Role of Multi-Detector CT (MDCT) in Evaluation of Bowel Diseases
Mohamad Tufail Sheikh1, Mohd Tafazul Sheikh2, Masrat Jan3, Hayat A Khan4, Guru P. Vashisht5, Mohd L Wani6
1 Senior Specialist, Department of Radiology, Dr. Sulaiman Al Habib Hospital, Sweidi Riyadh.
2 M Ch Scholar, Department of Plastic Surgery, JLN Medical College, Aligarh, Uttar Pradesh, India.
3 Senior Resident, Department of Gynaecology and Obstetrics, Sher-i-Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India.
4 Senior Resident, Department of Orthopaedics, Sher-i-Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India.
5 Director and Head, Department of Imaging, Batra Hospital and Medical Research Centre, New Delhi, India.
6 Senior Resident, Department of CTVS, Sher-i-Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohamad Tufail Sheikh, Senior Specialist, Department of Radiology, Dr. Sulaiman Al Habib Hospital, Sweidi-12987, Riyadh Saudi Arabia.
E-mail: sheikhtufail@gmail.com
Introduction
Multi-Detector Computed Tomography (MDCT) has revealed excellent results in various systems of the body. Its role in abdominal imaging for solid viscera has been proved beyond doubt. It is an emerging non invasive tool for evaluation of bowel diseases.
Aim
To see the efficacy of MDCT in evaluation of various bowel diseases.
Materials and Methods
The study was carried out in the Department of Radiodiagnosis and Imaging, Batra Hospital and Medical Research Centre, Delhi, India. A total of 60 patients were enrolled in this study from March 2008 to June 2010 over a period of 24 months. All patients suspected to have inflammatory, obstructive, ischaemic and neoplastic diseases of small or large bowel disease were included in the study. The patients with past history of chronic renal failure, allergic reaction to contrast were excluded from the study. Comparison was made between CT findings with the operative findings, endoscopy, angiography or histopathology correlation whichever was relevant with case. All this data was compiled and statistically analysed.
Results
Out of 60 patients 12 patients were diagnosed having appendicitis using axial, Multiplaner Reconstruction (MPR) and curved MPR images. The findings of appendicitis were confirmed on surgery and subsequent histopathology correlation. Inflammatory bowel diseases comprised of 28 cases out of which seven persons were diagnosed with intestinal Koch’s disease. Four patients had idiopathic inflammatory bowel diseases. Rest of the 17 patients were reported to have findings of non-specific colitis and they responded well with antibiotic treatment.
Conclusion
The sensitivity and specificity of MDCT in case of bowel obstruction clearly demonstrates not only the site of obstruction, but also reveal the cause of obstruction which includes intraluminal, intramural and extrinsic factors. CT scan categorizes the lesion to inflammatory or neoplastic to a greater accuracy. MDCT can also demonstrate the complications associated with obstruction like strangulation and perforation. CT is now considered a good tool in the evaluation of patients with suspected bowel obstruction, particularly in indeterminate clinical and conventional radiographic findings.
Appendicitis, Bowel obstruction, Inflammatory bowel disease
Introduction
The introduction of CT in the 1970s heralded a new era in radiology, initially with applications to the head and later to the chest and abdomen. Abdominal studies were originally confined to the solid organs and the retro-peritoneum, extending eventually into the peritoneal cavity. Bowel detail itself was not referred to owing to slow data acquisition times and lack of definition [1]. There were many limitations of small-bowel follow-through and enteroclysis as these examinations provide only indirect information about the bowel wall and surrounding structures and also the problems due to by overlapping bowel loops [2]. To overcome the limitations of [3], previous techniques, CT enteroclysis, a technique combining the advantages of enteroclysis and CT, has been extensively investigated [4,5]. Although CT enteroclysis profits from excellent distention of the entire small bowel and precise evaluation of the extent of extra-luminal disease, it has the major drawbacks of invasiveness and high radiation exposure. Recently, the role of wireless capsule endoscopy to assess small-bowel disease has been reported. The value of this technique is well documented for diagnosing obscure gastrointestinal bleeding and early Crohn’s disease [6,7]. However, problems with this technique include capsule obstruction by bowel strictures and battery failure in prolonged transit (battery life is approximately 7 hours). The technique can overlook the results if there is rapid peristalsis at a lesion site or in case of bowel angulation may impair camera view [3,8].
Currently, the availability of MDCT and the continuous refinement of the 3D imaging process have greatly expanded the utility of CT for evaluating patients with bowel disease. MDCT is now readily available and has advantages over classic helical CT in the imaging of the mesenteric vasculature and of the bowel. The purpose of this study was to see MDCT in evaluation of small and large bowel diseases including tumours, appendicitis, diverticular, ischaemic bowel disease by utilizing the multiplanar capabilities (axial, coronal and sagittal images) and post processing techniques [like Maximum Intensity Projection (MIP), MPR, 3D Volume Rendering (VR)] for detailed evaluation of disease process and enhancing the diagnostic accuracy of initial diagnosis, management, follow up and detection of potential complications.
Materials and Methods
A prospective study was carried out in the Department of Radiodiagnosis and Imaging, Batra Hospital and Medical Research Centre, Tuglakabad Institutional Area, New Delhi. The study was carried out over a period of 24 months from March 2008 to June 2010 and total of 60 patients got enrolled during this period. Necessary clearance was taken from Ethical Committee and written informed consent was taken from every patient. All patients suspected to have inflammatory and obstructive small or large bowel disease were included in the study. The patients with past history of chronic renal failure and history of allergic reaction to contrast were excluded. All the cases were done on 64 slice MDCT of GE radical system with advanced workstation 4.2 GE for post processing. Scanning protocol include anatomical coverage 350–500 mm, scan direction cranio-caudal, acquisition time 5-6 sec. Factors used were mA 200-300 mA and kVp 120; rotation time 0.55 sec and pitch 1.014.
Patients were informed not to take any meals at least four hours prior to examination. Breath holding is an important requirement for the examination and patients were asked to practice the technique of breath holding for five minutes. About 500-1000 ml of low concentration Barium (0.1% w/v) mixed with sorbitol was given to patients at least one hour prior to study the small bowel loops and if large bowel loops is the area of interest, oral contrast has to be given four hours prior to the study. Scout films were taken to assess the opacification of bowel loops with contrast. Additional 50 ml of contrast was given to the patient orally just before the scan to opacify stomach and duodenum. Oral contrast was not given to patients suspected for bowel obstruction. Non-ionic contrast omnipaque 350 mg/ml was given intravenously through 18 G needle at the rate of 3 ml/sec. Scanning was performed on 64 slice MDCT beginning 45 seconds after contrast injection. Images were acquired of thickness 2.0-2.5 mm in a reconstruction interval of 1.0-1.5 mm. Automatic coronal reformatted images were generated on 64-slice MDCT using several parameters. For other scanners, coronal reformatted images were generated at the workstation from the axial images. CT abdomen was performed with a multi–detector row scanner (Light Speed VCT 64 slice Multi-detector CT, GE) with commercially available reconstruction software (4.2 workstation; GE Medical Systems). Helical scanning was performed within a single breath hold from liver to lower margin of pubic symphysis. The scan coverage is from lower thorax including both domes of diaphragm to the pubic symphysis in a cranial-to-caudal direction. Internal mammary arteries were also assessed. Bowel wall, mesenteric vasculature, mesentery can be studied post processing tools based on the advantage workstation environment. We used a workstation that permits real-time axial, multiplanar reconstruction, maximum-intensity-projection, and volume-rendering techniques. The axial images were considered to be the source images providing the basic information in the CT. Scrolling through these images in cranio-caudal direction allows interpretation of bowel lesions and other structures. However, because of complex course of intestines interpretation in multiplanar images is also required. In MPR, a plane is selected from the 3D volume and the region of interest is displayed in the desired plane. An MPR can be performed by using either straight planes or curved planes. More advanced methods of performing curved MPR allow localization of a lesion by selection of a point within the lumen of the bowel, after which automatic segmentation of the centerline of the intestine is used to perform the curved MPR. The limitation of MPR is that it is operator dependent. Therefore, MPR is prone to introduce false-positive or false-negative lesions. Furthermore, only one segment of a bowel can be displayed at a time. For each segment, a separate MPR image is required. All this data was compiled and statistically analysed. The findings on 64 slice MDCT were compared with either surgery or on colonoscopy or angiography.
Results
The study was more confined towards adults. Only five cases were less than 20 years of age and the youngest case of this study was 17-year-old. There were 27 females and rest 33 were males. Twelve patients were diagnosed having appendicitis using axial, MPR and curved MPR images. All of them were found having appendicitis on surgery [Table/Fig-1]. Twenty eight cases had inflammatory bowel disease out of which seven persons were diagnosed with intestinal Koch’s disease. For (non-neoplastic) inflammatory bowel diseases, following findings were considered: mild symmetrical wall thickening (<1.5 cm); segmental bowel wall thickening (>10 cm length of the involved bowel); homogeneous enhancement pattern with mural stratification and surrounding fat stranding, for neoplastic diseases marked asymmetrical wall thickening (>1.5-3.0 cm); focal bowel wall involvement (< 10 cm length of involvement); heterogeneous enhancement with associated enhancing lymph nodes or liver metastasis. Necrotic lymph nodes and/or loculated collections with peritonitis were considered for infective (e.g., Koch’s disease) aetiologies. Seven patients were put on ATT and were followed in six months. One case was lost in follow up and was excluded from the study. Out of the six remaining five patients, responded to ATT. One case did not respond to ATT, who then underwent colonoscopy. Colonoscopy revealed Crohn’s disease in it. Rest of the seventeen patients were reported to have findings of non-specific colitis and they responded well with antibiotic treatment. Four patients had idiopathic inflammatory bowel diseases. Three were reported as idiopathic inflammatory bowel disease (ulcerative colitis in two cases and Crohn’s disease in one). One patient was reported normal who subsequently underwent colonoscopy and was diagnosed with Crohn’s disease. Thus, one case was missed on CT. Three cases were reported as mesenteric ischemia (ischaemic colitis) and vascular occlusion. They subsequently underwent triple phase study which confirmed thrombus in Superior Mesenteric Artery (SMA) in first case [Table/Fig-2], thrombus in segmental branch of SMA in second case and thrombus in SMV in the third case [Table/Fig-3,4]. The overall sensitivity of MDCT for diagnosing inflammatory bowel is 96.3% and the specificity is 100%. Two cases were noted with secondary signs of perforation which include free fluid and free air in peritoneal cavity. There bowel findings revealed perforation in jejunum in one case and perforation in ileum in the other. The same was confirmed on surgery. In three cases, findings were suggestive of bowel malignancy. In one case growth was seen at recto-sigmoid junction and in two cases growth was seen at hepatic flexure of colon [Table/Fig-5]. They underwent colonoscopy and out of three cases, all the three cases revealed mitotic growth. This group included patients with findings which included hernias, diverticula and polyps. The same was confirmed on either surgery or on colonoscopy [Table/Fig-6]. The sensitivity, specificity, positive predictive value, negative predictive value and the kappa statistics for all the cases are given in [Table/Fig-7].
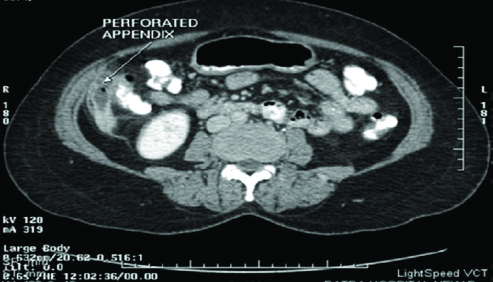
Dilated appendix showing wall enhancement and focal breech consistent with perforation.
Thrombus in SMA with distal bowel ischaemic changes.

Post processing MIP images showing thrombus in SMV.

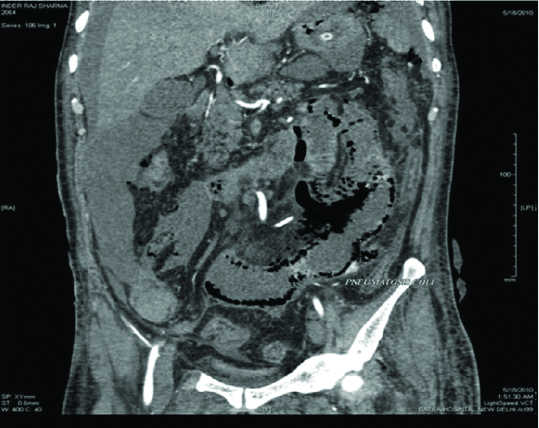
Transmural infarct and pneumatosis coli.
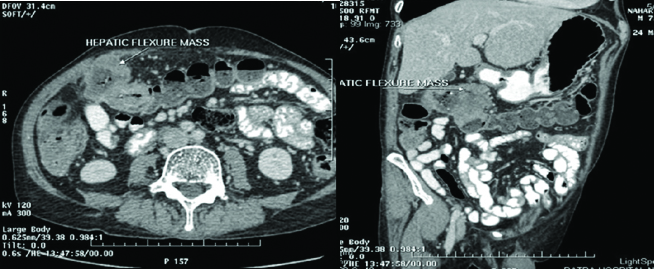
Axial images showing hepatic flexure mass. Post processing curved MPR showing the extent of mass.
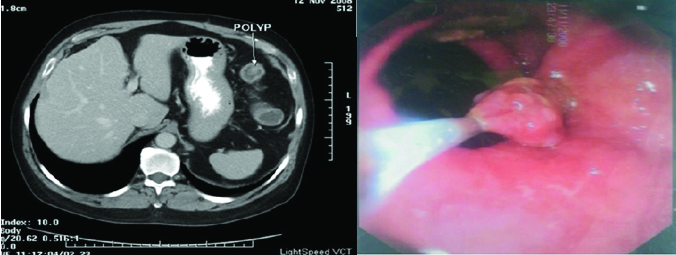
CT axial image showing a colonic polyp. Same was confirmed on colonoscopy.
Statistical analysis in terms of sensitivity, specificity, positive predictive value, negative predictive value and the kappa statistics.
| Statistical Analysis | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | Kappa |
|---|
| Appendicitis | 100 | 100 | 100 | 100 | 1 |
| Inflammatory Bowel Disease | 96.3 | 100 | 100 | 97.0 | 0.94 |
| Bowel Perforation | 100 | 100 | 100 | 100 | 1 |
| Malignancy | 100 | 100 | 100 | 100 | 1 |
| Others (Hernia’s, Diverticulum, polyps) | 100 | 100 | 100 | 100 | 1 |
Discussion
The introduction of MDCT has transformed an axial imaging modality into a volumetric one and allows the radiologist to display a finding in any desired plane. The creation of MPR images increases confidence in identifying the lesion and in diagnosing or excluding the bowel pathology. Some of the factors that cause difficulty in the diagnosis of lesion at axial CT can be overcome with MPR. In addition, a coronal MPR image can help clinicians and radiologists, since it is analogous to a conventional abdominal radiograph. Abdomen imaging with spiral CT, the area to be scanned is typically 40–60 cm from the lung bases to the pubis. CT can cover the entire abdomen and display high resolution images.
A 64 slice MDCT is one such non-invasive modality with excellent sensitivity and specificity. The present study was thus, undertaken to evaluate the diagnostic accuracy of 64 multi-slice CT in assessing bowel pathology in symptomatic patients and compare the findings with intraoperative findings, colonoscopy or with the specific treatment.
Out of the 60 patients 12 were reported with CT findings of appendicitis. The same number of patients got operated subsequently. The intraoperative findings were consistent with the CT findings in all patients. Thus, sensitivity and specificity of MDCT in diagnosing appendicitis was 100%. Our results were almost consistent with the study conducted by Thoeni RF et al., [9].
The overall sensitivity of MDCT for diagnosing inflammatory bowel is 96.3% and the specificity is 100%. Three cases were reported as mesenteric ischemia (ischaemic colitis) and vascular occlusion. They subsequently underwent triple phase study which confirmed thrombus in SMA in first case, thrombus in segmental branch of SMA in second case and thrombus in SMV in the third case. Our results were consistent with the study done earlier by Mazzeo S et al., [10]. The sensitivity of MDCT in diagnosing bowel perforation in our study was 100% which is almost consistent with the study done by Hainaux B et al., [11]. In three cases findings were suggestive of malignancy one was seen which growth at recto-sigmoid junction and two were seen with mass growth at hepatic flexure of colon. They underwent colonoscopy and out of three cases, two revealed mitotic growth. One was diagnosed with inflammatory thickening. However, our study varies mildly compared to early studies may be due to less number of cases. Sixteen patients had findings which included hernias, diverticula and polyps. The same was confirmed on either surgery or on colonoscopy, thus sensitivity and specificity of our study was 100% and 100% respectively.
Limitation
The patients with deranged renal functions and suspected bowel disease could not be included in the study. Pregnant females with suspected inflammatory or infective bowel pathology were excluded from the study. Because of the radiation concern, the study mostly remained confined to adults.
Conclusion
Multi–detector has revolutionized axial imaging into volumetric one and the images can be displayed in any desired plane. Thin collimation (0.5–1.25 mm sections) and fast scanning resulted in mesenteric vessels visualization on routine basis. This in turn lead to improved 3D vascular maps, used in cancer staging, surgical planning. The post processing of volume by MPR/curved MPR images increases confidence in diagnosing or excluding acute appendicitis. Some of the factors that cause difficulty in the visualization of normal Appendix or inflamed Appendix on axial images can be overcome with MPR. Coronal MPR images simulate conventional abdominal radiograph and can help clinicians also to understand the bowel anatomy and pathology better.
[1]. Freeman A H, CT and bowel diseasesBJR 2001 74:4-14. [Google Scholar]
[2]. Hong S, Kim A, Byun J, Won H, Kim P, Lee M, MDCT of small-bowel disease value of 3D imagingAJR 2006 187:1212-21. [Google Scholar]
[3]. Hartmann D, Schilling D, Bolz G, Riemann JF, Capsule endoscopy, technical impact, benefits and limitationsLangenbecks Arch Surg 2004 389:225-33. [Google Scholar]
[4]. Maglinte DD, Bender GN, Heitkamp DE, Lappas JC, Kelvin FM, Multidetector-row helical CT enteroclysisRadiol Clin North Am 2003 41:249-62. [Google Scholar]
[5]. Horton KM, Fishman EK, The current status of multidetector row CT and 3D imaging of small bowelRadiol Clin North Am 2003 41:199-212. [Google Scholar]
[6]. Lewis BS, Swain P, Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: results of a pilot studyGastrointest Endosc 2002 56:349-53. [Google Scholar]
[7]. Voderholzer WA, Beinhoelzl J, Rogalla P, Murrer S, Schachschal G, Lochs H, Small bowel involvement in Crohn’s disease: a prospective comparison of wireless capsule endoscopy and CT enteroclysisGut 2005 54:369-73. [Google Scholar]
[8]. Voderholzer WA, Ortner M, Rogalla P, Beinholzl J, Lochs H, Diagnostic yield of wireless capsule enteroscopy in comparison with CT enteroclysisEndoscopy 2003 35:1009-14. [Google Scholar]
[9]. Thoeni RF, Moss AA, Schnyder P, Margulis AR, Detection and staging of primary rectal and rectosigmoid cancer by computed tomographyRadiology 1981 141:135-38. [Google Scholar]
[10]. Mazzeo S, Caramella D, Battolla L, Melai L, Masolino P, Bertoni M, Crohn disease of the small bowel: spiral CT evaluation after oral hyperhydration with isotonic solutionJ Comput Assist Tomogr 2001 25(4):612-16. [Google Scholar]
[11]. Hainaux B, Bertinotti E, Maertelaer V, Rubesova E, Capellutoet E, Accuracy of MDCT in predicting site of gastrointestinal tract perforationAJR 2006 187:1179-83. [Google Scholar]