Large renal tumours are not uncommon in developing countries. Enhancing renal tumours are considered to be malignant unless proved otherwise and radical surgical resection remains the mainstay of treatment of such tumours. A giant renal tumour, especially on right side, poses a big challenge for the operating team and requires a thoracoabdominal approach for successful excision. We report successful removal of the largest documented Multilocular Cystic Nephroma (MLCN, 5.5 kg) from a 28-year-old female who presented with right abdomen lump since two years. The surgery was done through a 9th intercostal thoracoabdominal incision as the mass (31 x 19 x 19.6 cm) extended from right sub-diaphragmatic space up to the dome of the bladder. We discuss here the technique of removing such a huge renal mass and the challenges an operating surgeon may encounter.
Case Report
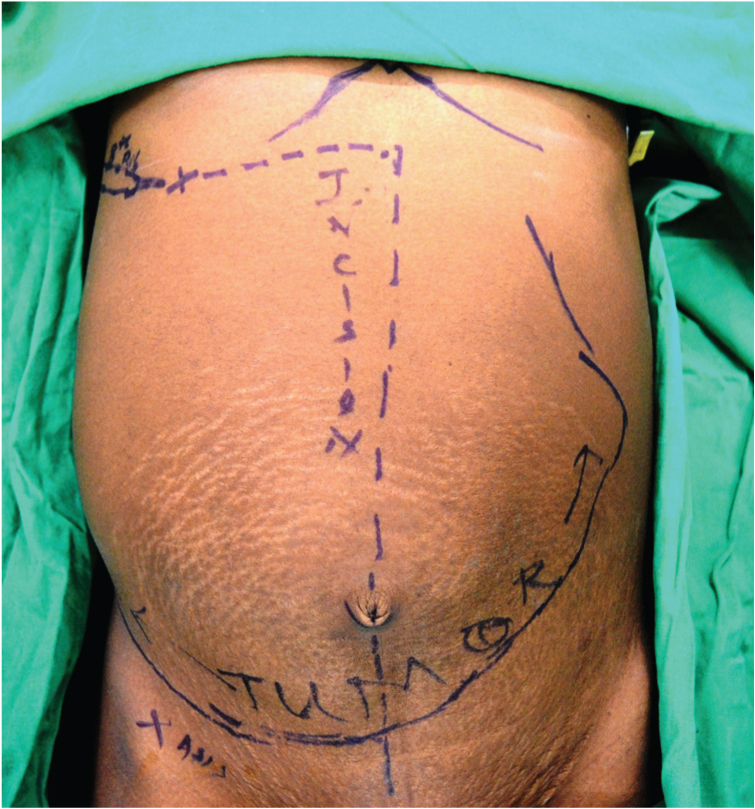
A 28-year-old female, hailing from rural part of India, presented with a progressively increasing right abdomen lump with flank pain and haematuria for two years. On examination, the patient was of average built with a large visible right intra-abdominal mass extending from right subcostal region to the hypogastric region and crossing the midline and was firm, smooth, non-tender [Table/Fig-1].
Visible right renal tumour and the right thoracoabdominal incision.
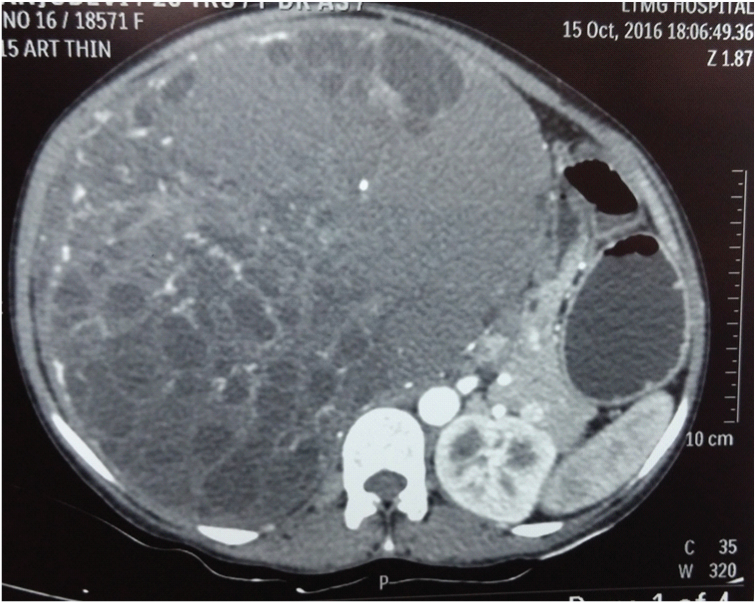
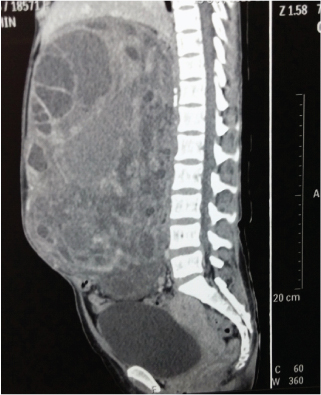
On investigations, Hb was 12 gm% with normal renal and liver function tests. Radiological investigations showed a large multicystic right renal tumour extending from infrahepatic to hypogastric region on ultrasonography. Contrast enhanced CT scan showed a multicystic enhancing tumour of 31 x 19 x 19.6 cm size arising from right kidney. Thin strip of normal renal parenchyma was evident inferolateral to the tumour. The tumour was extending from sub hepatic region to the dome of bladder and from anterior to posterior abdominal wall sagitally. The tumour was crossing the midline and was pushing the duodenum, head of pancreas and IVC to the left [Table/Fig-2,3 and 4]. Right Renal vein was free of thrombus and Chest X ray was normal. The preoperative differential diagnosis was a multicystic Renal Cell Carcinoma (RCC, T2bN0M0) or a MLCN.
Transverse section of CECT showed 31x19x19.6 cm right renal mass, which pushed IVC, duodenum and head of pancreas to the left.
Sagittal section showed the multiloculated cystic tumour extending from subhepatic region up to the dome of the bladder and from anterior to posterior wall.
Right thoracoabdominal incision with right eighth rib exposed and tumour visible.
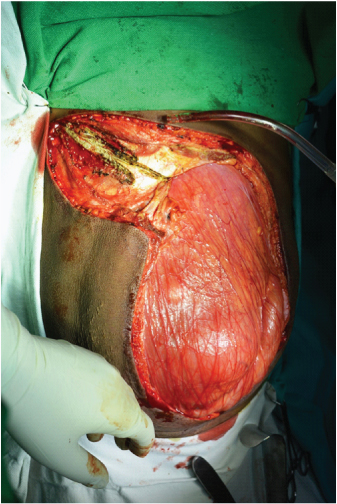
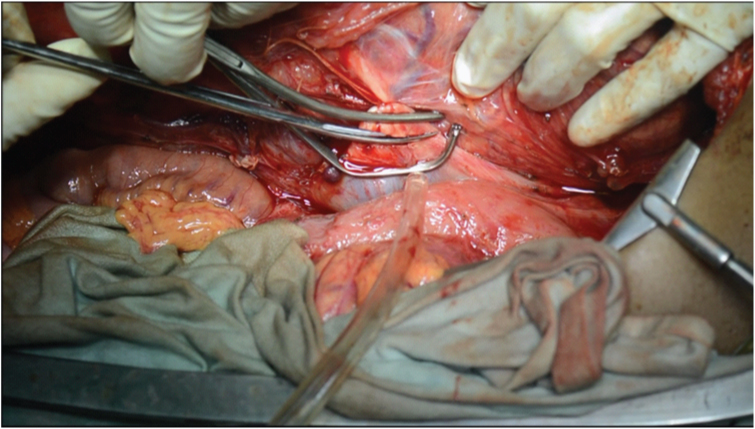
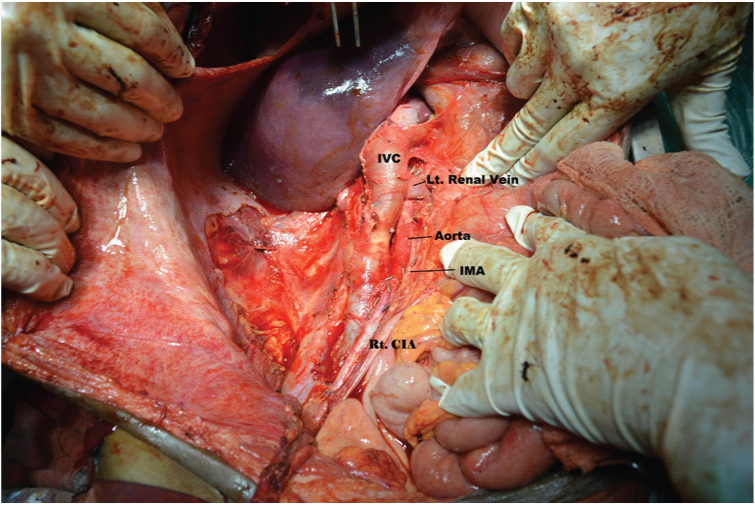
She underwent right radical nephrectomy by an eighth rib cutting thoracoabdominal incision [Table/Fig-5]. The tumour was occupying the entire right abdomen and was pushing the intestines, IVC (inferior vena cava) and head of the pancreas to the left. The colon was mobilised, duodenum kocherized and dissection was carried out on medial aspect of tumour to expose the renal vessels. Bookwalter retractor helped significantly in reducing the number of hands occupied for retraction. Right renal artery was dissected, ligated and cut between the ligatures [Table/Fig-6]. Right renal vein was dissected which was enlarged (3.5 to 4 cm in diameter) with no evidence of tumour thrombus. Satinsky clamp was applied on IVC [Table/Fig-7] and the Renal vein was incised at its origin and the defect in IVC was closed with polypropylene 4/0 vascular continuous sutures in two layers [Table/Fig-8]. After the control of vascular pedicles the mass was then dissected inferolaterally and right ureter with gonadal vein were ligated. It was then dissected posteriorly and cranially from liver and diaphragm. Right adrenal vein was ligated and the tumour was finally delivered out. Radical lymph node dissection was done from crus of diaphragm to bifurcation of aorta for removal of paracaval and interaortocaval lymph nodes [Table/Fig-9,10].
Right renal artery dissected.
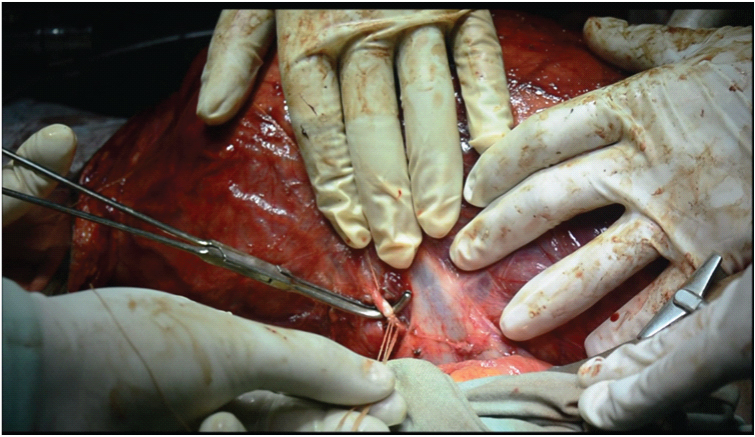
Right renal vein was enlarged (3.5-4 cm diameter). Satinsky clamp applied over IVC and renal vein being cut.
Final appearance of the dissection after right radical nephrectomy and lymphadenectomy fromcrus of diaphragm to bifurcation of aorta.
Right thoracoabdominal wound closed in two layers and skin closed with staples.

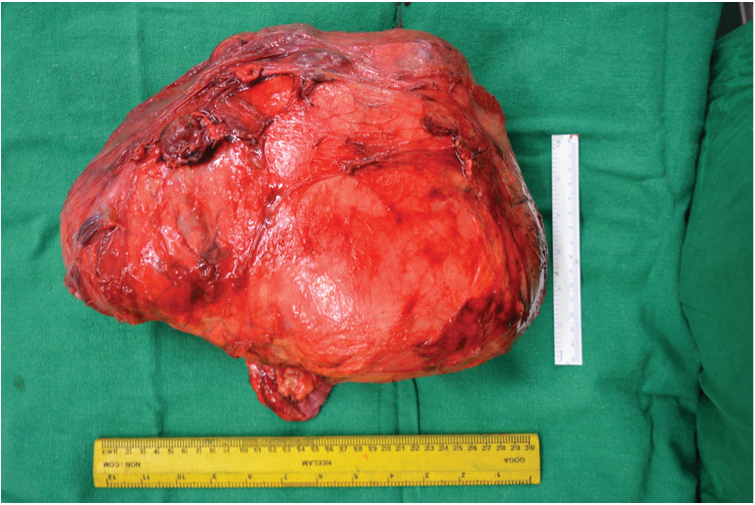
Weight of the renal tumour - 5.5 kg.

The specimen - 31x19x 9.6 cm.
After ensuring haemostasis, Intercostal (ICD) and abdominal drains were kept. The diaphragm was closed with polypropylene 2/0 interrupted sutures. The edges of costal cartilage were approximated with polyamide 1/0 sutures. The thoracoabdominal incision was closed in two layers [Table/Fig-11]. Patient required mechanical ventilation for 24 hours postoperatively. Postoperative pain control for the first two days was achieved with epidural analgesia. Her recuperation was uneventful. Abdominal drain was removed on Post op day four when output was less than 20 ml per day. Intercostal drainage tube was removed on day seven.
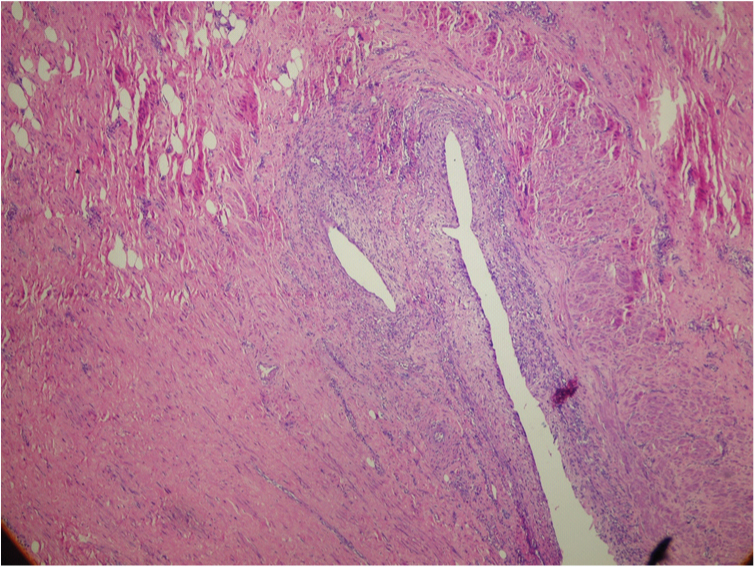
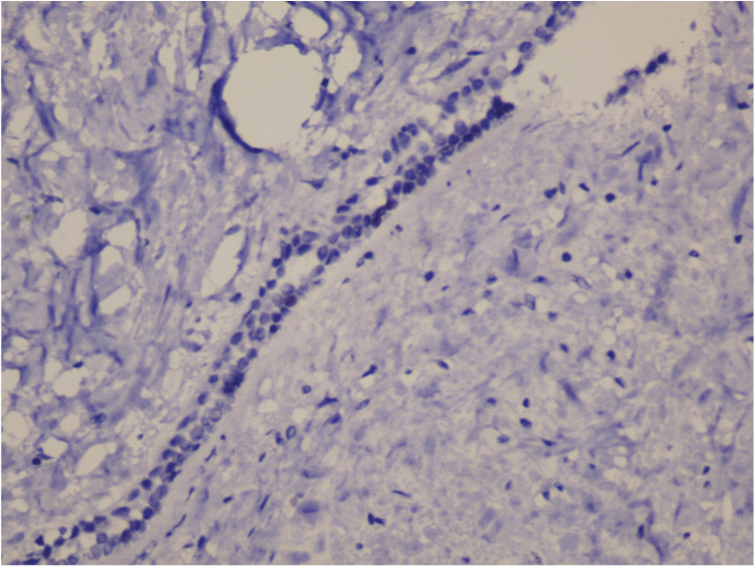
Haematoxylin and eosin stain the excised mass was composed of multiple cysts lined by cuboidal cells and scattered ‘hobnail’ cells as seen in MLCN. The stroma was composed of spindle cells and pauci-cellular collagen resembling ovarian stroma. Entrapped mature adipose tissue was seen too. No blastemal or glomerular component was seen. (4X).
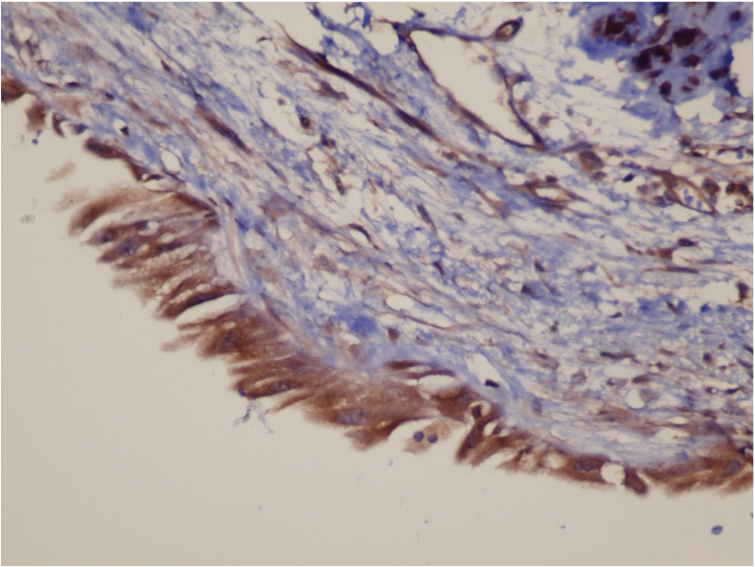
The mass weighed 5.50 kg [Table/Fig-12,13]. On histopathological examination and Immunohistochemistry (positive for oestrogen and progesterone receptors, SMA, WT1 and CK; negative for HMB-45 and S-100), the mass was a MLCN and the lymph nodes were found to be reactive [Table/Fig-14,15 and 16].
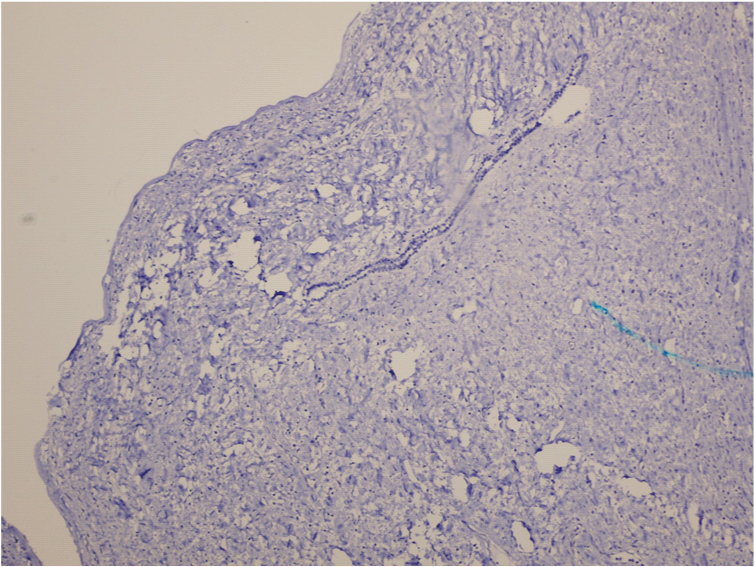
HMB 45 ImmunoHistochemistry (IHC) Negative (4X).
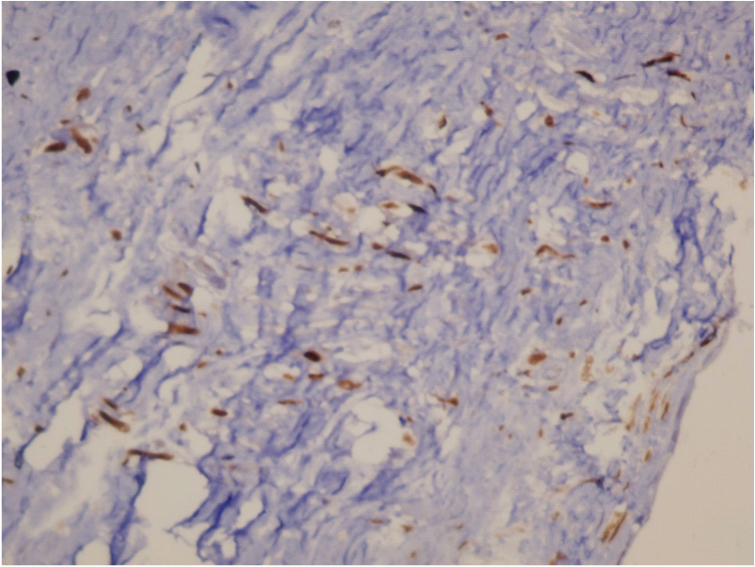
Progesterone receptor IHC Positive (10X). [
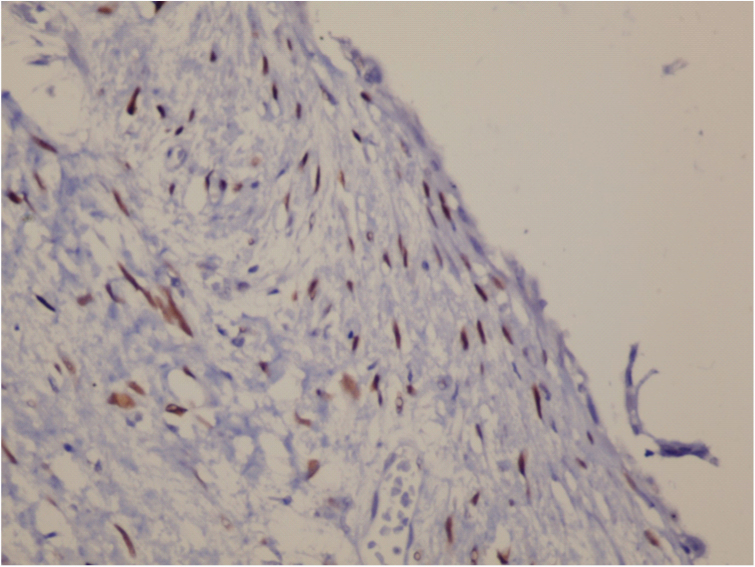
Estrogen Receptor IHC Positive (10X).
S 100 IHC Negative (10x).
Discussion
Large kidneys or renal masses are encountered in several pathological conditions like polycystic kidney disease, complex and simple cysts, RCC or even benign neoplasia like Angiomyolipoma (AML), MLCN [1,2].
A primary renal mass is malignant in 80% cases and benign in 20% cases [2]. Besides, it is radiologically impossible to differentiate a malignant renal mass from a benign one, with an exception of AML. For this reason, any solid renal mass is considered malignant and managed accordingly unless proven otherwise. Principles of radical nephrectomy include early control of renal vessels, excision of mass along with intact Gerota’s fascia, lymph node dissection in selected patients and adrenal gland preservation [2].
Early vascular control of a small renal tumour is possible through Flank 11th or 12th rib-cutting incision. However, for large renal tumours overlapping or pushing the hilum towards opposite side, conventional flank approach often prove to be inadequate for early vascular control. Dissecting such a large tumour free from liver and diaphragm (upper pole) is also difficult through a flank/midline approach and may require assistance of hepatic surgeon. In such cases, a thoracoabdominal incision gives the best exposure, especially on the right side and in venous involvement [2-5]. However, Thoracoabdominal incision causes higher postoperative pain and complications like haemopneumo thorax. For this reason, it is reserved for extremely large renal masses extending up to the diaphragm (as in our case – 31 x 19 x 19.6 cm in size) [2-5].
Large renal tumours are a challenge because of the increased vascularity, retroperitoneal position, proximity to large vessels and surrounding vital organs and therefore require a multidisciplinary team approach involving Urologists, Hepatic and Vascular surgeons, Uroanaesthetists, Intensivists, Interventional Radiologists. They are preferably operated in Tertiary Care Centres, where all the infrastructure and experience is available under one roof. Preoperative work up includes cardiac and chest fitness, extensive metastatic workup.
The indexed patient had a huge right renal mass (31 x 19 x 19.6 cm in size), extending from subhepatic region right up to dome of bladder. To remove such tumours, especially from upper pole, thoracoabdominal transpleural and transperitoneal approach is required and early vascular control helps in resection with minimal blood loss. These tumours need to be dissected meticulously from surrounding vital structures like IVC, duodenum, pancreas, colon and liver.
Histopathological examination revealed that the tumour was a MLCN which is a relatively rare benign tumour with only 200 cases reported over last 150 years [6,7].
MLCN is a benign renal mass with a bimodal age distribution. It has two peaks, first at one or two years of life (predominantly in boys) and second in fourth and fifth decades of life (predominantly in females, 8:1 preponderance) [1,8-10] Our patient was a 28-year-old female. Clinically, patients present with palpable mass, abdominal pain, haematuria just as in RCC. Radiologically, MLCN usually present as a solitary, centrally located cystic lesion of mean 9 cm size [1,11].
In the present case, the tumour, which was 31 cm in its maximal length, is the largest MLCN documented till date. These masses, if left untreated, progressively increase in size to achieve giant proportions and gradually push the surrounding viscera and great vessels to the opposite side [Table/Fig-2]. A cystic mass with septal enhancement is difficult to differentiate on CT scan from a cystic RCC and the diagnosis is histopathological, after surgical removal [12]. We did radical nephrectomy with lymph node dissection owing to enlarged lymph nodes found intraoperatively.
The tumour weighed 5.5 kg and had maximum diameter of 31 cm. To the best of our knowledge and after extensive database search (PubMed, Google Scholar), it is the largest (31 cm) and the heaviest (5.5 kg) MLCN removed successfully and published till date [Table/Fig-17] [7,10,11,13-19].
Case studies and review of literature on MLCN.
| Study | Year | Number of cases | Largest mass |
|---|
| Present case | 2016 | 1 | 31 x 19 x 19.6 cm (5.5 kg) |
| Wilkinson C et al., [7] | 2013 | 6 | 12 cm |
| Stamatiou K et al., [10] | 2008 | Case report and review of literature | 7 cm (371 gm) |
| Turbiner J et al., [11] | 2007 | 34 | 14 cm |
| Granja M et al., [13] | 2015 | Review of literature (179 cases reviewed) | 24 cm |
| Mukhopadhyay S et al., [14] | 2004 | 10 | 13 cm |
| Montironi R et al., [15] | 2008 | - | - |
| Baldauf MC et al., [16] | 1976 | 3 | 12 x 8 cm (285 gm) |
| Carlson DH et al., [17] | 1978 | 3 | 15 x 12 x 8 cm |
| Banner MP et al., [18] | 1981 | 13 | 23 cm |
| Joshi W et al., [19] | 1989 | 5 | 24 cm |
Histopathologically, the excised mass was composed of multiple cysts lined by cuboidal cells and scattered ‘hobnail’ cells as seen in MLCN. The stroma was composed of spindle cells and paucicellular collagen resembling ovarian stroma [1,20]. Entrapped mature adipose tissue was seen too [Table/Fig-11]. No blastemal or glomerular component was seen. Immunohistochemistry of MLCN has not been studied in detail compared to other renal tumours considering the rarity of the tumour [14]. The specimen in the present case was positive for oestrogen and progesterone receptors, SMA, WT1 and CK; negative for HMB-45 and S-100, supporting MLCN [Table/Fig-12,13,14,15 and 16] [14,15].
Conclusion
Giant renal masses are not a rare presentation, especially in a country where there is a huge rural population and the Urologist is often required to rise to the challenge. Thoracoabdominal incision is the preferred approach for such a large renal tumour. Such patients are better treated in a Tertiary Care Hospital with a multidisciplinary team approach.
[1]. Margulis V, Karam J, Matin S, Wood C, Benign renal tumoursUrology, Campbell-Walsh. Alan Wein, Louis Kavoussi, Alan Partin, Craig Peters 2016 Elsevier:1309 [Google Scholar]
[2]. Campbell S, Lane B, Malignant renal tumoursWein, Kavoussi, Peters, Partin. Campbell Walsh Urology 2016 Elsevier:1315 [Google Scholar]
[3]. Blute M, Inman B, Smith H. S, Hinman JA, Simple nephrectomyAtlas of Urologic Surgery 2012 Saunders:985 [Google Scholar]
[4]. Sawh LR, Budhooram S, Ewe P, Rattan R, Sawh SL, A case report of one of the largest {3.63 kg}renal tumour removed in the western hemisphere. A combined Uro vascular approach for complete removalInternational Journal of Surgery Case Reports 2016 24:156-61. [Google Scholar]
[5]. Moslemi MK, Hosseini SJE, Firoozabadi MHD, A huge renal cell carcinoma, nine years after its primary diagnosis and obligate observationCase Reports in Oncology 2010 3(3):326-33. [Google Scholar]
[6]. Edmunds W, Cystic adenoma of the kidneyTrans Pathol Soc Lond 1892 43:89-90. [Google Scholar]
[7]. Wilkinson C, Palit V, Bardapure M, Thomas J, Browning AJ, Gill K, Adult multilocular cystic nephroma: Report of six cases with clinical, radiopathologic correlation and review of literatureUrol Ann 2013 5(1):13-17. [Google Scholar]
[8]. Madewell JE, Goldman SM, Davis CJ, JrHartman DS, Feigin DS, Lichtenstein JE, Multilocular cystic nephroma: A radiographic-pathologic correlation of 58 patientsRadiology 1983 146:309-21. [Google Scholar]
[9]. Upadhyay AK, Neely JA, Cystic nephroma: An emerging entityAnn R Coll Surg Engl 1989 71(6):381-83. [Google Scholar]
[10]. Stamatiou K, Polizois K, Kollaitis G, Dahanis S, Zafeiropoulos Leventis C, Cystic nephroma: A case report and review of the literatureCases Journal 2008 1:267 [Google Scholar]
[11]. Turbiner J, Amin MB, Humphrey PA, Srigley JR, De Leval L, Radhakrishnan A, Cystic nephroma and mixed epithelial and stromal tumour of kidney: A detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumour (REST) as a unifying termAm J Surg Pathol 2007 31(4):489-500. [Google Scholar]
[12]. Vujanic GM, Jenney ME, Adams H, Meyrick SM, Juxtaposed cystic nephroma and Wilms’tumourPediatr Dev Pathol 2000 3:91-94. [Google Scholar]
[13]. Granja M, O’Brien A, Trujillo S, Mancera J, Aguirre D, Multilocular cystic nephroma: A systematic literature review of the radiologic and clinical findingsRoentgenology 2015 205:1188-93. [Google Scholar]
[14]. Mukhopadhyay S, Valente AL, de la Roza G, Cystic nephroma: A histologic and immunohistochemical study of 10 casesArch Pathol Lab Med 2004 128(12):1404-11. [Google Scholar]
[15]. Montironi R, Mazzucchelli R, Lopez-Beltran A, Martignoni G, Cheng L, Montorsi F, Cystic nephroma and mixed epithelial and stromal tumour of the kidney: Opposite ends of the spectrum of the same entity?Eur Urol 2008 54(6):1237-46. [Google Scholar]
[16]. Baldauf MC, Schulz DM, Multilocular cyst of the kidney. Report of three cases with review of the literatureAm J Clin Pathol 1976 65(1):93-102. [Google Scholar]
[17]. Carlson DH, Carlson D, Simon H, Benign multilocal cystic nephromaAm J Roentgenol 1978 131(4):621-25. [Google Scholar]
[18]. Banner MP, Pollack HM, Chatten J, Witzleben C, Multilocular renal cysts: Radiologic-pathologic correlationAJR Am J Roentgenol 1981 136(2):239-47. [Google Scholar]
[19]. Joshi VV, Beckwith JB, Multilocular cyst of the kidney (cystic nephroma) and cystic, partially differentiated nephroblastoma. Terminology and criteria for diagnosisCancer 1989 64:466-79. [Google Scholar]
[20]. Tamboli P, Ro JY, Amin MB, Ligato S, Ayala AG, Benign tumours and tumour-like lesions of the adult kidney part II: Benign mesenchymal and mixed neoplasms, and tumour-like lesionsAdv Anat Pathol 2000 7(1):47-66. [Google Scholar]