Comparison of Intubating Conditions using Fentanyl plus Propofol Versus Fentanyl plus Midazolam during Fiberoptic Laryngoscopy
Parmod Kumar1, Tripat Kaur2, Gurpreet Kaur Atwal3, Jatinderpaul Singh Bhupal4, Ajay Kumar Basra5
1 Professor and Head, Department of Anaesthesiology and Intensive Care, GMC and RH, Patiala, Punjab, India.
2 Associate Professor, Department of Anaesthesiology and Intensive Care, GMC and RH, Patiala, Punjab, India.
3 Junior Resident, Department of Anaesthesiology and Intensive Care, GMC and RH, Patiala, Punjab, India.
4 Retired Professor and Head, Department of Anaesthesiology and Intensive Care, GMC and RH, Patiala, Punjab, India.
5 Junior Resident, Department of Anaesthesiology and Intensive Care, GMC and RH, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gurpreet Kaur Atwal, 44-B, New Kangra Colony, Near A.V. Partap School, Amritsar-143006, Punjab, India. E-mail : preetatwal14@gmail.com
Introduction
Awake nasal or oral flexible fiberoptic intubation is the airway management technique of choice in known or anticipated difficult airway, unstable cervical fracture, limited mouth opening (as in temporomandibular joint disease), mandibular-maxillary fixation and severe facial burns. Both optimal intubating condition and patient comfort are important for fiberoptic intubation. Optimal intubating conditions provided by an ideal sedation regimen would ensure haemodynamic stability, patient comfort, attenuation of airway reflexes and amnesia.
Aim
To compare the intubating conditions using fentanyl plus propofol versus fentanyl plus midazolam during fiberoptic laryngoscopy.
Materials and Methods
A prospective, comparative and randomized study was conducted on 60 patients of either gender aged between 18 and 60 years belonging to the American Society of Anaesthesiologists (ASA) grade-I or II scheduled for elective surgery. Patients were randomly allocated into two groups of 30 each. In group I, patients received i.v. fentanyl 1 μg/kg+ propofol 1 mg/kg to achieve an adequate level of sedation that is Ramsay Sedation Scale (RSS) score of 3. In group II, patients received i.v. fentanyl 1 μg/kg + midazolam 0.03 mg/kg to achieve RSS= score of 3. Haemodynamic parameters (heart rate, systolic and diastolic blood pressure, mean arterial pressure), SpO2, EtCO2, total comfort scale values and patient’s tolerance were assessed during preoxygenation, fiberscope insertion and endotracheal intubation.
Results
Fentanyl plus midazolam group showed better patient comfort and maintenance of oxygen saturation than fentanyl plus propofol group during fiberoptic intubation.
Conclusion
Both fentanyl plus midazolam and fentanyl plus propofol regimes are suitable for fiberoptic intubation. Fentanyl plus midazolam appeared to offer better tolerance, preservation of an airway and spontaneous ventilation, while maintaining haemodynamic stability.
Patient’s tolerance, Ramsay sedation scale, SpO2, Total comfort scale
Introduction
Awake nasal or oral flexible fiberoptic intubation is an airway management technique of choice in known or anticipated difficult airway, unstable cervical fracture, severe cervical stenosis, vertebral artery insufficiency, chiari malformation, limited mouth opening (as in temporomandibular joint disease), mandibular-maxillary fixation and severe facial burns [1].
Fiberoptic intubation can be performed awake, under sedation with or without topical anaesthesia or with muscle relaxant (suxamethonium, vecuronium, rocuronium, atracurium). Both optimal intubating conditions and patient comfort are necessary for fiberoptic intubation. Optimal intubating conditions provided by an ideal sedation regimen would ensure haemodynamic stability, patient comfort, attenuation of airway reflexes and amnesia during fiberoptic laryngoscopy. For sedation, drugs such as fentanyl, midazolam, propofol, dexmedetomidine and remifentanil may be used. Each drug has its advantages and disadvantages. The use of fentanyl or other narcotics reduces the discomfort and haemodynamic changes associated with airway instrumentation [2,3].
Fentanyl is a phenylpiperidine derivative synthetic opioid agonist that is structurally related to meperidine and binds mu (μ) opioid G protein - coupled receptor [4].
Benzodiazepines exert pharmacologic effects by facilitating the action of GABA. Midazolam is water soluble and an ultrashort acting benzodiazepine derivative and used for conscious sedation [5,6]. Rolo R et al., and Rodrigues AJ et al., reported that fiberoptic bronchoscope intubation according to the conscious sedation protocol with midazolam and midazolam plus fentanyl respectively is effective and safe and does not affect significant haemodynamic changes in management of patients with difficult airway [7,8].
Propofol (2,6-diisopropylphenol) is a short-acting, intravenously administered hypnotic agent. It is used for the induction and maintenance of general anaesthesia, sedation for mechanically ventilated patients and procedural sedation [9].
Crawford M et al., reported oxygen saturation decreased in both midazolam and propofol groups, but the decrease was greater in propofol group in outpatient bronchoscopy [10].
The aim of this study was to compare different drugs that produce better intubating conditions with minimal or no side effects during fiberoptic laryngoscopy, the present study was conducted using fentanyl plus propofol versus fentanyl plus midazolam.
Materials and Methods
This prospective, comparative and randomized study was conducted on 60 patients aged between 18 and 60 years, belonging to the ASA grades I and II, scheduled for elective surgeries under general anaesthesia after obtaining approval from Ethical Committee, Government Medical College, Patiala, Punjab, India. A written informed consent was obtained from each patient after explaining the technique in vernacular language before including them in this study. With a power of 0.9 and type one error of 0.05, we calculated the sample size of at least 10 patients in each group, based on the result of previous study. As there is no upper limit of sample size and due to availabiliity of logistic support, 30 patients were taken in each group. Randomization was done by simple sealed envelope method. Exclusion criterias were patient’s refusal and being allergic to the drugs involved in the study, a history of hypertension/ or diabetes mellitus/ or bronchial asthma, previous nasal surgery/nasal trauma, severe bradycardia, any type of A-V block in ECG, thrombocytopenia, coagulopathy, liver cirrhosis, nasal polyp, mental illness patients, pregnancy and drug abuse.
Preparation of Patients
All patients received injection of glycopyrrolate (0.2 mg) as premedication 30 min before the procedure and 2% lignocaine viscous gargles were done to achieve adequate topical anaesthesia. Nasal mucosa was sprayed with xylometazoline 0.1% vasoconstrictor. Each nostril was checked for patency. The nostril with least resistance was chosen for nasal intubation and nasal mucosa was sprayed with two puffs of 10% lignocaine. A nasopharyngeal dilator with lignocaine jelly was introduced. For further topical anaesthesia two puffs of 10% lignocaine were sprayed to tonsillar pillars and back of the throat.
Transtracheal block was performed by piercing the cricothyroid membrane in the midline of the neck with 4 ml of 4% lignocaine. Instillation of local anaesthetic invariably results in coughing that leads to dispersion of the drug, diffusely blocking the sensory nerve endings of the recurrent laryngeal nerve [11].
Group I patients received i.v. fentanyl 1 μg/kg+ propofol 1 mg/kg to achieve an adequate level of sedation that is RSS score of 3. Group II patients received i.v. fentanyl 1 μg/kg + midazolam 0.03 mg/kg to achieve RSS= score of 3.
Fiberoptic nasotracheal intubation was carried out in both groups of patients. Once tracheal intubation was completed and the tube was secured, general anaesthesia was administered. Haemodynamic parameters including Heart Rate (HR), Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP), SpO2 and EtCO2 were recorded during preoxygenation, fiberscope insertion (1,2,3,4 and 5 min. intervals) and endotracheal intubation (1,2,3,4 and 5 min. intervals). Comfort scale value and patient’s reaction to placement of endotracheal tube were assessed during preoxygenation, fiberscope insertion (1,2,3,4 and 5 min. intervals) and endotracheal intubation (1,2,3,4 and 5 min. intervals). The surgical procedure then performed as planned.
The total comfort score for each patient was calculated by summing the scores of the seven comfort categories at each time point. The total score was 35 [Table/Fig-1]. Patient’s tolerance [12] was assessed by an independent observer on the basis of 5 point Fiber Optic Index (FOI) score: No reaction (1); Slight grimacing (2); Severe grimacing (3); Verbal objection (4); Defensive movement of head, hands or feet (5).
Comfort scale, as modified by Ambuel B et al., [12]
| Parameter | 1 | 2 | 3 | 4 | 5 |
|---|
| Alertness | Deeply asleep | Lightly asleep | Drowsy | Fully awake and alert | Hyper-alert |
| Calmness | Calm | Slightly anxious | Anxious | Very anxious | panicky |
| Respiratory response | No coughing and no sponta-neous respiration | Spontaneous respiration | Occasional cough | Coughing regularly | Frequent coughing or choking |
| Crying | Quiet breathing, no crying | Sobbing or gasping | Moaning | Crying | Screaming |
| Physical movement | No movement | Frequent slight movement | Vigorous movement limited to the extremities | Vigorous mov-ements including torso and head | Occasional slight movement |
| Muscle movement | Muscles totally relaxed, no muscle movement | Reduced muscle tone | Normal muscle tone | Increased muscle tone and flexing of fingers and toes | Extreme muscle rigidity and flexing of fingers and toes |
| Facial tension | Facial muscle totally relaxed | No facial tension evident | Tension evident throughout facial muscle | Facial muscle contorted | Grimacing |
*Total score=35
Statistical Analysis
Statistical analysis was conducted using IBM SPSS statistics (version 22.0). Numerical data were expressed as mean and standard deviation and statistical analysis was performed using the independent t-test to compare the scores of the two groups. For skewed data/scores Mann-Whitney U-test was conducted. Gender was compared using Chi-square test. A p-value of <0.05 was considered as statistically significant.
Results
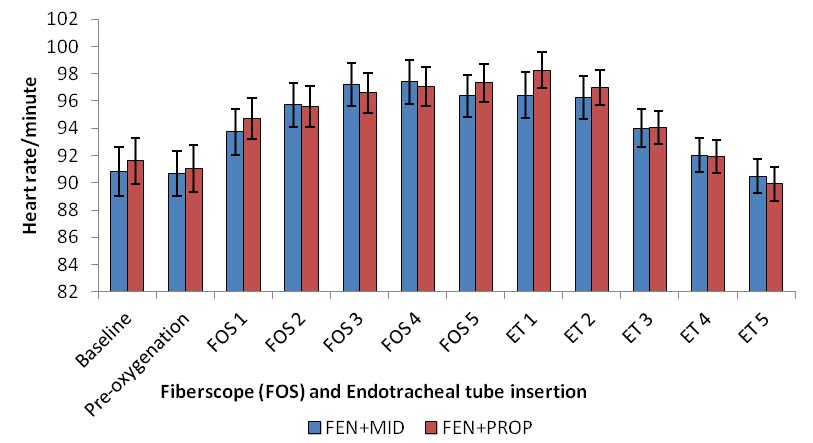
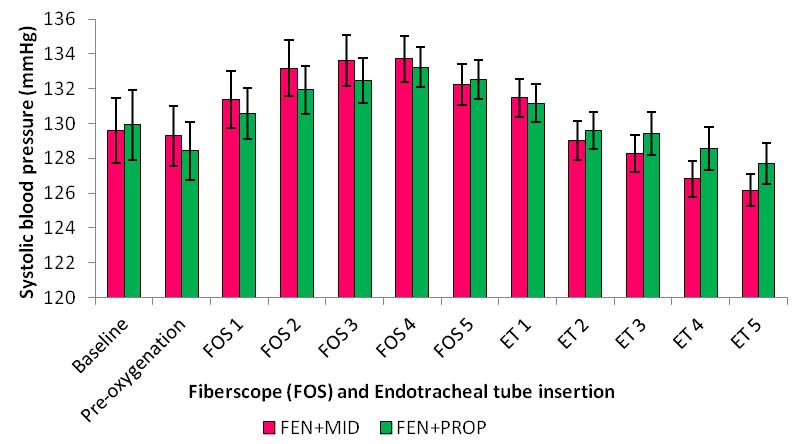
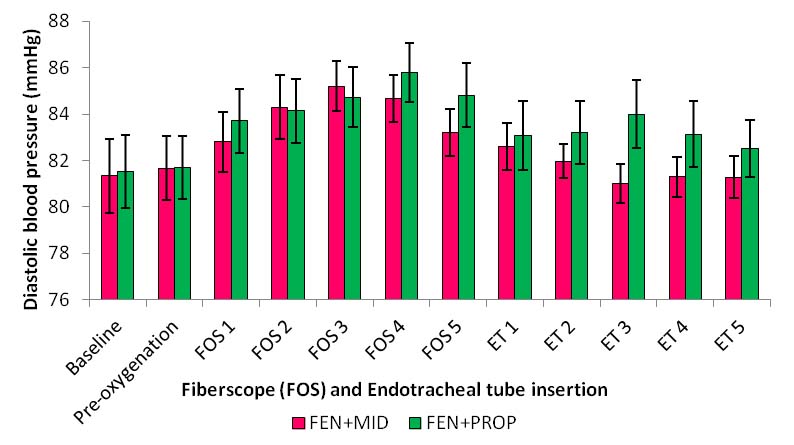
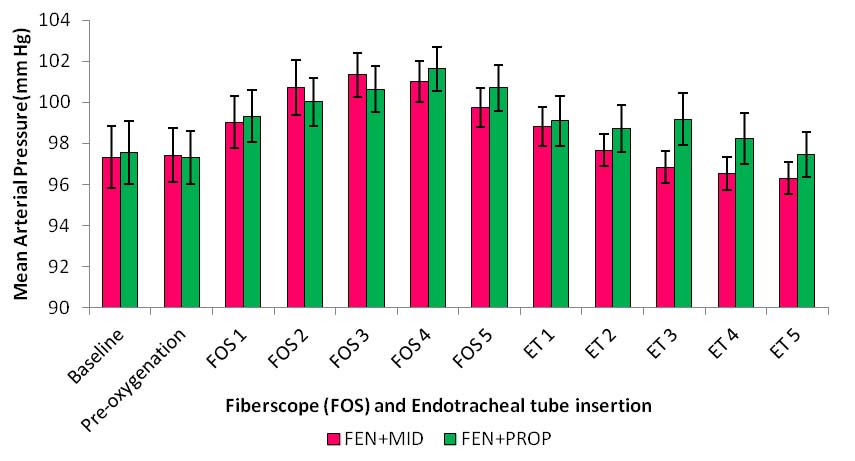
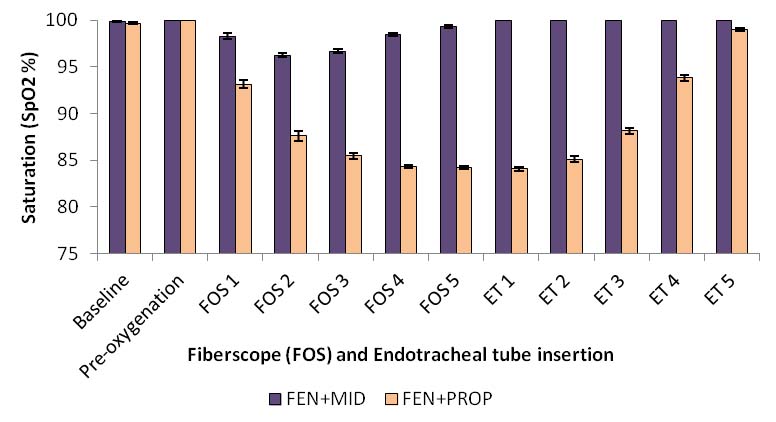
The scores of both groups were compared demographically [Table/Fig-2]. All patients in both groups underwent uncomplicated fiberoptic intubation. The differences in mean HR, SBP, DBP and MAP were statistically insignificant among both groups during preoxygenation, fiberscope insertion and Endotracheal Tube (ET) placement [Table/Fig-3,4,5 and 6]. The mean SpO2 was significantly lower in Group I compared to Group II during Fiberscope (FOS) and ET placement [Table/Fig-7]. No significant difference was found in EtCO2 readings and sedation among either group. Total comfort scores were lower in Group II (they were more calm) during FOS and ET compared to those in Group I. Group I had high five point FOI score, implying better patient tolerance in Group II [Table/Fig-8-9].
| Group | Group I (Fentanyl + Propofol), Mean±SD | Group II (Fentanyl + Midazolam), Mean±SD | p-value | Significance |
|---|
| Age(years) | 43.73±12.15 | 39.87±12.24 | 0.244 | NS |
| Weight(kg) | 63.55±4.47 | 62.60±6.82 | 0.091 | NS |
| Sex(F/M) | 20/10 | 17/13 | 0.42 | NS |
Comparison of HR baseline, during preoxygenation, fiberscope and ET insertion in groups I and II.
Comparison of SBP baseline, during preoxygenation, fiberscope and ET insertion in groups I and II.
Comparison of DBP baseline, during preoxygenation, fiberscope and ET insertion in groups I and II.
Comparison of MAP baseline, during preoxygenation, fiberscope and ET insertion in groups I and II.
Comparison of saturation (SpO2%) baseline, during preoxygenation, fiberscope and ET insertion in groups I and II.
Total comfort score (Mann -Whitney U-test).
| Time Interval | Group I(Fentanyl +Propofol) | Group II(Fentanyl +Midazolam) | p-value | Significance |
|---|
| Mean | SD | Mean | SD |
|---|
| During Preoxgenation | 13.27 | 0.94 | 12.87 | 1.38 | 0.74 | NS |
| During FOS | 13.60 | 0.85 | 12.70 | 1.29 | 0.001 | HS |
| During ET | 13.80 | 1.21 | 13.13 | 0.86 | 0.035 | S |
Patient’s Tolerance based on 5 point Fiberoptic Index Score (Mann-Whitney U-test).
| Group | Group I(Fentanyl +Propofol) | Group II(Fentanyl +Midazolam) | p-value | Significance |
|---|
| Mean | SD (±) | Mean | SD (±) |
|---|
| Fiberscope insertion | 3.23 | 0.81 | 2.70 | 0.91 | 0.01 | S |
| Endotracheal tube | 2.43 | 1.00 | 1.93 | 0.58 | 0.002 | S |
Discussion
Awake nasal or oral flexible fiberoptic intubation is the airway management technique of choice in patients with anticipated difficult airway. Both optimal intubating conditions and patient comfort are necessary for fiberoptic intubation. Optimal intubating conditions provided by an ideal sedation regimen would ensure haemodynamic stability, patient comfort, attenuation of airway reflexes and amnesia during fiberoptic laryngoscopy. The primary outcome of our study showed that both fentanyl plus propofol and fentanyl plus midazolam regimes provide adequate conditions for fiberoptic intubation. Both groups underwent uncomplicated fiberoptic intubation. No significant difference was found in HR, SBP, DBP and MAP between the two groups. These findings are similar to those reported in the studies conducted by Crawford M et al., Falkman H et al., and Clarkson K et al., who found no significant difference in haemodynamics parameters among propofol and midazolam groups during fiberoptic laryngoscopy [10,13,14]. However, study conducted by Grendelmier P et al., on comparative evaluation of propofol and midazolam as sedative agents concluded that patient randomized to propofol showed more episodes of hypotension [15]. It might be due to the dose of propofol used in the study. The median dose of propofol used was 310 mg corresponding to 4.69 mg/kg compared to 1 mg/kg in our study.
The mean SpO2 was significantly lower in Group I compared to Group II during FOS and ET placement. These findings were similar to those reported by Grandelmeir P et al., who conducted study on comparative evaluation of propofol and midazolam as sedative agents in 90 consecutive patients undergoing medical thoracoscopy and observed that patients randomized to propofol group showed more episodes of hypoxia [15]. Tsai CJ et al., in their study concluded that airway obstruction and hypoxia occurred more frequently in the propofol group than in the dexmedetomidine group [16]. Crawford M et al., also showed the same result in their study [10]. However, the study conducted by Bailey PL et al., showed that midazolam alone does not produce ventilatory depressant effects in healthy volunteers [17], but the combination of midazolam (0.05 mg/kg) and fentanyl (2 μg/kg) i.v. resulted in hypoxemia and/or hypoventilation. In our study, no ventilatory depression and no decrease in arterial saturation was observed in patients receiving midazolam and fentanyl. It might be because of the dose of midazolam (0.03 mg/kg) and fentanyl (1 μg/kg) used in study which was just adequate for procedural sedation without causing respiratory depression.
Total comfort scores were lower in Group II (they were more calm) during FOS and ET compared to Group I. Group I had high five point FOI scores implying better patient tolerance than Group II. These findings are corroborated by the studies conducted by Rolo R et al., Rodrigues AJ et al., and Dhasmana S et al., show that midazolam and fentanyl provide better intubating conditions, patient comfort and tolerance in fiberoptic bronchoscopy [7,8,18]. However, the study conducted by Falkman H et al., in their study concluded that propofol shows more homogeneous satisfaction score [13]. The reason for this was the propofol dose used in this study was higher than that used in our study.
It can be concluded, that the use of midazolam (0.03 mg/kg) and fentanyl (1 μg/kg) is safe and effective in patients undergoing fiberoptic laryngoscopy offering conscious sedation, better tolerance and comfort while maintaining oxygen saturation without any haemodynamic alteration.
[1]. Artime C, Flexible fiberoptic intubation. In CA Hagberg, WH Daily, editorsThe Difficult Airway: A Practical Guide 2013 OxfordOxford University Press:97 [Google Scholar]
[2]. Lallo A, Billard V, Bourgain JL, A comparison of propofol and remifentanil target control infusion to facilitate fiberoptic nasotracheal intubationAnaesth and Anal 2009 108:852-57. [Google Scholar]
[3]. Stamenkovic DM, Hassid M, Dexmedetomidine for fiberoptic intubation of a patient with severe mental retardation and atlantoaxial instabilityActa Anaethesiol Scand 2006 50:1314-15. [Google Scholar]
[4]. Bentley JB, Borel JD, Nenad RE Jr, Gillespie TJ, Age and fentanyl pharmacokineticsAnaesth Analog 1982 61:968-71. [Google Scholar]
[5]. Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ, Midazolam: Pharmacology and usesAnaesthesiology 1985 62:310-24. [Google Scholar]
[6]. Brown CR, Sarnquest FH, Carup CA, Pedley TA, Clinical, EEG, Pharmacokinetic studies of water soluble benzodiazepine midazolam maleateAnaesthesiology 1979 50:467-70. [Google Scholar]
[7]. Rolo R, Mota PC, Coelha F, Alves D, Fernandes G, Cunha J, Sedation with midazolam in flexible bronchoscopy- A prospective studyRev Port Pneumol 2012 18:226-32. [Google Scholar]
[8]. Rodrigues AJ, Scordamagilo PR, Palomino AM, Oliveira EQ, Jacomelli M, Figueiredo VR, Difficult airway intubation with flexible bronchoscopeRev Bras Anestesiol 2013 63:358-61. [Google Scholar]
[9]. Stoelting RK, Hillier SC, Hillier Pharmacology and Physiology in Anaesthetic Practice 2006 4th ednLippincott Williams and Wilkins:154 [Google Scholar]
[10]. Crawford M, Pollock J, Anderson K, Glavin RJ, Macintyre D, Vernon D, Comparison of midazolam with propofol for sedation in outpatient BronchoscopyBr J Anaesth 1993 70(4):419-22. [Google Scholar]
[11]. Furlan JC, Anatomical study applied to anaesthetic block technique of the superior laryngeal nerveActa Anaesthesiol Scand 2002 46:199-202. [Google Scholar]
[12]. Ambuel B, Hamlett KW, Marx CM, Blumer JL, Assessing distress in Pediatric Intensive Care Env: The Comfort ScaleJ Pediatr Psychol 1992 17(1):95-109. [Google Scholar]
[13]. Falkmann H, Lemogne M, Baighezale S, Choufane S, Eurin B, Intravenous sedation for fiberoptic intubation: comparison of propofol vs midazolam/alfentanilEur J Anaesthesiol 2001 18:6-7. [Google Scholar]
[14]. Clarkson K, Power CK, O’Connell F, Pathmakanthan S, Burke CM, A comparative evaluation of propofol and midazolam as sedative agents in fiberoptic bronchoscopyChest 1993 104(4):1029-31. [Google Scholar]
[15]. Grendelmeier P, Tamm M, Jahn K, Pflimlin E, Stolz D, Propofol versus midazolam in medical thoracoscopy: A randomized, noninferiority trialRespiration 2014 88:26-36. [Google Scholar]
[16]. Tsai CJ, Chu KS, Chen TI, Lu DV, Wang HM, Lu IC, A comparison of the effectiveness of dexmedetomidine versus propofol target-controlled infusion for sedation during fibreoptic nasotracheal intubationAnaesthesia 2010 65:254-59. [Google Scholar]
[17]. Bailey PL, Pace NL, Ashburn MA, Moll JW, East KA, Stanley TH, Frequent hypoxemia and apnea after sedation with midazolam and fentanylAnaesthesiology 1990 73:826-30. [Google Scholar]
[18]. Dhasmana S, Singh V, Pal US, Awake blind nasotracheal intubation in temporomandibular joint ankylosis patients under conscious sedation using fentanyl and midazolamJ Maxillo Oral Surg 2010 9(4):377-81. [Google Scholar]