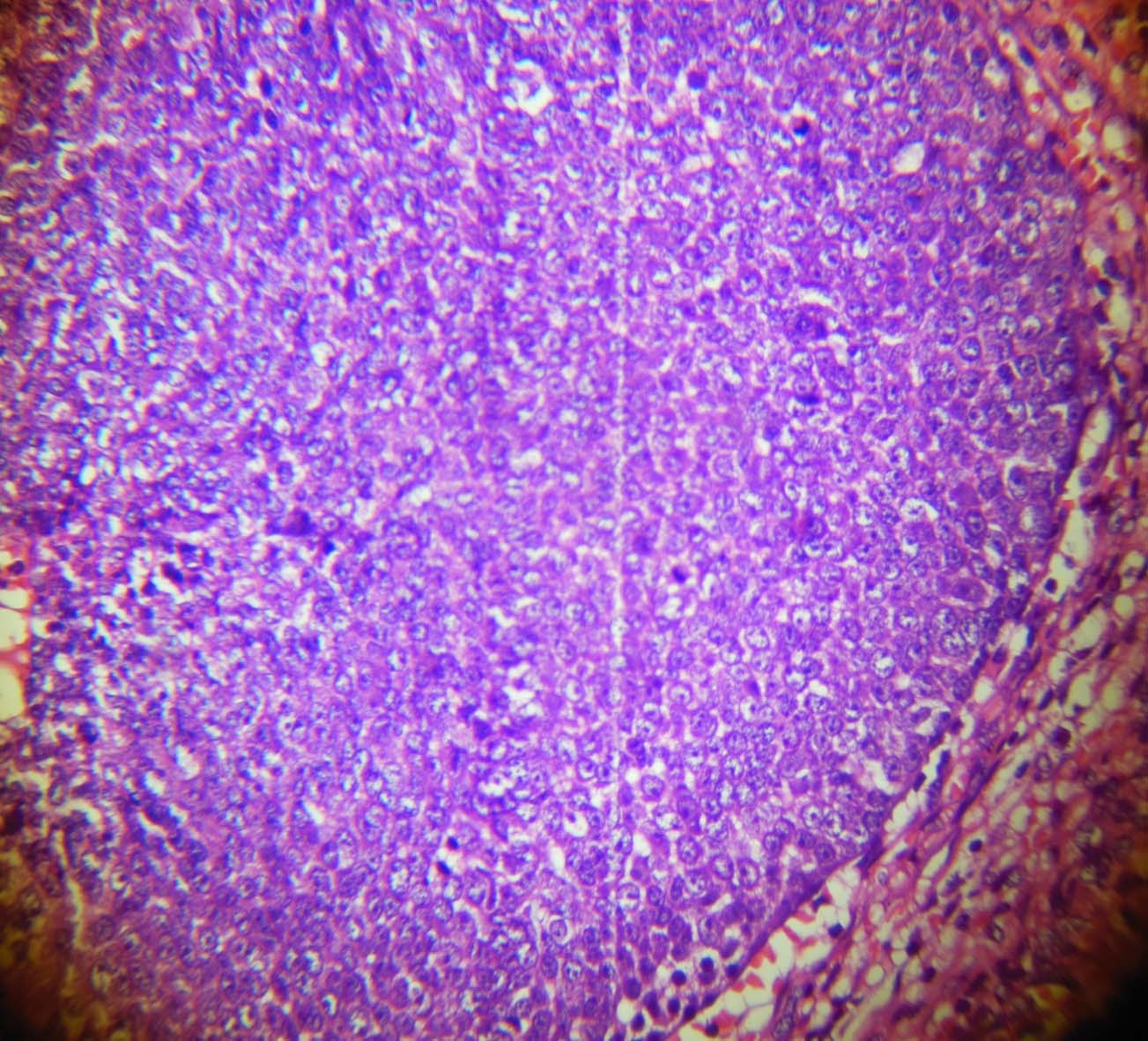
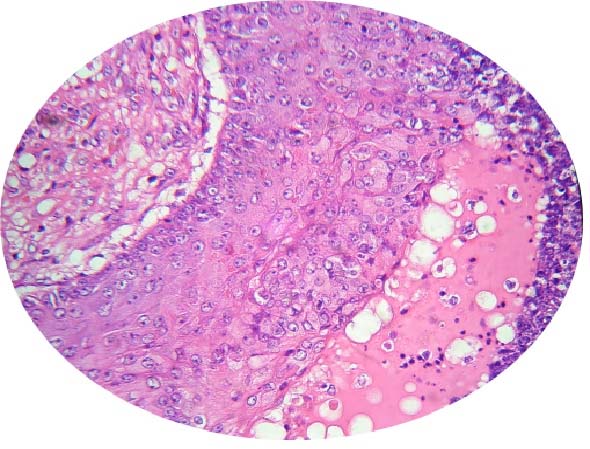
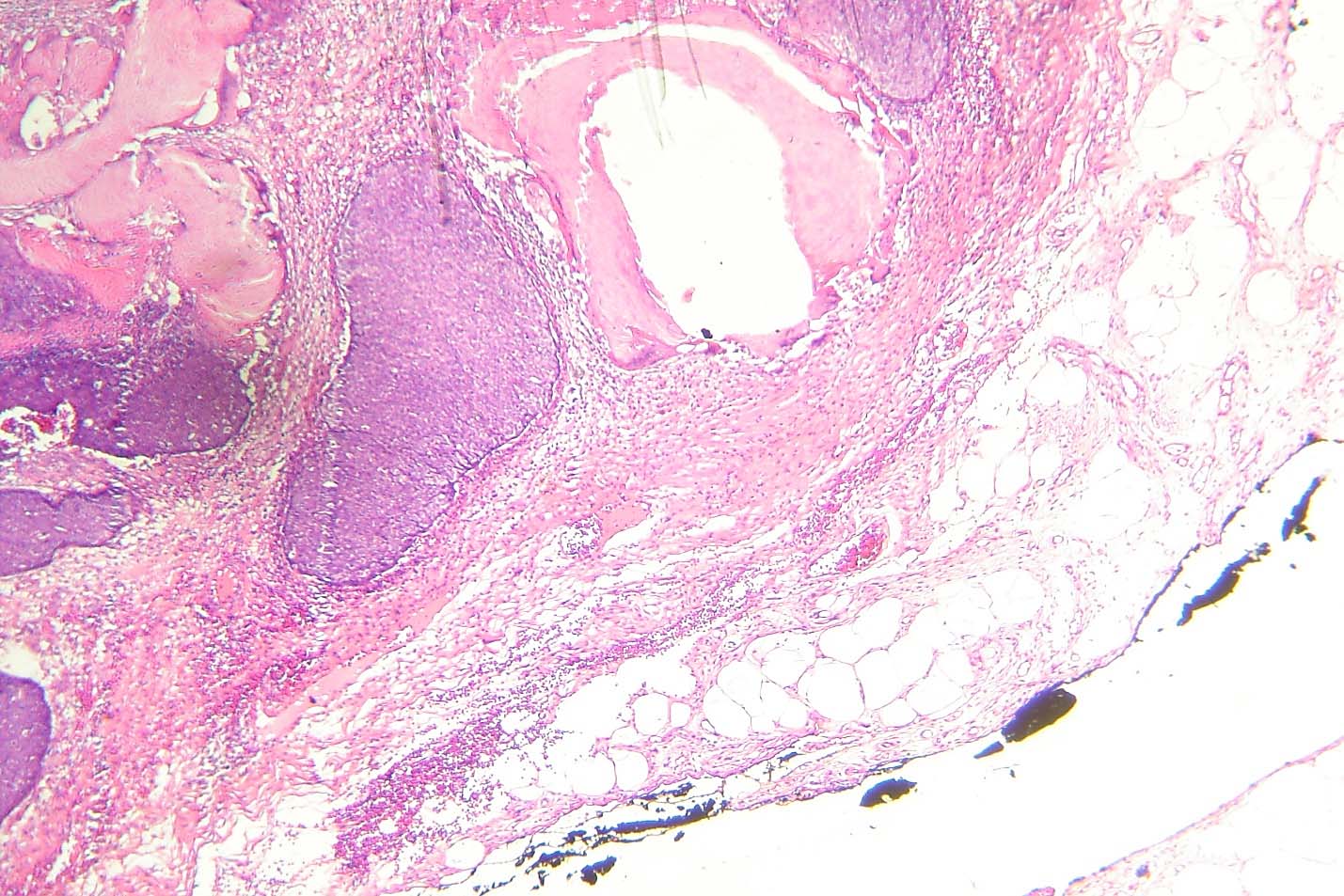
Microscopy showed bits of tissue showing a malignant tumour composed of sheets and nests of neoplastic basaloid cells with infiltrating borders. Tumour was seen at the inked margins of the resected bits. Transition to squamous cells and areas of necrosis were also seen. Mitoses were increased (2-3/HPF). Keratin production, keratin cysts, shadow cells and keratohyaline granules were also present [Table/Fig-2,3]. The diagnosis of malignant pilomatricoma was confirmed. The patient was admitted in Neurosurgery ward and was managed by neurosurgeons and radiotherapists; however, final outcome was fatal.
Case 1 - Masses of hyperchromatic pleomorphic basaloid tumour cells (B) with areas of necrosis (N), keratin (K) and stromal invasion (I) (H&E 10X).
Case 1 - Tumour cell mass with keratin pearls formation showing area of necrosis (N) and mass of shadow cells (SC) (H&E 10 X).
Case 2
A 14-year-old girl came to Surgery Outpatient Department (OPD) with a history of a slow growing painless swelling on the left shoulder since two months. There was no history of trauma. On examination, it was a 2x2 cm, firm, non-tender nodule over the left deltoid. It was superficial and easily mobile. No associated lymphadenopathy was seen. Pre-surgery complete blood count, coagulation profile and HIV and HBsAg tests were done which were within normal limits. The swelling was excised and the tissue was sent for histopathology. The gross specimen was an elliptical skin covered soft tissue piece measuring 2.4 x 1.8 x 1.6 cm with skin surface showing a nodule. Cut section showed a yellowish nodule with cystic areas measuring 1.5 x 1 cm.
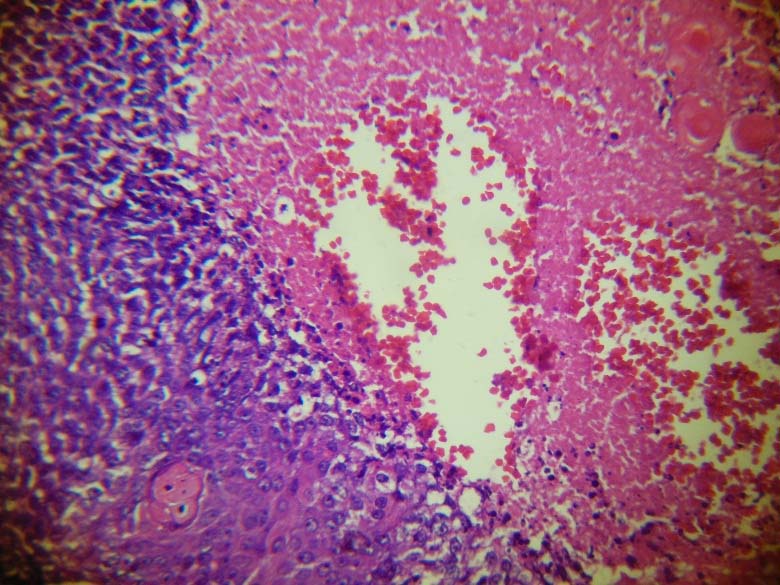
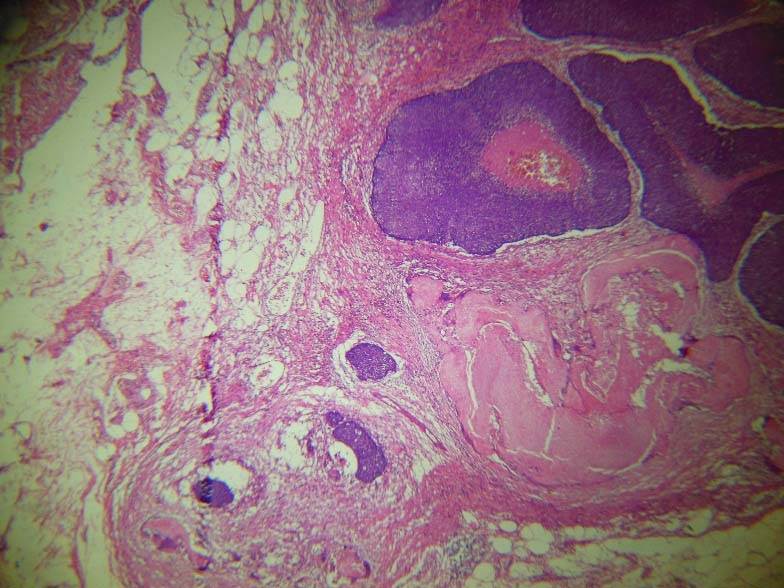
Microscopy revealed a tumour composed of proliferating large anaplastic hyperchromatic basophilic cells with scanty cytoplasm and pleomorphic nuclei with prominent nucleoli and coarse chromatin [Table/Fig-4,5]. Masses of eosinophilic shadow cells, multinucleated giant cells and foci of squamoid transformation were present [Table/Fig-6]. Numerous atypical mitotic figures (3-4/HPF) were seen [Table/Fig-4]. Areas of necrosis [Table/Fig-7] and tumour infiltration into adjacent tissues were noted [Table/Fig-8]. The tumour did not involve overlying skin. There was no evidence of lymphovascular invasion. However, even though the inked surgical margin was free, the tumour was very close to it (0.1 cm away) [Table/Fig-9]. The diagnosis of malignant pilomatricoma was given. Revision of surgical margins was done subsequent to the histopathology report. There was no residual tumour in the resected revised margins sent for histopathology. Subsequent liver function test and serum calcium were within normal limits. Patient is doing well but has been advised regular yearly follow up with chest X-Ray.
Case 2 - Tumour cells showing moderate atypia with prominent nucleoli and numerous mitoses (indicated by arrows) (H&E 40X).
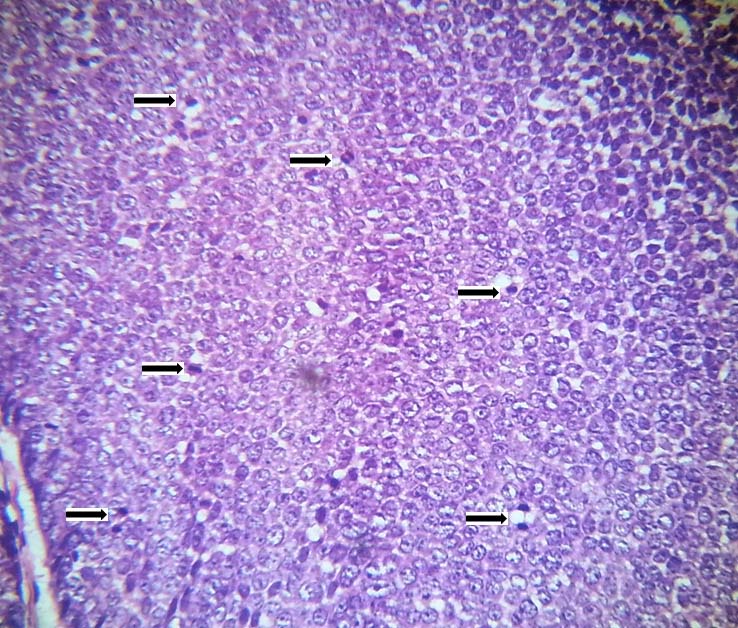
Case 2 -. Masses of hyperchromatic pleomorphic cells with increased mitoses (H&E 40X).
Case 2-Focus of squamoid differentiation (H&E 40X).
Case 2 - Necrosis with karyorrhectic debris (H&E 40X).
Case 2 - Nests of tumour cells showing infiltration into surrounding tissues (H&E 10X).
Case 2 - Inked resected margin free of tumour (H&E 10X).
Discussion
Malignant pilomatricoma is an extremely rare malignant tumour arising from the hair follicle with about 80 cases reported in literature till date [1-3]. It was first described in 1960 [1]. It is a locally aggressive variant of benign pilomatricoma and is regarded as a low grade malignant tumour [4]. It is known to metastasize to lungs, bones and lymph nodes [1]. This lesion occurs in an older age group between sixth and seventh decades. Sex ratio is 5:1 with a male preponderance [4,5]. Both our cases were young females in the second and third decades in contrast to the age incidence in literature. Common sites of occurrence are head and neck, and back [5]. They vary in size from 1-10 cm [5]. They are usually located in the deep dermis – subcutis and have no relation to the epidermis [1]. It is difficult to differentiate clinically between benign and malignant pilomatricoma [6].
Patient must be evaluated for liver function tests and calcium levels. Our first case patient underwent these tests as she came in a moribund state to the hospital. These tests were not done in the second case as it was clinically diagnosed as a sebaceous cyst and hence simply excised as such. Imaging modalities such as chest X-Ray, CT and MRI may be done to evaluate tissue and bone invasion [3].
Grossly, the tumour appears as reddish, firm and lobulated surface [2,6]. On microscopy, scanning magnification shows the tumor to exhibit ulceration, asymmetry, poor circumscription and variably sized basaloid aggregations. The tumour is composed of basaloid cells which show moderate to marked pleomorphism and prominent nucleoli. Atypical mitoses and necrosis are present along with central keratotic material and shadow cells. The tumour nests infiltrate the adjacent tissues. Desmoplasia is present. Vascular or perineural infiltration is not generally observed [7]. Rarely, the basaloid cells may contain melanin pigment in their cytoplasm [2,6,8]. Since there are no well-defined histologic criteria for diagnosis [9], it is a difficult task to distinguish it from conventional pilomatricoma and its variants [aggressive pilomatricoma, proliferating pilomatricoma], matricoma and basal cell carcinoma with matrical differentiation [6]. Immunohistochemistry has no utility, although one study from Japan reports diagnosis of malignant pilomatricoma by antihair keratin antibody [4]. The histopathology report must include the depth of infiltration, presence of necrosis and atypical mitotic figures along with evidence of perineural or vascular invasion [1]. Poorly differentiated tumours with extensive soft tissue infiltration are associated with poor prognosis [1]. Though the first case did not pose any difficulty in diagnosis due to extensive disease and large amount of tissue excised, the second case was challenging as the lesion was small and focus of infiltration was single and tiny. However, keeping the above mentioned points in mind, we were able to confidently give the diagnosis of malignant pilomatricoma.
Malignant pilomatricoma is a locally aggressive low grade malignant tumour. Hence, adequate surgical clearance is essential to prevent local recurrence [6,10]. Metastases to lymph nodes, lung or bone can occur rarely [10]. In spite of its rarity, most authors recommend removal of tumour with an adequate safe margin of 0.5-1.0 cm [1,6,10]. In case of recurrence or residual disease, postoperative radiotherapy is recommended. However, data regarding dosage of radiotherapy and therapeutic outcomes is still under study [3,8]. The role of adjuvant chemotherapy also is unclear [3,8].
Conclusion
Malignant pilomatricoma is a rare entity. The diagnosis of malignant pilomatricoma can be overlooked because of similar overlapping histological features of benign pilomatricoma. Pathologists and clinicians should be aware of it because of its potential for local aggressiveness and distant metastases. Since the diagnosis is mainly morphological, histological evaluation should be meticulous.
[1]. Petit T, Grossin M, Lefort E, Lamarche F, Henin D, Pilomatrix carcinoma: histologic and immunohistochemical features. Two studiesAnn Pathol 2003 23(1):50-54. [Google Scholar]
[2]. Allaoui M, Hubert E, Michels J, Malignant pilomatricoma: two new observations and review of the relevant literatureTurk J Path 2014 30(1):66-68. [Google Scholar]
[3]. Lopansri S, Mihm MC, JrPilomatrix carcinoma or calcifying epithelioma of Mahlerbe: A case report and review of the literatureCancer 1980 45:2368-73. [Google Scholar]
[4]. Tateyama H, Eimoto T, Tada T, Niwa T, Malignant pilomatricoma: An immunohistochemical study with antihair keratin antibodyCancer 2006 69(1):127-32. [Google Scholar]
[5]. Sau P, Lupton GP, Graham JH, Pilomatrix carcinomaCancer 1993 71(8):2491-98. [Google Scholar]
[6]. Hardisson D, Linares MD, Cuevas–Santos J, Contreras F, Pilomatrix carcinoma: a clinicopathologic study of six casesAm J Dermatopathol 2001 23(5):394-401. [Google Scholar]
[7]. Kaddu S, Soyer HP, Hödl S, Kerl H, Morphological stages of pilomatricomaAm J Dermatopathol 1996 18:333-38. [Google Scholar]
[8]. Duarte VM, Sepahdari AR, Abasolo PA, St John M, Pilomatrix carcinoma of the Head and Neck: Case Report and review of the LiteratureInternational Journal of Otolaryngology and Head & Neck Surgery 2012 1:53-56. [Google Scholar]
[9]. Kondo T, Tanaka Y, Malignant pilomatricoma in the parietal regionPathol Oncol Res 2006 12(4):251-53. [Google Scholar]
[10]. Ahern NJ, Fitzpatrick DA, Gibbons D, Collins OD, Armstrong JG, Recurrent malignant pilomatricoma invading the cranial cavity: Improved local control with adjuvant radiationJournal of Medical Imaging and Radiation Oncology 2009 53:139-41. [Google Scholar]