Large Eccrine Acrospiroma of the Hand
Surya Rao Rao Venkata Mahipathy1, Alagar Raja Durairaj2, Narayanamurthy Sundaramurthy3, Vimal Chander Rajamanohar4, Prabu Shankar Sivagnanam5
1 Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Kanchipuram, Tamil Nadu, India.
2 Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Kanchipuram, Tamil Nadu, India.
3 Assistant Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Kanchipuram, Tamil Nadu, India.
4 Associate Professor, Department of Pathology, Saveetha Medical College and Hospital, Kanchipuram, Tamil Nadu, India.
5 Associate Professor, Department of General Surgery, Saveetha Medical College and Hospital, Kanchipuram, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Rao Rao Venkata Mahipathy, Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Kanchipuram 602105, Tamil Nadu, India.
E-mail: surya_3@hotmail.com
Eccrine acrospiroma are benign skin tumours of sweat duct origin. They usually present as small solid or cystic lesions which are confused clinically with other solid or cystic lesions. These are generally benign lesions with few reports of malignant transformation. Here, we report a case of a middle aged female presenting with a swelling of the dorsum of left first web space which was histopathologically diagnosed as an eccrine acrospiroma, which was managed with surgical excision and covered with a regional flap. This case is presented due to the large size of the lesion in the hand.
Benign, Malignant transformation, Surgical excision, Sweat duct
Case Report
A 45-year-old female presented to the Department of Plastic Surgery with a swelling on the dorsum of left hand for period of about two years. Patient was apparently normal till two years ago when she noticed a small painless swelling on the dorsum of left hand near base of thumb. On examination, a 4 x 4 x 2.5 cm firm non tender swelling was present on the dorsal aspect of base of left thumb. Margins were well defined and the surface was lobular. Skin over the swelling was normal. Thumb extensors were normal. [Table/Fig-1].
Pre-op clinical photograph showing the swelling.

A clinical diagnosis of dermatofibrosarcoma protuberans was made. MRI of the left hand showed T1, T2 heterointense lobulated mass lesion measuring 3.3 x 2.7 x 2.8 cm in the dorsal subcutaneous plane of the left proximal thumb with areas of T1 hyperintensity and foci of T2 hypointensity seen within the lesion. Cystic foci and multiple thick enhancing septations were seen within the lesion. Post contrast images showed intense arterial enhancement of the lesion with arterial feeders seen arising from the princeps polliceps artery, a branch of the radial artery and the cephalic vein encircling the lesion. The lesion was seen overlying the first metacarpal, proximal interphalangeal joint and base of proximal phalanx. Adjacent metacarpal and proximal phalanx bone showed normal signal intensity with intact cortex and no evidence of invasion. The lesion appeared superficial to extensor pollicis longus and extensor pollicis brevis tendons with no obvious infiltration or invasion of the tendons. A probable diagnosis of a giant cell tumour of the tendon sheath was given by the radiologist [Table/Fig-2].
MRI pictures showing areas of T1 hyperintensity and foci of T2 hyperintensity with cystic foci and thick septations. Bones and tendons are normal.

Surgical excision of the lesion was planned. Under supraclavicular block and tourniquet control, the lesion was excised in toto with a 1cm margin. Extensor tendons and neurovascular structures were preserved. The defect was 5 x 5 cm [Table/Fig-3].
Defect after surgical excision.

A posterior interosseous artery flap was planned in reverse and executed [Table/Fig-4]. The flap was tunnelled into the defect and inset given with 3-0 nylon and the secondary defect covered with a split skin graft [Table/Fig-5].
Posterior Interosseous artery Flap marking.

Flap tunneled into defect and secondary defect covered with split skin graft.

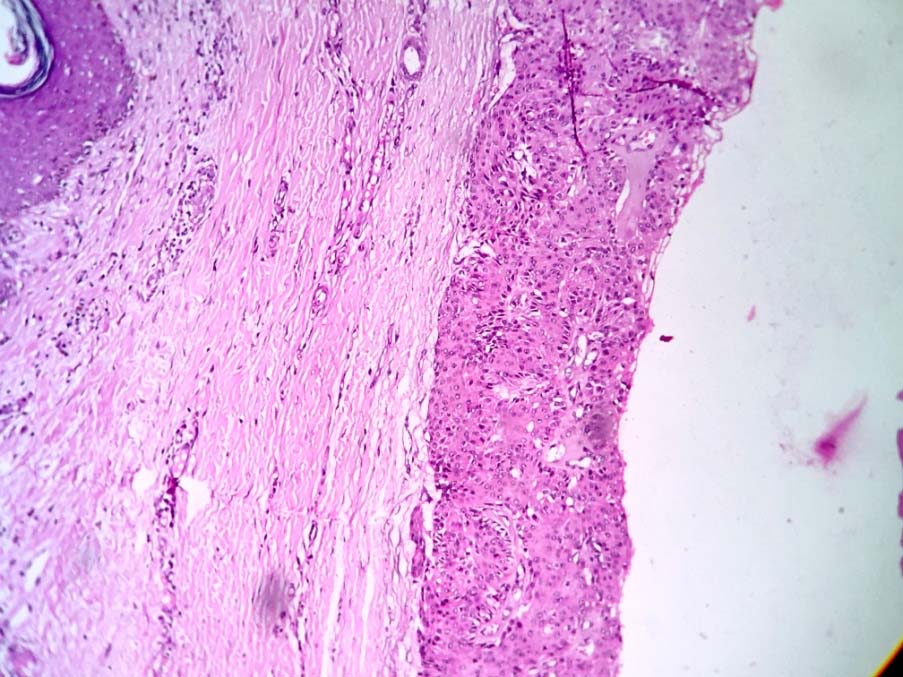
The flap and the split skin graft were well settled on the 5th postoperative day. Microscopic examination revealed stratified squamous epithelium of skin with underlying dermis [Table/Fig-6].
Stratified squamous epithelium of skin with underlying dermis showing the benign neoplasm (H&E 10X).
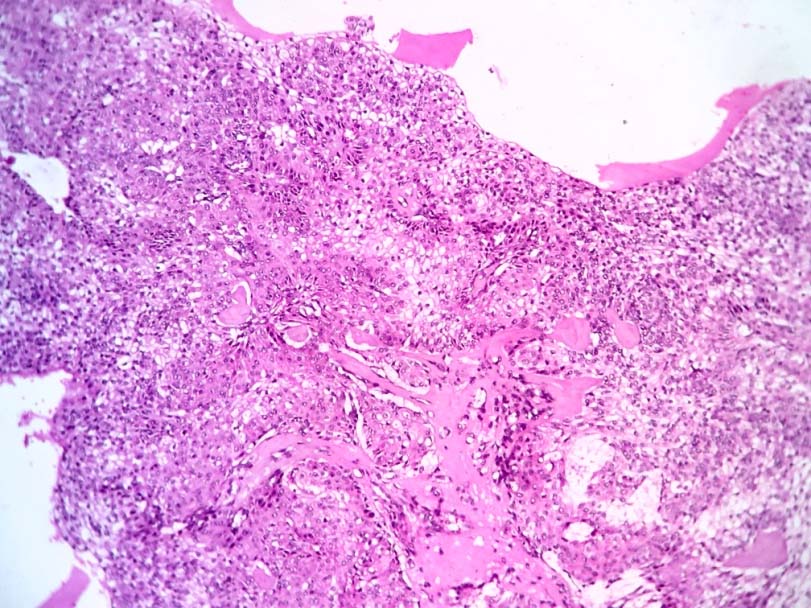
[Table/Fig-7] showing a benign neoplasm composed of cells arranged in lobules and sheets with interspersed capillaries and cystic spaces (H&E 10X). The cells were polygonal with abundant clear to pale eosinophilic cytoplasm and regular small round nuclei [Table/Fig-8].
Benign neoplasm composed of cells arranged in lobules and sheets with interspersed capillaries and cystic spaces (H&E 10X).
The tumor cells are polygonal with clear to pale eosinophilic cytoplasm and uniform round nuclei (H&E 40X).
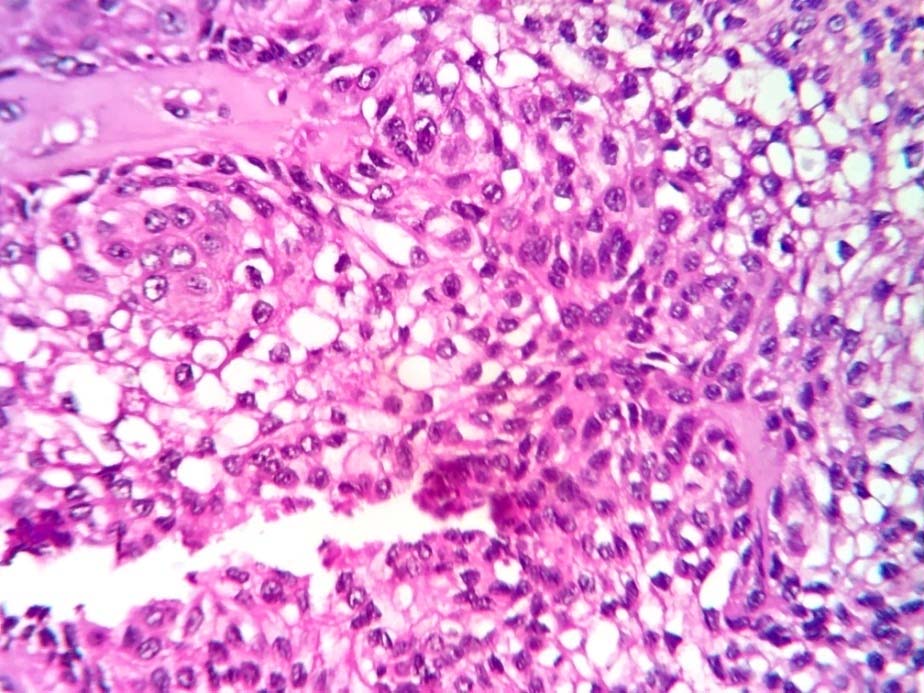
There was no atypia or necrosis, features suggestive of nodular hidradenoma (eccrine acrospiroma). Patient was discharged and reviewed at weekly intervals. The flap was well settled when patient came for review after two months [Table/Fig-9].
Two months follow up picture.

Discussion
Eccrine acrospiroma, is a benign cutaneous tumour arising from the epithelial cells of eccrine sweat ducts as defined by Johnson BL Jr and Helwig EB in 1969 [1]. Acrospiromas are usually less than 2 cm in size solid or cystic lesions presenting as solitary plaques, nodules or exophytic papules. It generally presents in all age groups throughout the body and are usually benign [2]. These tumours are known for malignant transformation [2]. Eccrine acrospiroma are also termed as clear cell, nodular, superficial or solid-cystic hidradenoma; clear cell papillary carcinoma; clear cell myoepithelioma; porosyringoma; large cell sweat gland adenoma; or basal cell carcinoma of sweat gland origin [3]. Clinically they masquerade as some other nodular and cystic lesions. The characteristic feature is that the skin over the tumour is smooth and either flesh-coloured, red or blue but at times it can be thickened and papillary. These tumours usually occur in adults and in some children [4]. Histologically, the tumours are further classified as epidermal when the lesion is confined to the epidermis and dermal acrospiroma when the tumour is found in the dermis [5]. Large eccrine acrospiromas may foster concerns of malignancy, but malignant eccrine acrospiromas are rare usually of moderate size. In a review of the literature, the largest dimension specified for malignant acrospiromas ranged from 4 to 10 cm [2]. In one study, four tumours (out of 38 total tumours) with diameters of more than 4 cm are accepted as tumours of ‘large size’. Acrospiromas occur on all areas of the body, but with preponderance on the trunk (40%), the head (30%) and extremities (30%) [6,7]. Acrospiromas commonly affect middle-aged and older women by a ratio of approximately 2:1. They are occasionally associated with tenderness and pruritis (7%) [3].
The differential diagnosis includes haemangioma, squamous cell carcinoma, melanoma, metastatic tumours and other adnexal tumours [2]. Eccrine acrospiromas stain positive for keratin, Epithelial Membrane Antigen (EMA), Carcinoembryonic Antigen (CEA), S-100 and vimentin whereas glomus tumours stain positive for CD 34. Malignant acrospiromas are aggressive lesions with increased tendency for lymphatic and distant metastasis [8]. They present as solid lesions with minimal cystic areas. The diagnosis is difficult both clinically and histopathologically [8]. Microscopy of malignant eccrine acrospiroma shows cellular atypia, increased mitoses, local areas of infiltration and necrosis, perineural and angiolymphatic invasion [3]. Malignant transformation of benign eccrine acrospiromas has also been reported [3]. The mainstay treatment for benign acrospiromas is surgical excision. Inadequate excision seems to be the cause of recurrence [1]. Malignant acrospiromas require wide local excision with regional lymph node dissection even when there is a clinically negative lymph node examination. The prognosis of benign acrospiroma is good and the recurrence rate after adequate excision is nil [9].
Conclusion
Eccrine acrospiromas are solitary benign cutaneous lesions of sweat duct origin. They are often confused with other clinical conditions. Careful examination of the lesion microscopically will lead to the diagnosis. Surgery is the only treatment and the patient should be on regular follow up as malignant transformation has been known to occur.
[1]. Johnson BL, JrHelwig EB, Eccrine acrospiroma: A clinicopathologic studyCancer 1969 23:641-57. [Google Scholar]
[2]. Hunt SJ, Santa Cruz DJ, Kerl H, Giant eccrine acrospiromaJ Am Acad Dermatol 1990 23:663-68. [Google Scholar]
[3]. Laws RA, English JC, 3rdElston DM, Acrospiroma: A case report and reviewCutis 1996 58:349-51. [Google Scholar]
[4]. Bagga P, Shahi M, Mahajan N, Clear Cell Hidradenoma- a case reportThe Internet Journal of Pathology 2008 8:2 [Google Scholar]
[5]. Fletcher CD, Diagnostic histopathology of tumours 2000 3rd EdPhiladelphiaChurchill Livingstone:1457-458. [Google Scholar]
[6]. Cohen PR, Tschen JA, A painless enlarging scalp nodule: Eccrine acrospiomaArch Dermatol 1992 128:547-50. [Google Scholar]
[7]. Grossniklaus HE, Knight SH, Eccrine acrospiroma (clear cell hidradenoma) of the eyelid: Immunohistochemical and ultrastructural featuresOphthalmology 1991 98:347-52. [Google Scholar]
[8]. Long WP, Dupin C, Levine EA, Recurrent malignant acrospiroma: treatment by chest wall excisionDermatol Surg 1998 24:908-12. [Google Scholar]
[9]. Koçer U, Aksoy HM, Tiftikcioðlu YO, Ertoy D, Karaaslan O, Giant eccrine acrospiroma: A case report and review of the literatureCan J Plast Surg 2003 11(1):43-46. [Google Scholar]