Pain plays very crucial role in surgery, advantages of good post operative pain control is patient comfort, provides hemodynamic stability, helps in early ambulation, plays important role in fast track surgery and it also prevents progression of acute pain to chronic pain [1,2].
Multi-interventional/rehabilitation strategy is hence required for optimal pain relief. Recognition of these factors has led to the concept of ‘fast Track’ surgery [2]. The concept of fast track surgery enables early discharge which also require optimal pain relief after total hip and knee arthroplasty.
The acute and chronic pain is interrelated as it may progress to chronic pain. It is evident that early analgesic intervention may reduce postoperative chronic pain. There are multiple modalities for post operative pain relief in Total Knee Replacement (TKR)-Epidural infusion, peripheral nerve block (femoral nerve block, saphenous nerve block), local wound infiltration. Local anaesthetic wound infiltration reduces the persistent and neuropathic pain without affecting the motor power which is responsible for early mobilization [3]. The aim of study was to assess the quality of post operative analgesia provided by FNB and LIA in unilateral TKR (postoperatively and decreases the duration of stay.
Materials and Methods
A prospective interventional study was carried out from September 2014 to November 2015, after approval from the Ethical Committee of the Institute. Informed consent was taken from all patient entered into the study. A total of 60 patients were included in the study {the minimum required sample in each group was calculated using Epi info version 7 software with an assumed alpha error of 5% and power of 80%. Average pain score were taken as 2.1 and 1.6 at rest for local infiltration analgesia and femoral block respectively [4]}. The subjects included in the study were of 25-65 years of age group and had ASA grade I or II. Patients more than 65 years, had ASA grade III or IV, had chronic pain or taking chronic opioid medication, were known for allergy to the medications used and had contraindications to performing regional anaesthesia were excluded from the study.
The study was double blind, the patient and reviewer (pain clinic nurse) were unaware. All surgeries were conducted by single surgeon and all anaesthesia and pain management by single anaesthetist. The patients were divided randomly by serial assignment that is first patient was assigned to Group 1 (FNB) and second patient to Group 2 (LIA) and henceforth, in two groups of 30 patients each, scheduled for elective surgery for unilateral TKR.
Each patient in whom FNB or LIA has been given postoperatively had received general anaesthesia intraoperatively. A pneumatic thigh tourniquet inflated to a pressure of 300 mmHg. All patients had gone through pre anaesthetic evaluation and intraoperative monitoring. Equipment used were 18 gauge touhys needle, catheter and lectocath.
Group 1(FNB)
After cleaning and draping, femoral nerve of operated leg was localised with the help of linear ultrasound probe and then touhy needle was proceeded along the long axis of the probe while tracing the tip of the needle the position of needle was rechecked by normal saline before injecting drug. Catheter fixed at the 15 cm on skin. Catheter was attached to infusion pump which consisted of 0.1% of ropivacaine at 6 ml/hr.
Group 2(LIA)
Preparing an injectant mixture which consisted of 0.2 percent ropivacaine HCl, 2.0 mg/ml mixed with 30 mg ketorolac and 10 μg/ml adrenaline. We made 150 ml of solution divided in three equal parts and infiltrated at medial, lateral collateral ligaments and posterior capsule before putting the implant in surgery. Before closure, the drug was infiltrated at wound edges and subcutaneous tissues. Catheter tip was left between posterior capsule and medial condyle. The catheter was secured for further infiltration of 25-30 ml subsequently at 20th hours and 48th hours. After administering the drug, drain was clamped for one hour.
Both groups received multimodal analgesia in the form of Inj Paracetamol 1 gram, eight hourly and SOS. Fentanyl as a rescue analgesia was given. Injection fentanyl was given via patient controlled analgesia pump with concentration of 15 mcg/ml and lock out period of 15 minutes with maximum three times patient can press the button in 15 minutes so total fentanyl demand was calculated by calculating how many times patient pressed the button.
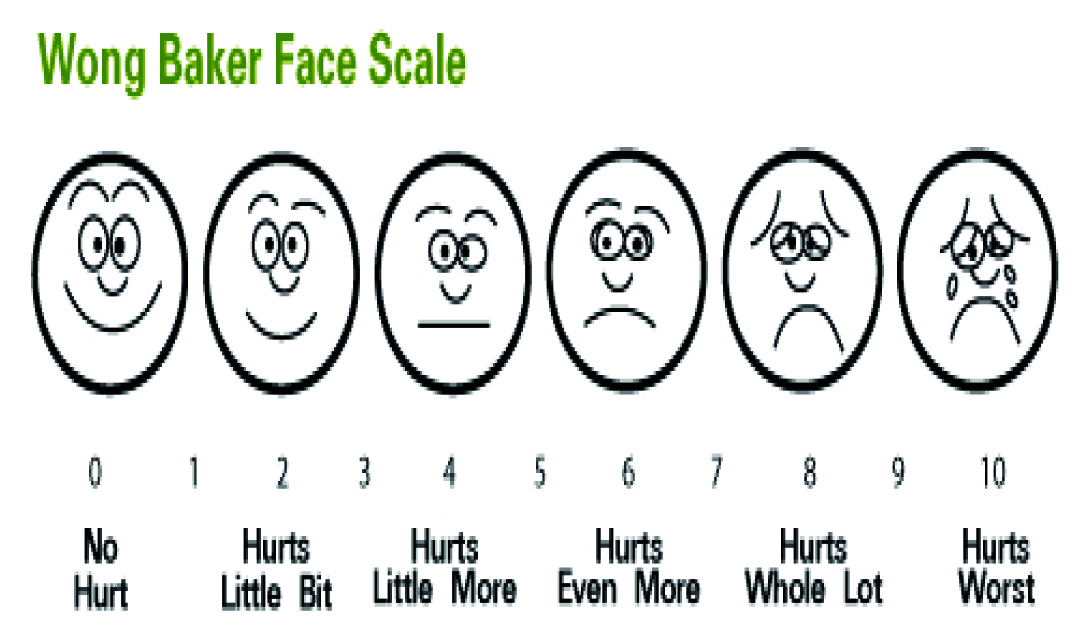
Method of measuring the outcome of interest were by Numeric Rating Scale (NRS) (0-10) [5], [Table/Fig-1]sedation score (0-4) scale [6] [Table/Fig-2], Motor Power Grading (MPG) (0-5) scale [7]. [Table/Fig-3], early mobilization time (at 24 hours of surgery) time interval from zero to until the first walk and free mobilization time (at 48 hours of surgery) from zero to independent mobility.
| Sedation Score | Response |
|---|
| 0 | Awake |
| 1 | Mild sedation, easy to rouse |
| 2 | Moderate sedation, easy to rouse but constantly drowsy |
| 3 | somnolent, difficult to rouse |
| Score | Response |
|---|
| 0 | No movement |
| 1 | Flicker is perceptible in the muscle |
| 2 | Movement only if gravity eliminated |
| 3 | Can move limb against gravity |
| 4 | Can move against gravity and some resisitance exerted by examiner |
| 5 | Normal power |
All blocks and local infiltrations were given by anaesthetist of two years of experience under the guidance of senior consultant who is having experience of 20 years. The pain management nurse was kept unaware of the clinical background of the patients as she was assessing regularly under the guidance of anaesthetist.
Statistical Analysis
Statistical analysis was done by using the SPSS software. The comparison was made using the Chi-square test. It was done by applying independent t-test for those variables which were continuous in nature (NRS). The other four variables were categorical in nature, for the association between the groups Chi-square test was applied. In order to obtain linear trend within a group for those variables which were continuous in nature (NRS), we have applied repeated measurement analysis test followed by Bon N frienni test. In order to see the linear trend in case of categorical variables, we have applied Friedmann test followed by Newman-kallis test. These all variables were normally distributed and sample size was adequate that is why we have applied parametric test.
Results
No serious side effects were observed in the postoperative period. A total of 60 patient of which the most of patients were in the age group 50-60 years i.e., 15 in FNB and 18 in LIA. This was followed by the age group of 61-65 years. Out of 60 patients, 18 patients in FNB and 27 patients in LIA are female, gender distribution is showing female preponderance in both the groups. This may be due to the fact that randomization was done by serial assignment of patients to groups without gender randomization.
Pain score was higher in LIA Group and with the duration there was a gradual decrease in NRS in both the group postoperatively [Table/Fig-4].
Comparison of NRS score in both the groups.
| Group | Mean | Std.Deviation | T-value | p-value | Significance |
|---|
| NRS 4 | FNB | 4.40 | 1.52 | 6.64 | 0.001 | S |
| LIA | 6.57 | 0.94 |
| NRS 8 | FNB | 4.30 | 1.37 | 7.05 | 0.001 | S |
| LIA | 6.43 | 0.94 |
| NRS 12 | FNB | 4.13 | 1.22 | 6.89 | 0.001 | S |
| LIA | 5.93 | 0.74 |
| NRS 16 | FNB | 3.57 | 0.73 | 11.74 | 0.001 | S |
| LIA | 6.00 | 0.87 |
| NRS 20 | FNB | 3.30 | 0.60 | 12.27 | 0.001 | S |
| LIA | 5.40 | 0.72 |
| NRS 24 | FNB | 3.37 | 0.49 | 13.93 | 0.001 | S |
| LIA | 5.37 | 0.61 |
| NRS 48 | FNB | 3.47 | 0.68 | 9.42 | 0.001 | S |
| LIA | 5.10 | 0.66 |
p-value <0.05 is significant; NS - non significant; S - significant. Independent t test used
Sedation score was higher in LIA group and was statistically significant between two groups at 4th, 12th, and 48th hour [Table/Fig-5].
Comparison of Sedation score (SS).
| Group | Score | SS4 | SS8 | SS12 | SS16 | SS20 | SS24 | SS48 |
|---|
| FNB | 0 | 12 | 20 | 25 | 28 | 29 | 27 | 26 |
| 1 | 17 | 9 | 4 | 1 | 1 | 3 | 4 |
| 2 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| LIA | 0 | 3 | 13 | 15 | 24 | 26 | 24 | 19 |
| 1 | 27 | 16 | 14 | 4 | 2 | 5 | 11 |
| 2 | 0 | 1 | 1 | 2 | 2 | 1 | 0 |
| FNB vs LIA | Chi-square | 8.67 | 3.45 | 8.05 | 4.09 | 2.497 | 1.67 | 4.36 |
| p-value | 0.013* | 0.179 | 0.018* | 0.129 | 0.287 | 0.432 | 0.037* |
| Significance | S | NS | S | NS | NS | NS | S |
Significant values, Chi-square test used
LIA Group had higher MPG than FNB Group. Muscle power increased with time in postoperative period in both the group [Table/Fig-6].
| Group | MPG | MPG4 | MPG8 | MPG12 | MPG16 | MPG20 | MPG24 | MPG48 |
|---|
| FNB | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | 14 | 8 | 2 | 1 | 0 | 1 | 1 |
| 3 | 15 | 20 | 25 | 23 | 21 | 16 | 15 |
| 4 | 1 | 2 | 3 | 6 | 9 | 13 | 14 |
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| LIA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3 | 28 | 20 | 13 | 7 | 1 | 0 | 0 |
| 4 | 2 | 10 | 17 | 23 | 29 | 30 | 30 |
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| FNB vs LIA | chi-sqr | 18.26 | 13.33 | 15.59 | 19.5 | 28.71 | 23.72 | 21.82 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Chi-square test used
Early mobilisation were affected (were not able to stand with support also at 24 hours) in three patients (10%) of FNB and 27 patients (90%) of LIA. The result was significant with p-value of <0.001. The motor power was on rising trend from 4th hour to 48th hour in both the group [Table/Fig-7].
Comparison of early mobilization time.
| Early mobilization time | Type of analgesia | Total | Pearson Chi-square value | p-value |
|---|
| FNB | LIA |
|---|
| Affected | 3 | 27 | 30 | 38.4 | <0.001 |
| Unaffected | 27 | 3 | 30 |
| Total | 30 | 30 | 60 |
Chi-square test used
Free mobilisation time had been compared in both group and the difference is statistically insignificant (p-value <0.79). Twelve patients (40%) of FNB and 11(36%) patients of LIA were affected (were not able to move independently at 48 hours) explained in [Table/Fig-8]. For easy calculation of the rescue analgesia, we divided fentanyl demand in four groups: nil, < 5 times, 6-10 times, 11-15 times, 16-20 times. As PCA pump was used with lock out interval of 15 minutes with maximum three times, patient can press the button in 15 minutes with concentration of 15 mcg/ml so total fentanyl demand was calculated by how many times patient pressed the button. Need of rescue analgesia was more in LIA Group [Table/Fig-9].
Comparison of free mobilization time rescue analgesia.
| Free mobilization time | Type of analgesia | Total | Pearson Chi-sqr value | p-value |
|---|
| FNB | LIA |
|---|
| Affected | 12 | 11 | 23 | 0.071 | 0.791 |
| Unaffected | 18 | 19 | 37 |
| Total | 30 | 30 | 60 |
Chi-square test used
Tabular comparison of rescue analgesia.
| Number of time dose required | Type of analgesia | Total | Pearson Chi-sqr value | p-value |
|---|
| FNB | LIA |
|---|
| Rescue analgesia | NIL | 20 | 0 | 20 | 56.33 | <0.001 |
| < 5 times | 7 | 0 | 7 | | |
| 6-10 times | 2 | 0 | 2 | | |
| 11-15 times | 1 | 11 | 12 | | |
| 16-20 times | 0 | 19 | 19 | | |
| Total | 30 | 30 | 60 | | |
Chi-square test used
Discussion
In the present study, we found that NRS was comparatively lower in FNB Group as compared to LIA Group. MPG is on lower side in FNB group, but overall effect on mobilising time remained insignificant although rescue analgesia demand was high in LIA group. Vadivelu N et al., has found that pain management for orthopaedic surgery will depend on how anaesthesiologists use the current available medication and techniques in finding the appropriate technique of analgesia. This includes the drug mixtures, appropriate concentrations, and route of administration for each type of surgery [8]. There is controversy regarding use of ketorolac due to few side effects but we did not encounter any of the side effect [9].
Our study shows that NRS of pain [5], was on decreasing trend with the duration postoperatively in both the groups and it is possible to achieve satisfactory control of pain using LIA but still it remained significantly higher in LIA group.
Carli F et al., have shown that patient receiving FNB had low opioid demand [10]. Both femoral block and LIA resulted in low average pain intensity during the first two postoperative day but in our study, there is a significant difference between the two groups as we compared the NRS scoring where pain relief was less in LIA group. None of the patients in this study were given an analgesic other than intravenous fentanyl via PCA pump, and paracetamol (4 g in 24 hour).
Albrecht E et al., conducted a metanalysis along with a systemic review to see efficacy of periarticular multimodal drug injection in TKA and found remarkable decreased NRS scoring in LIA [11]. Fan L et al., Busch CA et al., Kehlet H et al., Kerr DR et al., Toftdahl K et al., Paul JE et al., Kurosaka et al., were of the same opinion [Table/Fig-10] [12-18].
Comparison of NRS score [12-18].
| Author’s name (year) | Reference no. | Study group | Parameter assessed | Outcome |
|---|
| Fan L et al., | [12] | -- patients for TKR | NRS | LIA had low NRS |
| Busch CA et al., | [13] | 64 patients for TKR | NRS | LIA had low NRS |
| Kehlet H et al., | [14] | 325 patients for THA | NRS | LIA had low NRS |
| Kerr DR et al., | [15] | 325 patients for TKR and THR | NRS | LIA had low NRS |
| Toftdahl K et al., | [16] | 80 patients for TKR | NRS | LIA had low NRS |
| Paul JE et al., | [17] | 80 patients for TKR | NRS | FNB had low NRS |
| Kurosaka et al., | [18] | 45 patients for TKA | NRS | LIA had lower NRS |
| Present study | | 60 patients for TKR | NRS | FNB had low NRS |
In our study, muscle power was better in LIA although early mobilization time was affected in LIA Group which was statistically significant (p-value<0.001) which may be because of high NRS in LIA Group. However, muscle power was better in LIA Group as compared to FNB Group. Free mobilization were affected in both group with no statistical significant difference (p<0.79). Toftdahl K and collaborators presented data suggesting that LIA with ropivacaine, ketorolac, and epinephrine results in faster postoperative activation, as indicated by being better able to walk on the first postoperative day as compared to femoral block [16]. Carli F et al., have conducted study in which Group FNB used less PCA (p=0.02) to achieve adequate analgesia although postoperative two minutes Walking Test was similar in both groups (p=0.27) [10].
This study categorised rescue analgesia into four groups according to their demand in a day less than five times, 6-10 times, 11-15 times, 16-20 times. Only seven patients (23%) of FNB Group had so less demand (less than five times). In LIA Group, 19 patients (63%) had so high requirement (more than 16 times). We have concluded that the rescue analgesia requirement was remarkably low in FNB Group. Carli F et al., and Paul JE et al., have shown that FNB had remarkable decrease in opioids dose [10,17].
In our study, we found that sedation score was higher in LIA Group which may be correlated with fentanyl dose which was also higher in LIA Group.
Number of night stay in our hospital is 10 days for every patient so we could not be able to calculate the duration of night stay.
Limitation
The limitation of study was that drain was present in every surgery. The patient has fixed package of duration of stay so we were not able to assess the number of night stay.
Conclusion
FNB group has better pain relief but range of motion was reduced. Grossly effect on mobilisation was comparable in both the group.
p-value <0.05 is significant; NS - non significant; S - significant. Independent t test used
*Significant values, Chi-square test used
Chi-square test used
Chi-square test used
Chi-square test used
Chi-square test used