Squamous Cell Carcinoma Penis in a Case of Urethral Stricture Due to Lichen Sclerosus Balanitis Xerotica Obliterans: A Case Report and Review of Literature
Yogesh Taneja1, Priyatama Ram2, Santosh Kumar Dhaked3, Tridib Kumar Sen4
1 DNB Trainee, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Prashantigram, Ananthpur, Andhra Pradesh, India.
2 Senior Resident, Department of Anaesthesia, Sri Sathya Sai General Hospital, Prashantigram, Ananthpur, Andhra Pradesh, India.
3 DNB Trainee, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Prashantigram, Ananthpur, Andhra Pradesh, India.
4 Head, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Prashantigram, Ananthpur, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yogesh Taneja, DNB Trainee, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Prashantigram, Ananthpur, Andhra Pradesh, India.
E-mail: dryogeshtaneja@gmail.com
Penile carcinoma is considered a delayed sequel of lichen sclerosus. It is important to recognize this not so uncommon complication in time as survival of patients with Squamous Cell Carcinoma (SCC) depends on early diagnosis and treatment. We describe a case of a 49-year-old male presenting with urethral stricture due to lichen sclerosus. He was treated for stricture disease and later on developed SCC penis after ten years of presentation.
Meatal stenosis, Partial penectomy, Urethra
Case Report
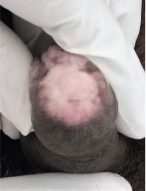
A 49-year-old male presented with a gradually increasing pale growth in preputial skin and nodular indurated lesion on glans for three months. This patient initially presented to us around ten years back at the age of 39 years with obstructive urinary symptoms for past one year. On examination, severe meatal stenosis with Balanitis Xerotica Obliterans changes over glans was observed [Table/Fig-1]. On evaluation, he was found to have pan anterior urethral stricture with a flow of around 1.9 ml per second. Whole of the anterior urethra was laid open with a perineal urethrostomy. No biopsy was taken at that time. Patient was planned for Stage 2 urethroplasty but patient denied as he was happy with perineal urethrostomy. After two years, he developed perineal urethrostomy stenosis which was dilated. He didn’t turn up for follow up for next few years.
Severe meatal stenosis with BXO changes on the glans;
Then he presented at 49 years with a gradually increasing pale growth in preputial skin and nodular indurated lesion on glans for last three months. He was voiding well without any complaints and uroflowmetry was good.
There was no palpable inguinal lymphadenopathy. General and systemic examination was within normal limits. Haematological examination and routine biochemical investigations were within normal limits.
On examination, a pale firm growth in preputial skin, coronal sulcus and adjacent glans localised on both sides of meatus about 1x1 cm in size. The growth was non-tender, appeared free from underlying corpora and was bleeding on touch. He was evaluated and a biopsy of lesion was taken under local anaesthesia. It turned out to be a superficially invasive moderately differentiated SCC.
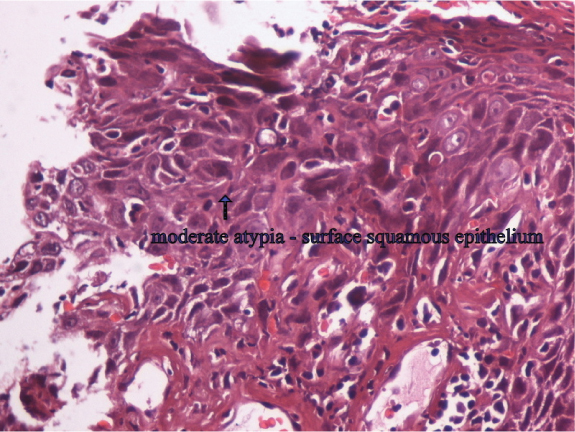
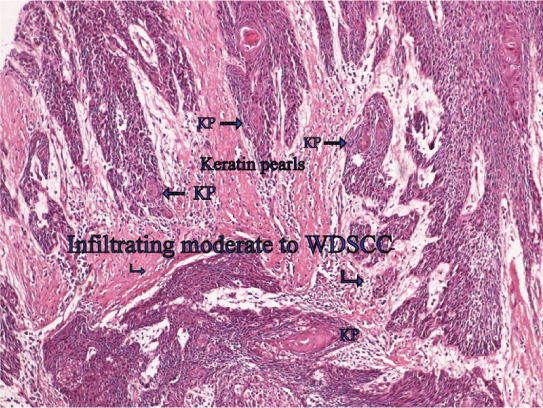
Patient was planned for partial penectomy and surgery done under spinal anaesthesia and specimen sent for histopathological examination [Table/Fig-2,3 and 4]. Histopathology report confirmed the diagnosis as lamina propria invasive moderately differentiated SCC (pT1a) with no lymphovascular invasion and margins were [Table/Fig-5,6]. No lymphadenopathy was seen after six months follow up and there were no signs and symptoms of metastasis.
Cut section of corpora after partial penectomy.

Closed wound appearance after partial penectomy;

Lay open urethra with partial penectomy.

Moderate atypia of the surface squamous epithelium (H&E 40X);
Keratin pearls in moderate to well differentiated SCC (H&E 10X).
Discussion
Lichen Sclerosus (LS) or BXO is a chronic inflammatory condition of skin with unknown aetiology. It was first described by Stuhmer A in 1928 who named it as BXO based on its pathological features [1]. After that many case reports have been published [2-5]. Exact incidence of LS is still unknown with most series reporting a 2.6– 5.8% incidence of penile carcinomas in patients with LS [6-8]. Therefore, it is not possible to say if a patient has LS, he has an increased risk of developing penile carcinoma or not. On the other hand, there is a well documented association between Vulval lichen sclerosus and SCC [9,10]. The reason for this might be relative less incidence of penile carcinoma and a prolonged lag period which makes the association between two difficult.
BXO is a localised genital manifestation of LS with unknown cause but factors like genetic, local trauma, autoimmune disease and infective process have been implicated by some authors as a potential cause [11]. On clinical examination, ivory white plaques involving the glans and prepuce are found. Common presenting complaints include itching, soreness and phimosis. These patients can present with complications like meatal stenosis and urethral stricture. Now the question is whether LS is premalignant or not? The European association of urology [12] has classified LS as a premalignant lesion for SCC of penis. Numerous authors have documented this association. Wallace HJ found that two patients developed SCC after BXO out of 44 patients [13]. Bingham JS reported a case of 39-year-old man developing SCC penis, six years after circumcision for phimosis [2]. Bart RS and Kopf AW have reported synchronous penile LS and SCC [14]. Nasca MR et al., found an incidence of 5.8% in their series of 86 patients with penile LS with a mean time interval of 17 years [6]. Largest series till date was published by Depasquale I et al., with 522 BXO patients, out of which 12 developed SCC [7]. In a series by they found 28% association of BXO and SCC penis. This was although less than what Powell J et al., documented [15]. They found an incidence of 50% but they included only histologically proven cases. Recently, Clouston D et al., has published that the risk of malignant transformation of penile LS is 4-8% [16]. The nature of this relationship is unclear. It is possible that this is merely a phenomenon that occurs when a rare condition, penile carcinoma, arises on the background of a common disease process, BXO. It is unlikely that the association between BXO and penile carcinoma is merely coincidental and thus might reflect a common aetiology.
On the other hand, this is also not the exact incidence. Actual incidence can be low or even higher as true incidence of BXO in community is unknown. The reason is most clinicians don’t follow these cases because of low risk of malignancy considered. There are no clear guidelines for follow up of BXO patients. In contrast, vulval lichen sclerosus has a documented premalignant potential, so the women vulval lichen sclerosus are followed regularly and undergo frequent biopsies [9]. For this reason, some authors recommend routine histological examination of all circumcision specimens and regular follow up [4,7,15]. This will allow early biopsy and a prompt diagnosis of a developing carcinoma.
The clinician should have a low threshold for doing biopsy in an uncircumcised BXO patient and in patients in whom glans BXO persists even after circumcision. In all clinically indicated circumcisions for BXO, specimens should be sent for histological examination.
Conclusion
In conclusion, the premalignant nature of BXO has been confirmed by many studies and a close association with penile carcinoma is seen. In this case if the biopsy could have been taken earlier or the patient would have been on regular follow up this case would have been diagnosed earlier.
[1]. Pietrzak P, Hadway P, Corbishley CM, Watkin NA, Is the association between balanitisxeroticaobliterans and penile carcinoma underestimated?BJU International 2006 98(1):74-76. [Google Scholar]
[2]. Bingham JS, Carcinoma of the penis developed in lichen sclerosus et atrophicusBr J Vener Dis 1978 54(5):350-51. [Google Scholar]
[3]. Weigand DA, Lichen sclerosus et atrophicus, multiple dysplastic keratoses, and squamous-cell carcinoma of the glans penisJ Dermatol Surg Oncol 1980 6(1):45-50. [Google Scholar]
[4]. Liatsikos EN, Perimenis P, Dandinis K, Kaladelfou E, Barbalias G, Lichen sclerosus et atrophicus. Findings after complete circumcisionScand J Urol Nephrol 1997 31(5):453-56. [Google Scholar]
[5]. Singh RP, Mahmood K, Gunjan K, Garg A, Tiwari R, A rare case report of squamous cell carcinoma of urethra arising from substituted penile skin flap with balanitis xerotica obliteransJ Evolution Med Dent Sci5:Issue 48/eISSN-2278-4802, pISSN-2278-4748/ [Google Scholar]
[6]. Nasca MR, Innocenzi D, Micali G, Penile cancer among patients with genital lichen sclerosusJ Am Acad Dermatol 1999 41(6):911-14. [Google Scholar]
[7]. Depasquale I, Park AJ, Bracka A, The treatment of balanitis xerotica obliteransBJU Int 2000 86(4):459-65. [Google Scholar]
[8]. Barbagli G, Palminteri E, Mirri F, Guazzoni G, Turini D, Lazzeri M, Penile carcinoma in patients with genital lichen sclerosus: A multicenter surveyJ Urol 2006 175:1359-63. [Google Scholar]
[9]. Scurry J, Does lichen sclerosus play a central role in the pathogenesis of human papillomavirus negative vulvar squamous cell carcinoma? The itch-scratch-lichen sclerosus hypothesisInt J Gynecol Cancer 1999 9(2):89-97. [Google Scholar]
[10]. Neill SM, Lessana-Leibowitch M, Pelisse M, Moyal-Barracco M, Lichen sclerosus, invasive squamous cell carcinoma, and human papillomavirusAm J Obstet Gynecol 1990 162:1633-34. [Google Scholar]
[11]. Powell JJ, Wojnarowska F, Lichen sclerosusLancet 1999 353(9166):1777-83. [Google Scholar]
[12]. Hakenberg OW, Compérat E, Minhas S, Necchi A, Protzel C, Watkin N, Penile CancerEuropean Association of Urology 2014 Available from: http://uroweb.org/guideline/penile-cancer/ [Google Scholar]
[13]. Wallace HJ, Lichen sclerosus et atrophicusTrans St Johns Hosp Dermatol Soc 1971 57(1):9-30. [Google Scholar]
[14]. Bart RS, Kopf AW, Tumour conference No 18: Squamous-cell carcinoma arising in balanitis xerotica obliteransJ Dermatol Surg Oncol 1978 4(8):556-58. [Google Scholar]
[15]. Powell J, Robson A, Cranston D, Wojnarowska F, Turner R, High incidence of lichen sclerosus in patients with squamous cell carcinoma of the penisBr J Dermatol 2001 145(1):85-89. [Google Scholar]
[16]. Clouston D, Hall A, Lawrentschuk N, Penile lichen sclerosus (balanitis xerotica obliterans)BJU Int 2011 108(Suppl 2):14-19. [Google Scholar]