Cellular Fibroma of Ovary Coexisting with Proliferative Endometrium Post Menopause: A Rare Presentation
Vandana Mohapatra1, Susama Patra2, Mamita Nayak3, Radhamohan Gharei4, Nibedita Sahoo5
1 Senior Resident, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha, India.
2 Additional Professor and Head, Department of Pathology and Laboratory Medicine, All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha, India.
3 Senior Resident, Department of Pathology and Laboratory Medicine, All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha, India.
4 Senior Resident, Department of Pathology and Laboratory Medicine, All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha, India.
5 Senior Resident, Department of Pathology and Laboratory Medicine, All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vandana Mohapatra, Senior Resident, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences (AIIMS), Sijua, Bhubaneswar-751019, Odisha, India.
E-mail: mohapatravandana@yahoo.in
Ovarian fibromas are benign sex cord stromal tumours occurring in peri-menopausal and post-menopausal women. These tumours are composed of spindle fibroblastic cells producing collagen. They are almost always endocrine-inert and are rarely associated with hormone production. We report herein a case of a 60-year-old Indian woman presenting as post-menopausal bleeding. Imaging studies and endometrial biopsy revealed a right ovarian solid tumour coexisting with thickened proliferative endometrium, other causes of hyperoestrogenism being excluded in the woman. She underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy. Histopathology showed cellular fibroma of right ovary and proliferative endometrium with foci of hyperplasia without atypia.
Oestrogenic manifestations, Ovarian tumour, Postmenopausal bleeding, Sex cord stromal tumours, Thickened endometrium
Case Report
A 60-year-old postmenopausal woman presented to the outpatient department with complaint of bleeding per vaginum since past five days. The blood flow was moderate in amount. She had attained menopause twelve years back and gave no history of abnormal genital bleeding in the past. There was no history of intake of hormone replacement therapy. She was para three with all vaginal deliveries. There was no history of any comorbid illness or surgical intervention in the past. General examination was unremarkable. Her body mass index was within normal range. Abdomen was soft, non-tender with no palpable mass or free fluid. Cervix and vagina were healthy on per speculum examination. On bimanual examination, uterus was normal in size, anteverted, firm and mobile with a 3 x 3 cm firm, well-defined, non tender adnexal mass felt in the right fornix. Bilateral breast examination was normal.
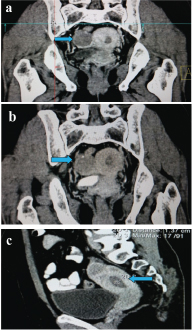
Routine blood investigations and thyroid function tests were within normal limit. Serum CA-125 was normal (14.10 U/ml). PAP smear was negative for intraepithelial lesion or malignancy. Ultrasonography showed increased endometrial thickness (13.5 mm) and a right ovarian complex mass of size 4 x 3 cm. On contrast enhanced computed tomography, a homogenous solid right ovarian tumour measuring 4 x 3 x 3 cm3 was present which showed delayed enhancement on contrast administration [Table/Fig-1a-c]. Endometrial biopsy revealed proliferative endometrium.
a) CECT showing homogenous, solid, well-defined right ovarian mass; b) Delayed phase showing enhancement after contrast administration; c) Thickened endometrium on CECT.
The woman underwent exploratory laparotomy. Intraoperative findings included right ovarian tumour with intact capsule; uterus, left ovary and bilateral tubes appeared healthy except for a small fundal myoma of 2 cm. Peritoneal washings taken were negative for malignant cells. Pouch of Douglas, paracolic gutter, omentum, intestinal surface, peritoneum, other pelvic and abdominal viscera were free of tumour deposits. Retroperitoneal lymph nodes were not enlarged. Total abdominal hysterectomy with bilateral salpingo-oophorectomy was done.
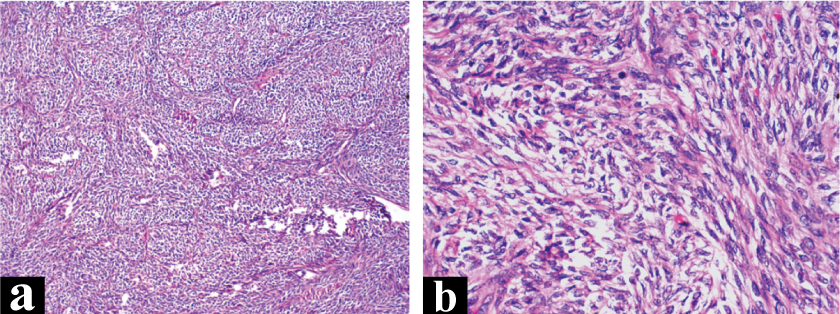
Grossly, right ovary was firm and enlarged to 4.5 x 3.5 x 3.5 cm3. Outer surface was smooth, glistening with intact capsule [Table/Fig-2]. Its cut section was solid, greyish white to greyish yellow with no cystic areas. Endometrial thickness was 0.1 cm. Histopathology showed cellular fibroma of right ovary with average mitotic rate of 2/10 high power fields [Table/Fig-3a,b]. Endometrium was proliferative with foci of hyperplasia without atypia [Table/Fig-4]. Postoperative recovery was uneventful and the woman was discharged on the seventh postoperative day. She is now on follow up and doing well for the past eighteen months post surgery with no complaints.
Cut open uterus with fundal myoma and right ovarian tumour with intact capsule.

a) Photomicrograph showing ovarian cellular fibroma composed of interlacing bundles and fascicles of spindle cells; H&E X 100; b) Nuclei are plump to elongated with a rim of pale eosinophilic to vacuolated cytoplasm; average mitotic rate 2/10 HPF; H&E X 400.
Photomicrograph of proliferative endometrium with foci of hyperplasia without atypia; H&E X 200.

Discussion
Ovarian fibromas are benign sex cord stromal tumours occurring in peri-menopausal and post-menopausal women. They comprise approximately 4% of all ovarian neoplasms [1]. They are derived from the coelomic epithelium or the mesenchymal cells of the embryonic gonads.
They are usually unilateral; less than 5% cases are bilateral [2]. They are often large with a mean tumour size of 8 cm, with only one-third of them being smaller than 3 cm. Grossly, the tumours are solid in majority of cases with cystic component in one-third of them. On histopathological examination, ovarian fibromas comprise spindle shaped fibroblastic cells producing collagen [1]. Approximately 10% of fibromas are classified as Cellular Fibromas (CF). Cellular fibroma is characterized by densely packed bland nuclei with 1 to 3 mitoses per 10 high-power fields and minimal nuclear atypia [2,3]. These tumours display uncertain malignant potential. Ovarian surface adhesions, involvement of the ovarian surface or both, were present in 6% of CFs. Extraovarian involvement was seen in 11% [4]. Local recurrence can occur occasionally even 10 years from initial surgery, particularly in cases of rupture, incomplete excision or adherent disease thus warranting long term follow up for patients with CFs [5].
The mean age of patients with cellular fibromas is 51 years [4]. Ovarian fibromas are usually asymptomatic with non specific clinical signs and may be incidentally detected on routine gynaecological examination or ultrasound in postmenopausal women. If symptomatic, patients usually present with abdominal pain, abnormal uterine bleeding or rarely adnexal torsion [6,7]. They are often misdiagnosed with uterine myomas on ultrasonography or mistaken for malignant ovarian tumours because of the solid nature of the tumour, increased tumour marker levels and ascites [8].
Unlike other sex cord-stromal tumours, ovarian fibromas are almost always endocrine-inert. They arise from non-functioning stroma and rarely show oestrogenic activity. Chechia A et al., in their series of ovarian fibromas and fibrothecomas, reported no endocrine activity in these tumours [1]. However, occurrence of ovarian tumour in women presenting with postmenopausal genital bleeding and endometrial thickening on sonography, raises the suspicion of oestrogen secretion by the ovarian tumour. The histological finding of proliferative endometrium or endometrial hyperplasia further suggests persistent unopposed oestrogen stimulation. Low levels of endogenous oestrogen in postmenopausal women can stimulate the endometrium sufficiently enough to cause bleeding but not endometrial proliferation [9]. In our case, ovarian cellular fibroma coexisted with thickened proliferative endometrium; no other cause of hyperoestrogenism was found in the woman. This raises question regarding the functional activity of ovarian cellular fibroma. Postmenopausal bleeding with thickened endometrium has been seen in association with ovarian fibromas, however, endometrial biopsy revealed either normal or atrophic endometrium [10]. In a retrospective analysis of 98 cases of ovarian fibroma, one was associated with carcinoma of endometrium and endometrial hyperplasia, thus emphasizing the importance of identifying these tumours as functioning [11]. High oestrogen secretion has earlier been demonstrated in postmenopausal non-functioning tumours particularly epithelial ovarian tumours, possibly as a result of stromal stimulation [12]. We present this case as ovarian cellular fibroma has rarely been linked to endocrine activity in postmenopausal women. Nevertheless, the source of oestrogen overproduction and its mechanism at molecular level needs to be explored in future studies.
There are limited specific markers for accurate preoperative diagnosis of ovarian fibromas [13]. On sonography, the solid components were isoechoic or hypoechoic compared to the uterus. They usually appear as a homogeneous solid tumour on computed tomography scan with varying degrees of enhancement after contrast injection [14]. Calcification, myxoid or cystic degeneration may occur, resulting in a heterogeneous pattern. Majority lesions show an isointense signal compared to the myometrium on T1-weighted MRI and hypointense signal on T2- weighted images [15]. CA-125 value was usually normal.
Surgery is the treatment of choice for ovarian fibromas; salpingo-oophorectomy should be done in perimenopausal and post menopausal women and resection of the tumour only can be performed in women desirous of future fertility [8]. Prognostic factors include capsule intact/rupture and completeness of excision [4]. Ovarian fibromas are generally associated with a good prognosis. Minimal-access surgery is an option in small to moderate sized tumours [6]. Laparoscopy has significant advantages of few postoperative adhesions, quicker return of bowel function and shorter hospital stay duration [7,8].
Conclusion
Ovarian fibromas may rarely show endocrine activity possibly as a result of stimulation of underlying ovarian stroma to produce oestrogen. This in turn can stimulate endometrial proliferative activity and cause postmenopausal bleeding as seen in our case. Thus, ovarian fibromas though underdiagnosed preoperatively, should be considered in the differential diagnosis of postmenopausal bleeding with adnexal mass besides keeping in mind the well-known hormonally active tumours. This knowledge is important as timely surgical removal of tumour would result in remission of symptoms of irregular vaginal bleeding as well as would prevent adverse effects of prolonged unopposed oestrogen stimulation postmenopause.
[1]. Chechia A, Attia L, Temime RB, Makhlouf T, Koubaa A, Incidence, clinical analysis, and management of ovarian fibromas and fibrothecomasAm J Obstet Gynecol 2008 199:473.e1-4. [Google Scholar]
[2]. Kurman RJ, Carcangiu ML, Herrington CS, Young RH, WHO classification of tumours of female reproductive organs 2014 4th edLyonIARC [Google Scholar]
[3]. Prat J, Scully RE, Cellular fibromas and fibrocarcomas of the ovary: a comparative clinicopathologic analysis of seventeen casesCancer 1981 47:2663-70. [Google Scholar]
[4]. Irving JA, Alkushi A, Young RH, Clement PB, Cellular fibromas of the ovary: a study of 75 cases including 40 mitotically active tumours emphasizing their distinction from fibrosarcomaAm J Surg Pathol 2006 30(8):929-38. [Google Scholar]
[5]. Adad SJ, Laterza VL, Cellular fibroma of the ovary with multiloculated macroscopic characteristicsCase Reports in Medicine 2012 2012:283948 [Google Scholar]
[6]. Leung SW, Yuen PM, Ovarian fibroma: a review on the clinical characteristics, diagnostic difficulties, and management options of 23 casesGynecol Obstet Invest 2006 62(1):1-6. [Google Scholar]
[7]. Tarcoveanu E, Dimofte G, Niculescu D, Vasilescu A, Moldovanu R, Ferariu D, Ovarian fibroma in the era of laparoscopic surgery: a general surgeon’s experienceActa Chir Belg 2007 107(6):664-69. [Google Scholar]
[8]. Cho YJ, Lee HS, Kim JM, Joo KY, Kim ML, Clinical characteristics and surgical management options for ovarian fibroma/fibrothecoma: a study of 97 casesGynecol Obstet Invest 2013 76(3):182-87. [Google Scholar]
[9]. Choo YC, Mak KC, Hsuo A, Wong TS, Ma HK, Postmenopausal uterine bleeding of non organic causeObstet Gynecol 1985 66:225-28. [Google Scholar]
[10]. Parwate NS, Patel SM, Arora R, Gupta M, Ovarian fibroma: A clinico-pathological study of 23 cases with review of literatureThe Journal of Obstetrics and Gynaecology of India 2016 66(6):460-65. [Google Scholar]
[11]. Haroon S, Zia A, Idrees R, Memon A, Fatima S, Kayani N, Clinicopathological spectrum of ovarian sex cord-stromal tumours;20 years’retrospective study in a developing countryJournal of Ovarian Research 2013 6:87 [Google Scholar]
[12]. Sekiguchi I, Suzuki M, Tamada T, Estrogen producing activity in epithelial ovarian tumours and dermoid cystsAsia Oceania J Obstet Gynaecol 1989 15(4):367-74. [Google Scholar]
[13]. Numanoglu C, Kuru O, Sakinci M, Akbayır O, Ulker V, Ovarian fibroma/fibrothecoma: retrospective cohort study shows limited value of risk of malignancy index scoreAust NZ J Obstet Gynaecol 2013 53(3):287-92. [Google Scholar]
[14]. Mak CW, Tzeng WS, Chen CY, Computed tomography appearance of ovarian fibrothecomas with and without torsionActa Radiol 2009 50(5):570-75. [Google Scholar]
[15]. Yen P, Khong K, Lamba R, Corwin MT, Gersovich EO, Ovarian fibromas and fibrothecomas: sonographic correlation with computed tomography and magnetic resonance imaging: A 5-year single-institution experienceJ Ultrasound Med 2013 32(1):13-18. [Google Scholar]