COPD is a progressive life threatening lung disease that causes breathlessness and predisposes to exacerbations and serious illness [1]. It is a major cause of morbidity and mortality across the globe. Unfortunately, COPD is characterized by a persistent reduction of airflow and is not a curable disease; though treatment can relieve symptoms, improve quality of life and reduce the risk of death [1]. According to World Health Organization (WHO) estimates, 65 million people have moderate to severe COPD and the prevalence is likely to increase in coming years due to higher smoking prevalence and aging populations in many countries [1]. More than three million people died of COPD in 2015 corresponding to 5% of all deaths globally and it is estimated to be the third leading cause of death by 2030 [1]. Almost, 7% death and 3% Disability Adjusted Life Years (DALYs) of our country can be attributed to COPD [2,3].
In 2005, India had the highest loss in potentially productive years of life worldwide [4]. Around 30 million COPD patients reside in India [5]. Total annual mortality due to COPD is the highest in India [6]. COPD is also an important economic burden on the patient and the health care infrastructure of the country and it has been estimated that each patient spends nearly 30 percent on disease management [2]. In India, lack of awareness about the disease, poor adherence to both national and international treatment guidelines, and problems in the diagnosis, management and follow up results in increased mortality than the developed nations [7].
In the tertiary health care facility where the study was carried out, it was observed that many COPD patients did not come for regular follow up. In these patients, treatment interruption may lead to increased morbidity and mortality. Considering the disease burden of India, lack of data on various aspects of COPD in the study area, the present study was carried out. This study aimed to find out the reasons for defaulting follow up and treatment in COPD patients.
Materials and Methods
A follow up study was conducted for a period of six months during September 2012 to February 2013 after obtaining ethical clearance. All patients attending the TB Chest OPD of the Guru Govind Singh Government Hospital in Jamnagar, Gujarat, India, during the study period, who were already diagnosed of having COPD, were included in the study if they gave their consent after fully understanding that they would be contacted or followed-up during the study. The contact number and address of these patients were taken so that they could be tracked within two weeks in case of turning defaulter. Patients who refused to give their contact address were excluded from the study. All 200 patients who met the inclusion criteria and who attended the OPD during the study period were recruited in the study. Data on patient’s sociodemographic profile, severity of disease and reasons for defaulting follow up and treatment was collected by personal interview by the researchers using a pre-designed, pre-tested, semi-structured questionnaire, detailed patient history was taken and clinical examination was performed. Patients were first identified and then classified into Group A (low risk, less symptoms), Group B (low risk, more symptoms), Group C (high risk, less symptoms) and Group D (high risk, more symptoms) according to latest GOLD guidelines updated in 2011 [8]. GOLD guidelines are based on modified British Medical Research Council (mMRC) breathlessness scale- a validated questionnaire grade for severity of breathlessness, Pulmonary Function Test (PFT) or airflow limitation and numbers of exacerbations in last one year [8].
Exacerbations was defined as an acute event characterized by worsening of patient’s respiratory symptoms that is beyond normal day to day variations and lead to change in medication (Low risk <1 episode per year, High risk >1 episode per year) [9]. For the present study, defaulter was defined as a patient who did not turn for follow up at least two weeks after the given appointment date. The reasons for default rate were determined when they came at a later date or after being tracked by the collected contact details taken at the time of the first interview.
Statistical Analysis
Data obtained were entered in Microsoft Excel 2007 and analysed using Chi-square test. A p-value of <0.05 was considered to be statistically significant.
Results
In the present study, a total of 200 COPD patients attending the TB Chest OPD were recruited. More than two-third of the study subjects i.e., 174 (87%) were males and 26 (13%) were females making the male:female ratio 6.69:1. The mean age of the participants was 59.38 years, ranging from 42 to 79 years. All the patients enrolled in the study were literate. A total of 163 (81.5%) of the patients had up to primary level education and 37 (18.5%) to secondary level or higher. A total of 177(88.5%), 21(10.5%) and 2 (1%) of the patients belonged to the lower, middle and upper socio-economic class respectively.
The patients were classified according to GOLD standard 2011 guidelines into Group A (low risk, less symptoms), Group B (low risk, more symptoms), Group C (high risk, less symptoms) and Group D (high risk, more symptoms) and it was observed that 22 (11%), 51(25.5%), 83 (41.5%) and 44 (22%) of the study subjects belonged to the respective groups.
Out of all the patients enrolled, 64 (32%) turned out to be defaulters. Twenty eight (43.75%) of the defaulters did not turn up at all and had to be tracked while the rest turned up within two weeks of default. Fifteen (23.43%), 9 (14.06%), 14 (21.88%) and 26 (40.63%) of the defaulters belonged to GOLD groups A, B, C and D respectively.
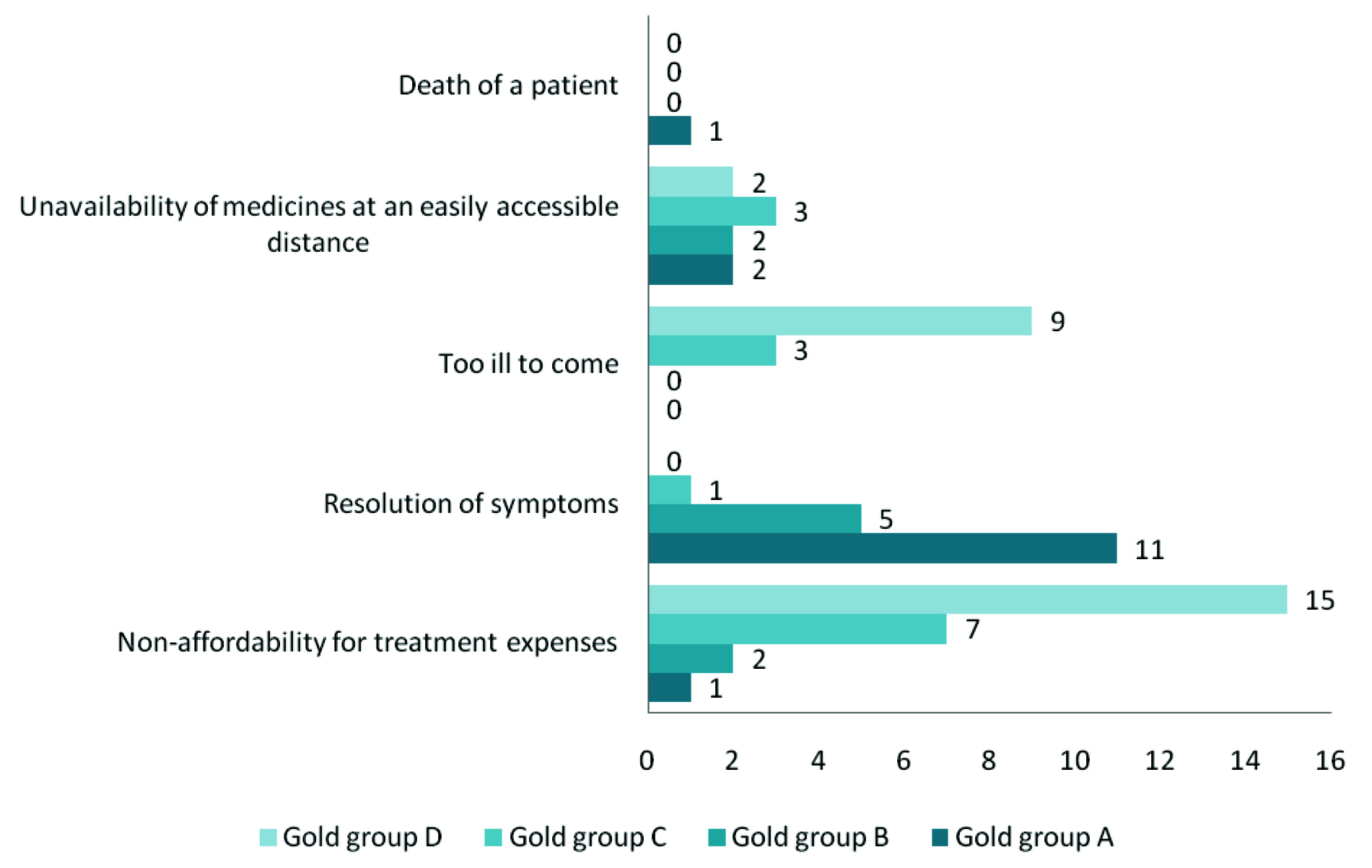
The reasons for default were non-affordability for treatment expenses 25 (39.07%), resolution of symptoms 17 (26.56%), severe illness i.e., too ill to come 12 (18.75%), unavailability of medicines at an easily accessible distance 9 (14.06%) and also, death of a patient 1 (1.56%) [Table/Fig-1].
Distribution of participants according to reasons for default.
There was no significant association between defaulter status and age or sex of the patient [Table/Fig-2]. However, defaulter status was significantly associated with monthly income of the family and educational status of the patient. It was seen that default status was significantly associated with Group A (low risk, less symptoms) and Group D (high risk, more symptoms) [Table/Fig-3].
Association between patient characteristics and default status.
| Variables | Defaulter | Non-defaulter | Total | Chi-square | p-value |
|---|
| Age (in completed years) |
| ≤60 | 28 | 61 | 89 | 0.02 | 0.88 |
| >60 | 36 | 75 | 111 |
| Gender |
| Male | 57 | 117 | 174 | 0.14 | 0.71 |
| Female | 7 | 19 | 26 |
| Monthly income of the family (median monthly family income was Rs. 10000) |
| ≤10000 | 62 | 115 | 177 | 5.33 | 0.02* |
| >10000 | 2 | 21 | 23 |
| Educational status of the patient |
| Up to secondary level | 62 | 101 | 163 | 13.29 | 0.0003** |
| Above secondary level | 2 | 35 | 37 |
p-value= Statistically significant,
p-value= Highly statistically significant
Distribution according to GOLD group and default status.
| GOLD Group | Defaulter | Non-defaulter | Total | Chi-square | p-value |
|---|
| A | 15 (23.43%) | 7 (5.14%) | 22 (11%) | 41.12 | <0.001* |
| B | 9 (14.06%) | 42 (30.88%) | 51 (25.5%) |
| C | 14 (21.88%) | 69 (50.73%) | 83 (41.5%) |
| D | 26 (40.63%) | 18 (13.26%) | 44 (22%) |
| Total | 64 (100%) | 136 (100%) | 200 (100%) |
p-value= Highly statistically significant
Discussion
In the current study, it was observed that a high proportion of COPD patients (32%) turn defaulter. This was higher than in the study by Fischer MJ et al., where 23% of the COPD patients did not complete the rehabilitation course [10]. However, this was comparable to the findings of Sabit R et al., where overall 52 patients (65%) attended all 18 sessions making the defaulter rate 35% [11]. Almost half (43.75%) of the defaulters did not turn up in the subsequent two weeks either and had to be tracked to probe about the reason of default.
In this study, 23.43%, 14.06%, 21.88% and 40.63% of the defaulters belonged to GOLD Groups A, B, C and D respectively. It was observed that the default status was significantly associated with GOLD Group A and Group D. The major reasons for default were non-affordability for treatment expenses (39.07%), resolution of symptoms (26.56%), and severe illness (18.75%). These reasons were similar to those given by the patients in other studies which were medical reasons like exacerbations and hospitalisations and inaccessibility [10,11].
In the present study a high male preponderance of 87% was observed and the male:female patient ratio was 6.69:1. This may be due to higher prevalence of COPD in man (2% to 22%) as compared to women (1.2% to 19%) [12]. This was higher than the recent community-based study conducted in Delhi where 54% of the patients were male. However, the difference may be due to the fact that this was a hospital-based study and health seeking behaviour has been observed to be lesser in Indian females [13]. The age of the recruited patients ranged from 42 to 79 years patients with a mean age was 59.3 years and this is the typical age of COPD onset [2]. This was comparable to study done by Sinha B et al., in Delhi where the mean age of the study participants was 46±13 years [13]. In the present study, the associations between default rate and demographic variables like age and gender were not found statistically signifcant. In the present study, the literacy rate was 100%. This was higher than the 86% literacy of the study by Sinha et al., [13]. Majority of the study subjects (88%) belonged to the lower socio-economic class and a negligible 1% to the upper. In Sinha’s study, most belonged to the lower (46%) and middle (33%) socio-economic class too; however the proportion in the present study is much higher [13]. It was observed, in the present study, that defaulter status was significantly associated with monthly income of the family and educational status of the patient.
This study elicits the various factors influencing COPD patients turning into defaulters. The results can be used by physicians, social workers, counsellors and even policy makers to reduce the morbidity and mortality caused by COPD in India. However, further research needs to be conducted in this regard as the results of the present hospital-based study might not be generalized because of less sample size and absence of baseline data.
Conclusion
It is unfortunate that though COPD is a preventable and treatable disease, it continues to be major public health problem in both the developing and developed nations. It is of great concern that as high as 32% of the COPD patients in the present study had abruptly stopped taking treatment. It was found that the main reasons for default were non-affordability of treatment expenses and worsening of health among GOLD Group D patients and resolution of symptoms among GOLD Group A patients which points out that immediate attention should be given to lessening out of pocket expenditure in these patients as well as increasing awareness about the disease and accessibility to the treatment among the patients.
*p-value= Statistically significant,
**p-value= Highly statistically significant
*p-value= Highly statistically significant