The vaginal flora of healthy adult women of reproductive age group constitutes predominantly the Lactobacilli [1]. The vaginal flora can be altered by different factors, including antimicrobial, contraceptive use and douching [2]. Many studies have been done to establish the relationship between contraceptives and Bacterial Vaginosis (BV) by different authors.
Contraceptives can produce inflammation and morphologic atypia in both squamous and endo cervical columnar cells. Mostly these atypias are benign, representing degenerative or reparative changes [3].
Some studies suggest increase risk of cervical cancer with consumption of OCPs for a longer time although no consistent association is observed [4]. No significant epithelial or glandular abnormalities are seen in women using condoms [5].
This study was conducted to compare effects of various contraceptive methods on cervico-vaginal smear.
Materials and Methods
This two years prospective study was conducted in the Department of Pathology at Subharti Medical College, Meerut between June 2014 and July 2016. Study was conducted on 120 symptomatic and asymptomatic women (women presenting with gynaecological complaints or came for follow up without any complaints) attending Obstetrics and Gynaecology outpatient department using different methods of contraception. Ethical clearance was procured from ethical committee of the institute; also informed written consent was taken from the patients. A control group comprising of 60 symptomatic as well as asymptomatic women not using any contraception were included in the study. Exclusion criteria included inadequate Pap smear, patients presenting with cervical polyp or uterine prolapsed, patients on antibiotic therapy or using intravaginal drugs.
Two smears were taken in every patient. One Pap stained cervical smear for cytology and the other Gram stained vaginal smear for studying the vaginal flora. Cervical smears were reported using the Bethesda system and vaginal smears were scored using Nugent scoring for BV [6]. By using Nugent scoring [6] the vaginal flora was categorised on the basis of type and number of bacteria per Oil Immersion Field (OIF) into normal, intermediate or BV group (Score 0-3, 4-6 and 7-10 respectively) [Table/Fig-1].
| Organism Morphotype | No./ OIF | SCORE |
|---|
| Lactobacillus (parallel sided, Gram positive bacilli) | >30 | 0 |
| 5-30 | 1 |
| 1-4 | 2 |
| <1 | 3 |
| 0 | 4 |
| Mobiluncus (curved Gram negative bacilli) | >5 | 2 |
| 1-4 | 1 |
| 0 | 0 |
| Gardnerella/Bacteroides (tiny, Gram variable coccobacilli, pleomorphic Gram negative bacilli with vacuoles) | >30 | 4 |
| 5-30 | 3 |
| 1-4 | 2 |
| <1 | 1 |
| 0 | 0 |
*OIF-Oil Immersion Field
Statistical analysis was done using SPSS (Statistical Package for the Social Sciences) software for Windows Version 19.0 and test of significance we applied was chi-square test. A p-value <0.05 was considered significant.
Results
Age of patients in the control group as well as the study group ranged from 20 to 44 years (with a mean of 32.31±6.47 years and 31.76±5.25 years respectively). Out of 120 contraceptive users, the most common method used was barrier (68.3%) followed by tubal ligation (14.2%), IUCD (9.2%), OCPs (6.6%) and injectable method (1.7%).
The most common complaint was pain lower abdomen (26.6% cases in the control group and 46.7% cases in the study group) followed by menstrual complaints (26.6% cases in the control group and 22.5% cases in the studied group). Few of the patients had more than one presenting complaints.
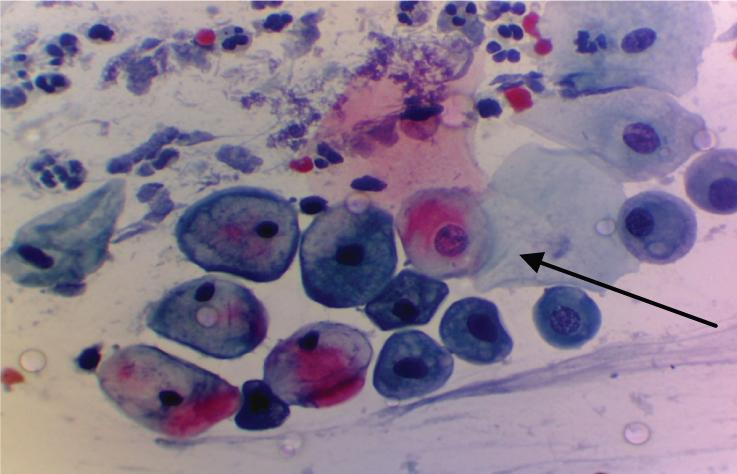
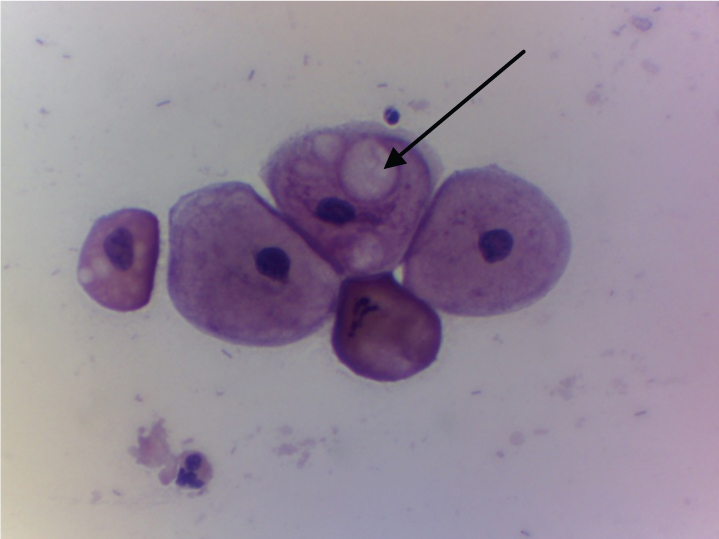
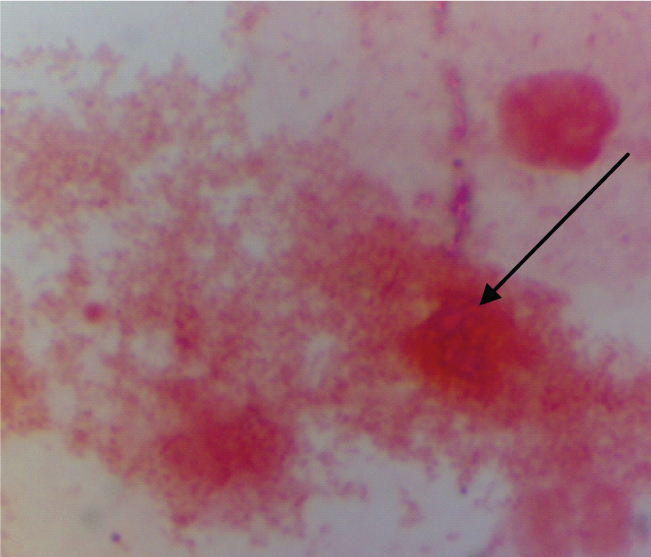
The most common findings in the control group were normal cervical smear and NILM (Negative for Intraepithelial Lesion or Malignancy) with metaplastic cells [Table/Fig-2] followed by NILM with reactive changes [Table/Fig-3]. While in the study group commonest epithelial change observed was NILM with reactive changes followed by NILM with metaplasia, koilocytotic changes, cytolytic effect, satellitosis, intracytoplasmic vacuoles and clue cells [Table/Fig-4] as shown in [Table/Fig-5]. In rest of the smears only inflammatory cervical changes were observed.
Shows metaplastic changes (arrow) (Pap stain 40X).
Shows reactive cellular change (intra-cytoplasmic vacuolations) (arrow) (Pap stain 40X).
Shows bacterial vaginosis (arrow) (Gram stain 40X).
Epithelial changes observed in different contraceptive methods and control group.
| Changes | Different Contraceptive Methods | Control Group |
|---|
| Barrier | Tubal ligation | IUCD | OCPs | Injectable | Total (n= 120) | Total (n=60) |
|---|
| NILM with reactive changes | 40 (48.7%) | 07 (41%) | 04 (36.3%) | 02 (25%) | 01 (50%) | 54 (45%) | 05 (8.3%) |
| NILM with metaplastic changes | 19 (23%) | 03 (17.6%) | 03 (27.2%) | 04 (50%) | 01 (50%) | 30 (25%) | 07 (11.7%) |
| Koilocytotic changes | 03 (3.6%) | 03 (17.6%) | - | - | - | 06 (5%) | - |
| Cytolytic effect | 04 (4.8%) | 01 (5.9%) | 01 (9%) | - | - | 06 (5%) | - |
| Satellitosis | 02 (2.4%) | - | 03 (27.2%) | - | - | 05 (4.2%) | 01 (1.7%) |
| Clue cells | 01 (1.2%) | - | - | 01 (12.5%) | - | 02 (1.7%) | 01 (1.7%) |
| No epithelial change (NILM) | 0 | 0 | 0 | 0 | 0 | 0 | 08 (13.3%) |
χ2 value= 43.96; p-value < 0.001 (sig.)
NILM with reactive changes were the commonest epithelial change observed in majority of different contraceptive users (barrier-48.7%, tubal ligation-41.0%, IUCD-36.3%) except for the hormonal users in whom NILM with metaplastic changes were more frequently observed (50%). Other changes like satellitosis were more common in IUCD users (27.2%), koilocytotic changes in ligated patients (17.6%) and clue cells in hormonal users (12.5%) as shown in [Table/Fig-5].
Among the control group majority of females had normal flora (81.7%), followed by intermediate or altered flora (13.3%) and 5% had BV. Among all the contraceptive users 51.7% of the patients had normal flora (Nugent score 0-3, which comprises of more number of Lactobacilli and Mobiluncus per OIF and absent or less number of Gardnerella per OIF), followed by intermediate or altered flora (30.0%) (Nugent score 4-6, intermediate number of bacteria) and rest had BV (18.3%) (Nugent score 7-10, which comprises of more number of Gardnerella and less number of Lactobacilli and Mobiluncus per OIF) [Table/Fig-6]. Scoring criteria is explained in [Table/Fig-1].
Distribution of vaginal flora in the control group and cases.
| Type of flora | Control group | Cases | p–value (z) |
|---|
| Normal flora | 49 (81.7%) | 62 (51.7%) | <0.001 |
| Intermediate/ Altered flora | 08 (13.3%) | 36 (30.0%) | 0.014 |
| Bacterial vaginosis | 03 (5.0%) | 22 (18.3%) | 0.015 |
| Total | 60 | 120 | |
χ2 = 15.50; p-value < 0.001 (sig)
Discussion
Effects of various contraceptive methods on cervical epithelium and vaginal microflora have been studied by various authors but varied results are obtained.
In the present study, majority of the contraceptive users belonged to 26-30 years of age group while least number belonged to 41-44 years of age group. This is comparable to the study conducted by Kumar M et al., in which majority of the contraceptive users belonged to 23-27 years of age group while least contraceptive users belonged to >38 years [7].
In the present study, the most common contraception used was barrier (68.3%) followed by tubal ligation (14.2%). The most common presenting complaint was pain lower abdomen among the study group (46.7%) and the control group (26.6%). In the study conducted by Ocak S et al., vaginal discharge was a frequent complaint present in 76.4% IUCD users and 55.8% OCP users [2]. Agarwal K et al., revealed backache as the most common presenting complaint (54%) followed by vaginal discharge (46%) and pain lower abdomen (34%) [8].
In the present study, among the barrier contraceptive users NILM with reactive changes were observed in 48.7% followed by NILM with metaplastic changes in 23% cases. No epithelial or glandular abnormalities like ASC-US, L-SIL or H-SIL was observed among this group. This is comparable to study conducted by Baris II and Karakaya YA in low rate of epithelial abnormalities were found in barrier method [9]. Similarly Chih HJ et al., observed no significant association between the use of condom and the risk of Cervical Intraepithelial Neoplasia (CIN) [5] while Munk AC et al., and Becker TM et al., observed a protective effect of barrier contraceptive on cervical dysplasia [10,11].
The most common epithelial change observed among the women who had undergone tubal ligation was NILM with reactive changes (41%) followed by NILM with metaplastic change and koilocytotic change (17.6% each). However, no atypical cell was observed among the cases. Study conducted by Kjaer SK et al., found no association between tubal ligation and cervical cancer [12].
In IUCD users, NILM with reactive changes were observed in 36.3% cases followed by NILM with metaplastic changes and satellitosis in 27.2% cases each. Pillay P et al., also revealed benign reactive changes in 70% cases [3].
Among the hormonal contraceptive users, NILM with metaplastic change (50%) was the commonest epithelial change observed in the present study followed by NILM with reactive changes (25%). No epithelial cell abnormalities like dysplasia, ASC-US, L-SIL or H-SIL was observed in the cases. Similarly in the studies conducted by Ocak S et al., Binesh F et al., and Baris II and Karakaya YA no epithelial cell abnormality was observed [2,4,9].
Comparison of vaginal flora: In our study, 51.7% of the cases had normal vaginal flora followed by intermediate or altered flora (30.0%) and rest had BV (18.3%). Majority of the barrier contraceptive users had normal vaginal flora (52.4%) followed by intermediate or altered flora (32.9%) and BV (14.6%). In the control group, normal flora was present in majority of the subjects (81.7%) followed by intermediate or altered flora (13.3%) and BV (5.0%). The result is comparable to the study conducted by Fosch SE et al., in which normal flora was present in 50% of the cases and BV was present in 16.6% cases [13]. To the best of our knowledge all studies showed protective effect of barrier contraception on BV.
However, among the control group normal flora was present in 44.4% subjects and BV in 33.3% subjects. In our study, among different methods of contraception majority of the cases having BV were observed in tubal ligation (35.2%). Similarly the study conducted on patients of tubal ligation by Riggs M et al., showed BV in majority of their cases (66%). However, in our study the cases were less in number [14].
This is followed by hormonal method of contraception (20.0%) and IUCD users (18.1%) in our study. Similar to this, decreased risk of bacterial vaginosis was observed among the hormonal contraceptive users in the studies conducted by Riggs M et al., and Baeten JM et al., on hormonal contraceptive users [14,15] and by Madden T et al., and Donders GG et al., on IUCD users [16,17].
Limitation
As the present study is hospital based and the subjects included in our study were the patients who visited the outpatient department, this might have resulted in some bias. Had the study been conducted on a larger scale, more cases of intraepithelial lesion could have been picked up. Also there was a variation in the number of subjects using different contraceptive methods.
Conclusion
Majority of the women in reproductive age of low socioeconomic status prefer to use barrier. Inflammatory cervical lesions were more common as compared to epithelial abnormalities. The cervico-vaginal changes were more frequent in contraceptive users as compared to the control group. NILM with reactive changes followed by metaplastic changes were the commonest finding in all except hormonal users. Bacterial vaginosis was most commonly observed in tubal ligation followed by hormonal users but it needs further evaluation as number of subjects was less. Thus, benign epithelial changes and alteration in the vaginal flora were more commonly observed in contraceptive users than non users.
*OIF-Oil Immersion Field
χ2 value= 43.96; p-value < 0.001 (sig.)
χ2 = 15.50; p-value < 0.001 (sig)